Hip Pelvis.
2017 Mar;29(1):35-43. 10.5371/hp.2017.29.1.35.
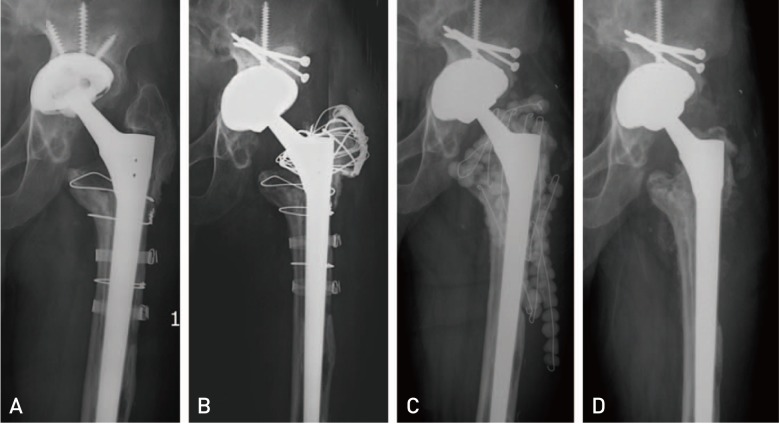
Acute Delayed or Late Infection of Revision Total Hip Arthroplasty Treated with Debridement/Antibiotic-loaded Cement Beads and Retention of the Prosthesis
- Affiliations
-
- 1Department of Orthopedic Surgery, Dongtan Sacred Heart Hospital, Hallym University School of Medicine, Hwaseong, Korea.
- 2Department of Orthopedic Surgery, Chuncheon Sacred Heart Hospital, Hallym University School of Medicine, Chuncheon, Korea.
- 3Department of Orthopedic Surgery, Hallym University Sacred Heart Hospital, Hallym University School of Medicine, Anyang, Korea. oships@hallym.ac.kr
- KMID: 2371766
- DOI: http://doi.org/10.5371/hp.2017.29.1.35
Abstract
- PURPOSE
The treatment of infected revision total hip arthroplasty (THA) is very challenging due to retained revision prosthesis, poor bone stock and soft tissue condition derived from previous revision surgeries, and comorbidities. The purpose of this study was to investigate the effectiveness and short-term outcomes of aggressive debridement and use of antibiotic-loaded cement beads with retention of the prosthesis for acute delayed or late infection of revision THAs.
MATERIALS AND METHODS
Ten consecutive patients with symptoms or signs of less than one-week evolution and well-fixed prostheses, were treated with this procedure and a postoperative course of organism-specific antibiotics for a minimum of 6 weeks. All hips presented with acute delayed or late infection of revision THAs. Patients with a mean age of 68.1 years (range, 59-78 years) underwent an average of 1.9 previous revision THAs (1-4) before the index surgery. The minimal follow-up was 2 years with a mean of 46.2 months (range, 24-64 months).
RESULTS
There were 8 cures (80.0%) and 2 failures with no mortality during the study period. The 2 failures involved the same and resistant bacteria implicated in the primary infection (methicillin-resistant Staphylococcus aureus and Prevotella oralis, respectively). The mean Harris hip score was 65.2 (range, 26-83) and the mean visual analogue scale was 2.6 (range, 1-4) at final follow-up.
CONCLUSION
With a favorable success rate and no mortality, our procedure may be considered a safe and effective alternative for the treatment of acute delayed or late infection of revision THAs with well-fixed prostheses.
Keyword
MeSH Terms
Figure
Reference
-
1. Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005; 87:1487–1497. PMID: 15995115.
Article2. Bozic KJ, Ries MD. The impact of infection after total hip arthroplasty on hospital and surgeon resource utilization. J Bone Joint Surg Am. 2005; 87:1746–1751. PMID: 16085614.
Article3. Hanssen AD, Rand JA. Evaluation and treatment of infection at the site of a total hip or knee arthroplasty. Instr Course Lect. 1999; 48:111–122. PMID: 10098033.4. Salvati EA, González Della, Masri BA, Duncan CP. The infected total hip arthroplasty. Instr Course Lect. 2003; 52:223–245. PMID: 12690851.5. Sanchez-Sotelo J, Berry DJ, Hanssen AD, Cabanela ME. Midterm to long-term followup of staged reimplantation for infected hip arthroplasty. Clin Orthop Relat Res. 2009; 467:219–224. PMID: 18813895.
Article6. Spangehl MJ, Younger AS, Masri BA, Duncan CP. Diagnosis of infection following total hip arthroplasty. Instr Course Lect. 1998; 47:285–295. PMID: 9571430.7. Hanssen AD, Spangehl MJ. Treatment of the infected hip replacement. Clin Orthop Relat Res. 2004; (420):63–71.
Article8. Parvizi J, Gehrke T, Chen AF. Proceedings of the international consensus on periprosthetic joint infection. Bone Joint J. 2013; 95-B:1450–1452. PMID: 24151261.
Article9. Tsukayama DT, Estrada R, Gustilo RB. Infection after total hip arthroplasty. A study of the treatment of one hundred and six infections. J Bone Joint Surg Am. 1996; 78:512–523. PMID: 8609130.
Article10. Zimmerli W, Trampuz A, Ochsner PE. Prosthetic-joint infections. N Engl J Med. 2004; 351:1645–1654. PMID: 15483283.
Article11. Kim YH, Kim JS, Park JW, Joo JH. Cementless revision for infected total hip replacements. J Bone Joint Surg Br. 2011; 93:19–26. PMID: 21196538.
Article12. Aboltins CA, Page MA, Buising KL, et al. Treatment of staphylococcal prosthetic joint infections with debridement, prosthesis retention and oral rifampicin and fusidic acid. Clin Microbiol Infect. 2007; 13:586–591. PMID: 17331125.
Article13. Cataldo MA, Petrosillo N, Cipriani M, Cauda R, Tacconelli E. Prosthetic joint infection: recent developments in diagnosis and management. J Infect. 2010; 61:443–448. PMID: 20932998.
Article14. Mirra JM, Amstutz HC, Matos M, Gold R. The pathology of the joint tissues and its clinical relevance in prosthesis failure. Clin Orthop Relat Res. 1976; (117):221–240. PMID: 776484.
Article15. Berend KR, Lombardi AV Jr, Morris MJ, Bergeson AG, Adams JB, Sneller MA. Two-stage treatment of hip periprosthetic joint infection is associated with a high rate of infection control but high mortality. Clin Orthop Relat Res. 2013; 471:510–518. PMID: 22983683.
Article16. Ekpo TE, Berend KR, Morris MJ, Adams JB, Lombardi AV Jr. Partial two-stage exchange for infected total hip arthroplasty: a preliminary report. Clin Orthop Relat Res. 2014; 472:437–448. PMID: 23852737.
Article17. Oussedik SI, Dodd MB, Haddad FS. Outcomes of revision total hip replacement for infection after grading according to a standard protocol. J Bone Joint Surg Br. 2010; 92:1222–1226. PMID: 20798438.
Article18. Toulson C, Walcott-Sapp S, Hur J, et al. Treatment of infected total hip arthroplasty with a 2-stage reimplantation protocol: update on “our institution's” experience from 1989 to 2003. J Arthroplasty. 2009; 24:1051–1060. PMID: 18848425.19. Engesaeter LB, Dale H, Schrama JC, Hallan G, Lie SA. Surgical procedures in the treatment of 784 infected THAs reported to the Norwegian Arthroplasty Register. Acta Orthop. 2011; 82:530–537. PMID: 21992085.20. Estes CS, Beauchamp CP, Clarke HD, Spangehl MJ. A twostage retention débridement protocol for acute periprosthetic joint infections. Clin Orthop Relat Res. 2010; 468:2029–2038. PMID: 20224958.
Article21. Tattevin P, Crémieux AC, Pottier P, Huten D, Carbon C. Prosthetic joint infection: when can prosthesis salvage be considered? Clin Infect Dis. 1999; 29:292–295. PMID: 10476729.
Article22. Meehan AM, Osmon DR, Duffy MC, Hanssen AD, Keating MR. Outcome of penicillin-susceptible streptococcal prosthetic joint infection treated with debridement and retention of the prosthesis. Clin Infect Dis. 2003; 36:845–849. PMID: 12652384.
Article23. Marculescu CE, Berbari EF, Hanssen AD, et al. Outcome of prosthetic joint infections treated with debridement and retention of components. Clin Infect Dis. 2006; 42:471–478. PMID: 16421790.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Staged Revision of Infected Hip Arthroplasty Using an Antibiotics-Loaded Intra-Articular Cement Spacer with Retention of the Stem
- The Treatment of Infected Total Hip Arthroplasty: Report of 12 Cases
- Efficacy of Debridement for Early Periprosthetic Joint Infection after Hip Arthroplasty
- Management of Periprosthetic Hip Joint Infection
- Treatment of Infected Hip Arthroplasty with Antibiotic-Impregnated Calcium Sulfate Cement