J Gastric Cancer.
2016 Sep;16(3):195-199. 10.5230/jgc.2016.16.3.195.
Phlegmonous Gastritis with Early Gastric Cancer
- Affiliations
-
- 1Center for Gastric Cancer, National Cancer Center, Goyang, Korea. glse@ncc.re.kr
- 2Emergency Department, National Cancer Center, Goyang, Korea.
- KMID: 2372564
- DOI: http://doi.org/10.5230/jgc.2016.16.3.195
Abstract
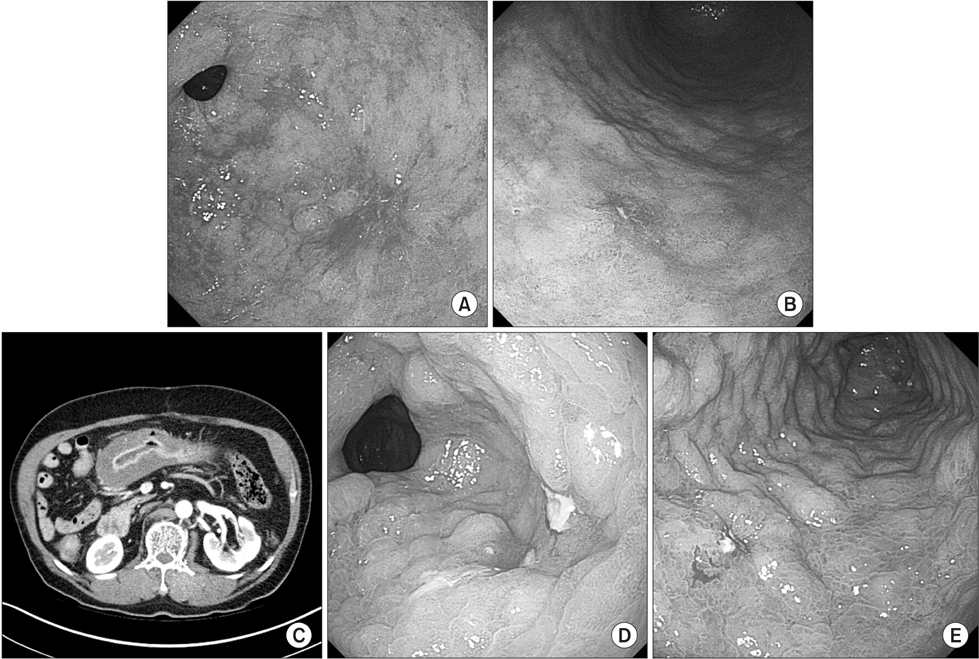
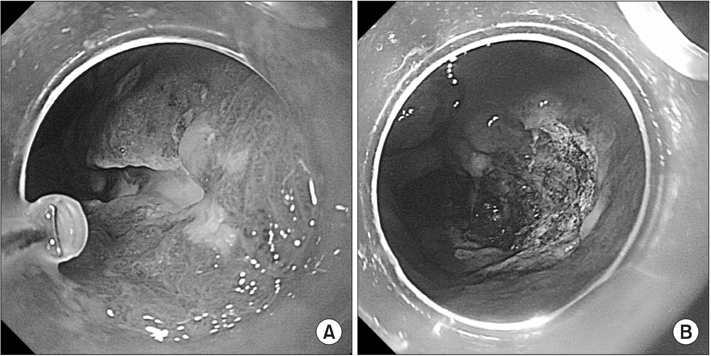
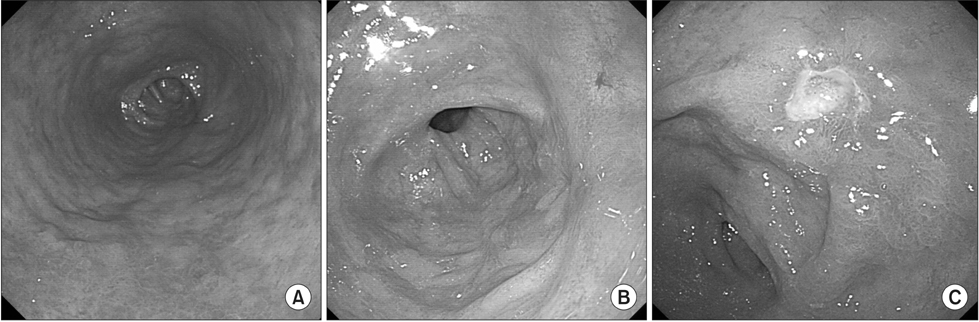
- Phlegmonous gastritis is a rare and rapidly progressive bacterial infection of the stomach wall, with a high mortality rate. Antibiotics with or without surgical treatment are required for treatment. We present a case in which phlegmonous gastritis occurred during the diagnostic evaluation of early gastric cancer. The patient showed improvement after antibiotic treatment, but attempted endoscopic submucosal dissection failed because of submucosal pus. We immediately applied argon plasma coagulation since surgical resection was also considered a high-risk procedure because of the submucosal pus and multiple comorbidities. However, there was local recurrence two years later, and the patient underwent subtotal gastrectomy with lymph node dissection. Considering the risk of incomplete treatment immediately after recovery from phlegmonous gastritis and that recurrent disease can be more difficult to manage, delaying treatment and evaluation until after complete recovery of PG might be a better option in this particular clinical situation.
MeSH Terms
Figure
Reference
-
1. Starr A, Wilson JM. Phlegmonous gastritis. Ann Surg. 1957; 145:88–93.2. Iwakiri Y, Kabemura T, Yasuda D, Okabe H, Soejima A, Miyagahara T, et al. A case of acute phlegmonous gastritis successfully treated with antibiotics. J Clin Gastroenterol. 1999; 28:175–177.3. Rada-Palomino A, Muñoz-Duyos A, Pérez-Romero N, Vargas-Pierola H, Puértolas-Rico N, Ruiz-Campos L, et al. Phlegmonous gastritis: a rare entity as a differential diagnostic of an acute abdomen. Description of a case and a bibliographic review. Rev Esp Enferm Dig. 2014; 106:418–424.4. Jung SJ, Cho SJ, Choi IJ, Kook MC, Kim CG, Lee JY, et al. Argon plasma coagulation is safe and effective for treating smaller gastric lesions with low-grade dysplasia: a comparison with endoscopic submucosal dissection. Surg Endosc. 2013; 27:1211–1218.5. Min SY, Kim YH, Park WS. Acute phlegmonous gastritis complicated by delayed perforation. World J Gastroenterol. 2014; 20:3383–3387.6. Kim NY, Park JS, Lee KJ, Yun HK, Kim JS. A case of acute phlegmonous gastritis causing gastroparesis and cured with medical treatment alone. Korean J Gastroenterol. 2011; 57:309–314.7. Wakayama T, Watanabe H, Ishizaki Y, Okuyama T, Ogata H, Tanigawa K, et al. A case of phlegmonous esophagitis associated with diffuse phlegmonous gastritis. Am J Gastroenterol. 1994; 89:804–806.8. Kim GY, Ward J, Henessey B, Peji J, Godell C, Desta H, et al. Phlegmonous gastritis: case report and review. Gastrointest Endosc. 2005; 61:168–174.9. Nicholson BW, Maull KI, Scher LA. Phlegmonous gastritis: clinical presentation and surgical management. South Med J. 1980; 73:875–877.10. Morimoto M, Tamura S, Hayakawa T, Yamanishi H, Nakamoto C, Nakamoto H, et al. Phlegmonous gastritis associated with group A streptococcal toxic shock syndrome. Intern Med. 2014; 53:2639–2642.11. Miller AI, Smith B, Rogers AI. Phlegmonous gastritis. Gastroenterology. 1975; 68:231–238.12. Saito M, Morioka M, Kanno H, Tanaka S. Acute phlegmonous gastritis with neutropenia. Intern Med. 2012; 51:2987–2988.13. Corti M, Metta H, Palmieri O, Schtirbu R. Acute phlegmonous gastritis in a patient with AIDS. Enferm Infecc Microbiol Clin. 2007; 25:218–220.14. Ajibe H, Osawa H, Yoshizawa M, Yamamoto H, Satoh K, Koinuma K, et al. Phlegmonous gastritis after endoscopic submucosal dissection for early gastric cancer. Therap Adv Gastroenterol. 2008; 1:91–95.15. Itonaga M, Ueda K, Ichinose M. Phlegmonous gastritis caused by endoscopic ultrasound-guided fine-needle aspiration (EUSFNA). Dig Endosc. 2012; 24:488.16. Lee BS, Kim SM, Seong JK, Kim SH, Jeong HY, Lee HY, et al. Phlegmonous gastritis after endoscopic mucosal resection. Endoscopy. 2005; 37:490–493.17. Avilés JF, Fernández-Seara J, Bárcena R, Domíinguez F, Fernández C, Ledo L. Localized phlegmonous gastritis: endoscopic view. Endoscopy. 1988; 20:38–39.18. Sood BP, Kalra N, Suri S. CT features of acute phlegmonous gastritis. Clin Imaging. 2000; 24:287–288.19. Park CW, Kim A, Cha SW, Jung SH, Yang HW, Lee YJ, et al. A case of phlegmonous gastritis associated with marked gastric distension. Gut Liver. 2010; 4:415–418.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acute Phlegmonous Gastritis Diagnosed Early Endoscopically and Treated Successfully with Antibiotics
- Acute Phlegmonous Gastritis Developing after Endoscopic Submucosal Dissection That Was Successfully Treated by Antibiotics Alone
- Infectious Gastric Diseases Other than Helicobacter
- A Case of Phlegmonous Gastritis Associated with Marked Gastric Distension
- Two Cases of Acute Phlegmonous Gastritis