Neurointervention.
2017 Mar;12(1):40-44. 10.5469/neuroint.2017.12.1.40.
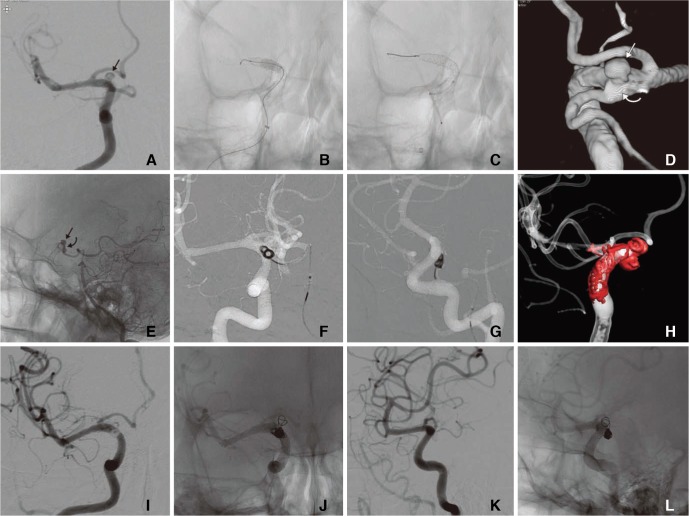
A Case of Ruptured Blood Blister-like Aneurysm Treated with Pipeline Embolization Device: Clinical Significance of Fetal-type Posterior Communicating Artery
- Affiliations
-
- 1Department of Neurosurgery, Chung-Ang University College of Medicine, Seoul, Korea.
- 2Department of Neurosurgery, Kyungpook National University School of Medicine, Daegu, Korea. kdhdock@hotmail.com
- 3Department of Radiology, Kyungpook National University School of Medicine, Daegu, Korea.
- 4Department of Radiology, Younsei University College of Medicine, Seoul, South, Korea.
- KMID: 2371757
- DOI: http://doi.org/10.5469/neuroint.2017.12.1.40
Abstract
- Blood-blister like aneurysms (BBAs) are challenging lesions because of their wide fragile neck. Flow-diverting stents (FDSs), such as the Pipeline Embolization Device (PED), have been applied to treat BBAs less amenable to more established techniques of treatment. However, the use of FDSs, including the PED, in acute subarachnoid hemorrhage (SAH) still remains controversial. We report a case of aneurysm regrowth following PED application for a ruptured BBA that overlapped the origin of the dominant posterior communicating artery (PCoA), which was successfully treated after coil trapping of the origin of the fetal-type PCoA. And, we discuss the clinical significance of the fetal-type PCoA communicating with a BBA in terms of PED failure.
Keyword
Figure
Reference
-
1. Park J. Blood blister-like aneurysm with rupture point close to origin of anterior choroidal artery. J Korean Neurosurg Soc. 2014; 56:500–503. PMID: 25628811.
Article2. Nerva JD, Morton RP, Levitt MR, Osbun JW, Ferreira MJ, Ghodke BV, et al. Pipeline Embolization Device as primary treatment for blister aneurysms and iatrogenic pseudoaneurysms of the internal carotid artery. J Neurointerv Surg. 2015; 7:210–216. PMID: 24578484.
Article3. Nakagawa F, Kobayashi S, Takemae T, Sugita K. Aneurysms protruding from the dorsal wall of the internal carotid artery. J Neurosurg. 1986; 65:303–308. PMID: 3734880.
Article4. Kojima M, Irie K, Fukuda T, Arai F, Hirose Y, Negoro M. The study of flow diversion effects on aneurysm using multiple enterprise stents and two flow diverters. Asian J Neurosurg. 2012; 7:159–165. PMID: 23559981.
Article5. McAuliffe W, Wenderoth JD. Immediate and midterm results following treatment of recently ruptured intracranial aneurysms with the Pipeline embolization device. AJNR Am J Neuroradiol. 2012; 33:487–493. PMID: 22135131.
Article6. Cruz JP, O'Kelly C, Kelly M, Wong JH, Alshaya W, Martin A, et al. Pipeline embolization device in aneurysmal subarachnoid hemorrhage. AJNR Am J Neuroradiol. 2013; 34:271–276. PMID: 23064594.
Article7. Cebral JR, Mut F, Raschi M, Scrivano E, Ceratto R, Lylyk P, et al. Aneurysm rupture following treatment with flow-diverting stents: computational hemodynamics analysis of treatment. AJNR Am J Neuroradiol. 2011; 32:27–33. PMID: 21071533.
Article8. Turowski B, Macht S, Kulcsar Z, Hanggi D, Stummer W. Early fatal hemorrhage after endovascular cerebral aneurysm treatment with a flow diverter (SILK-Stent): do we need to rethink our concepts? Neuroradiology. 2011; 53:37–41. PMID: 20339842.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Double-Balloon-Assisted Coiling for Wide-Necked Posterior Communicating Artery Aneurysms with a Fetal-Type Variant of the Posterior Cerebral Artery: A Case Series
- Treatment of a Ruptured Vertebrobasilar Fusiform Aneurysm Using Pipeline Embolization Device
- The Use of a Pipeline Embolization Device for Treatment of a Ruptured Dissecting Middle Cerebral Artery M3/M4 Aneurysm: Challenges and Technical Considerations
- Rupture of Giant Posterior Communicating Artery Aneurysm During Carotid Angiography: A Case Report
- Ventriculoperitoneal Shunt in a Patient with Ruptured Blister Aneurysm Treated with Pipeline Embolization Device