J Gastric Cancer.
2013 Mar;13(1):65-68.
Perforated Early Gastric Cancer: Uncommon and Easily Missed a Case Report and Review of Literature
- Affiliations
-
- 1Department of Surgery, Singapore National University Hospital, Singapore. cfsasim@nus.edu.sg
- 2Yong Loo Lin School of Medicine, National University of Singapore, Singapore.
- 3Department of Pathology, Singapore National University Hospital, Singapore.
Abstract
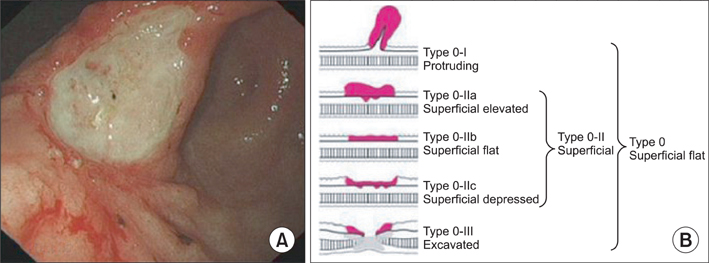
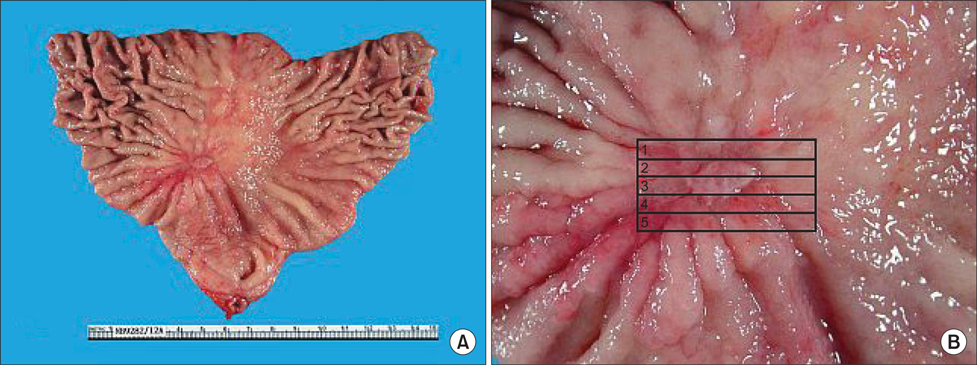
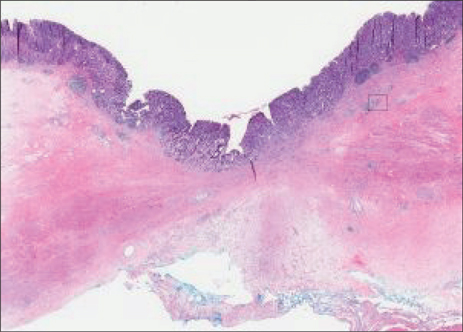
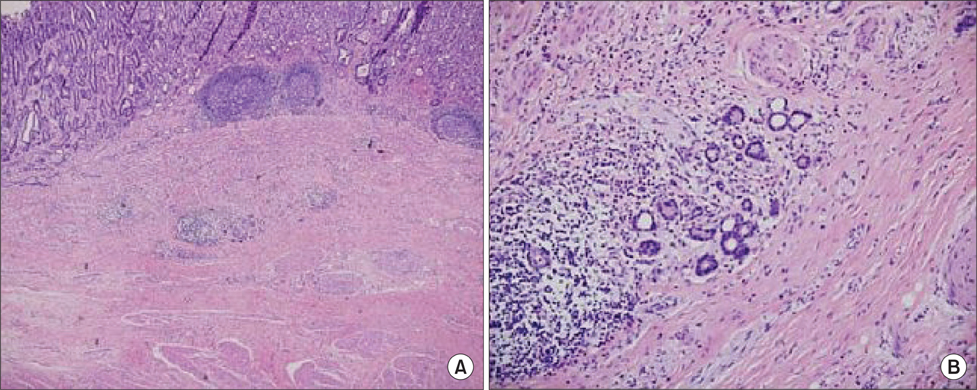
- Gastric carcinoma rarely presents as a perforation, but when it does, is perceived as advanced disease. The majority of such perforations are Stage III/IV disease. A T1 gastric carcinoma has never been reported to perforate spontaneously in English literature. We present a 56 year-old Chinese male who presented with a perforated gastric ulcer. Intra-operatively, there was no suspicion of malignancy. At operation, an open omental patch repair was performed. Post-operative endoscopy revealed a macroscopic Type 0~III tumour and from the ulcer edge biopsy was reported as adenocarcinoma. Subsequently, the patient underwent open subtotal gastrectomy and formal D2 lymphadenectomy. The final histopathology report confirms T1b N0 disease. The occurrence of a perforated early gastric cancer re-emphasises the need for vigilance, including intra-operative frozen section and/or biopsy, as well as routine post-operative endoscopy for all patients.
MeSH Terms
Figure
Reference
-
1. Adachi Y, Mori M, Maehara Y, Matsumata T, Okudaira Y, Sugimachi K. Surgical results of perforated gastric carcinoma: an analysis of 155 Japanese patients. Am J Gastroenterol. 1997. 92:516–518.2. Roviello F, Rossi S, Marrelli D, De Manzoni G, Pedrazzani C, Morgagni P, et al. Perforated gastric carcinoma: a report of 10 cases and review of the literature. World J Surg Oncol. 2006. 4:19.
Article3. Mahar AL, Brar SS, Coburn NG, Law C, Helyer LK. Surgical management of gastric perforation in the setting of gastric cancer. Gastric Cancer. 2012. 15:Suppl 1. S146–S152.
Article4. Kitakado Y, Tanigawa N, Muraoka R. A case report of perforated early gastric cancer. Nihon Geka Hokan. 1997. 66:86–90.5. Gertsch P, Yip SK, Chow LW, Lauder IJ. Free perforation of gastric carcinoma. Results of surgical treatment. Arch Surg. 1995. 130:177–181.6. Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011. 14:101–112.7. So JB, Yam A, Cheah WK, Kum CK, Goh PM. Risk factors related to operative mortality and morbidity in patients undergoing emergency gastrectomy. Br J Surg. 2000. 87:1702–1707.
Article8. Miura T, Ishii T, Shimoyama T, Hirano T, Tomita M. Surgical treatment of perforated gastric cancer. Dig Surg. 1985. 2:200–204.
Article9. Cuschieri A, Weeden S, Fielding J, Bancewicz J, Craven J, Joypaul V, et al. Patient survival after D1 and D2 resections for gastric cancer: long-term results of the MRC randomized surgical trial. Surgical Co-operative Group. Br J Cancer. 1999. 79:1522–1530.
Article10. Tan KK, Quek TJ, Wong N, Li KK, Lim KH. Emergency surgery for perforated gastric malignancy: an institution's experience and review of the literature. J Gastrointest Oncol. 2011. 2:13–18.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Perforated Early Gastric Cancer: A case report
- A Case of Early Gastric Cancer in Childhood
- Esophagus, Stomach & Intestine; One Case of Early Gastric Stump Cancer Following Partial Gastrectomy for Gastroptosis
- A Case of Perforated Stomach Cancer with Placental Abruption in Pregnancy
- Screening of gastric cancer