Korean J Crit Care Med.
2016 Nov;31(4):317-323. 10.4266/kjccm.2016.00703.
Surveillance of Extended-Spectrum β-Lactamase-producing Enterobacteriaceae Carriage in a Japanese Intensive Care Unit: a Retrospective Analysis
- Affiliations
-
- 1Department of Emergency and Critical Care Medicine, Fukuoka University Hospital, Fukuoka, Japan. kawano0301@cis.fukuoka-u.ac.jp
- 2Division of Medical Oncology, Hematology, and Infectious Diseases, Department of Medicine, Fukuoka University Hospital, Fukuoka, Japan.
- KMID: 2371187
- DOI: http://doi.org/10.4266/kjccm.2016.00703
Abstract
- BACKGROUND
The effectiveness of surveillance to identify extended-spectrum beta-lactamase-producing Enterobacteriaceae (ESBL-E) carriers is controversial during a non-outbreak situation. We performed additional stool cultures for ESBL-E among intensive care unit (ICU) patients already under active surveillance by means of sputum and urine cultures. We aimed to assess the efficacy of stool cultures for screening for ESBL-E in a non-outbreak situation.
METHODS
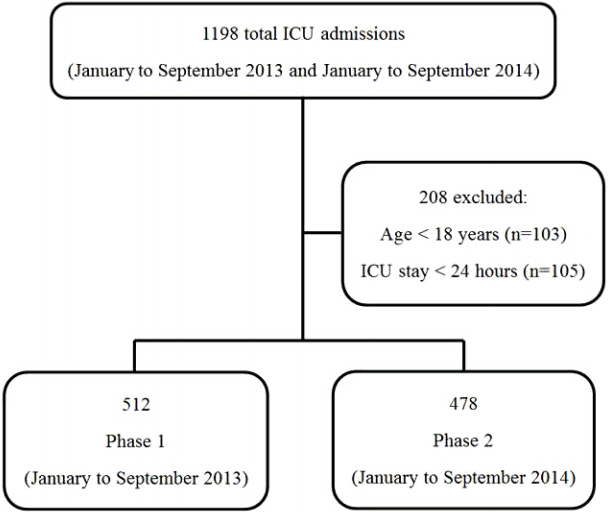
We conducted a retrospective cohort study in an ICU. Sputum and urine samples were cultured for ESBL-E surveillance purposes from January to September 2013 (phase 1). Stool cultures were routinely performed in addition from January to September 2014 (phase 2). Antimicrobial use density values and clinical outcomes were investigated and compared between phase 1 and 2.
RESULTS
We identified 512 and 478 patients in phase 1 and phase 2, respectively. ESBL-E were found in the feces of 65 (13.6%) patients in phase 2. The antimicrobial use density values (expressed as defined daily doses per 1,000 bed-days) were not significantly different between the two phases for fluoroquinolones (7 vs. 10, p = 0.376), third-generation cephalosporins (24.2 vs. 29.5, p = 0.724), tazobactam/piperacillin (44.6 vs. 57.3, p = 0.489), and carbapenems (73 vs. 55.5, p = 0.222). Moreover, there were no significant differences in ICU mortality and length of stay (11.5% vs. 9.8%, p = 0.412, and 9 vs. 10 days, p = 0.28, respectively).
CONCLUSIONS
Stool culture seemed ineffective in improving the antimicrobial use density of broad-spectrum antimicrobials, clinical outcomes, and ICU length of stay, and is not recommended for surveillance of ESBL-E in a non-outbreak situation.
Keyword
MeSH Terms
-
Asian Continental Ancestry Group*
beta-Lactamases
Carbapenems
Cephalosporins
Cohort Studies
Critical Care*
Disease Outbreaks
Enterobacteriaceae*
Epidemiology
Feces
Fluoroquinolones
Humans
Intensive Care Units*
Length of Stay
Mass Screening
Mortality
Retrospective Studies*
Sputum
Carbapenems
Cephalosporins
Fluoroquinolones
beta-Lactamases
Figure
Reference
-
References
1. Tumbarello M, Spanu T, Sanguinetti M, Citton R, Montuori E, Leone F, et al. Bloodstream infections caused by extended-spectrum-beta-lactamase-producing Klebsiella pneumoniae: risk factors, molecular epidemiology, and clinical outcome. Antimicrob Agents Cemother. 2006; 50:498–504.2. Thouverez M, Talon D, Bertrand X. Control of enterobacteriaceae producing extended-spectrum beta-lactamase in intensive care units: rectal screening may not be needed in non-epidemic situations. Infec Control Hosp Epidemiol. 2004; 25:838–41.
Article3. Han JH, Bilker WB, Nachamkin I, Zaoutis TE, Coffin SE, Linkin DR, et al. The effect of a hospitalwide urine culture screening intervention on the incidence of extended-spectrum β-lactamase-producing Escherichia coli and Klebsiella species. Infec Control Hosp Epidemiol. 2013; 34:1160–6.4. Troché G, Joly LM, Guibert M, Zazzo JF. Detection and treatment of antibiotic-resistant bacterial carriage in a surgical intensive care unit: a 6-year prospective survey. Infect Control Hosp Epidemiol. 2005; 26:161–5.
Article5. Liss BJ, Vehreschild JJ, Cornely OA, Hallek M, Fätkenheuer G, Wisplinghoff H, et al. Intestinal colonisation and blood stream infections due to vancomycin-resistant enterococci (VRE) and extended-spectrum beta-lactamase-producing Enterobacteriaceae (ESBLE) in patients with haematological and oncological malignancies. Infection. 2012; 40:613–9.
Article6. Blot S, Depuydt P, Vogelaers D, Decruyenaere J, De Waele J, Hoste E, et al. Colonization status and appropriate antibiotic therapy for nosocomial bacteremia caused by antibiotic-resistant gram-negative bacteria in an intensive care unit. Infect Control Hosp Epidemiol. 2005; 26:575–9.
Article7. Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing; Nineteenth informational supplement. CLSI document M100-S19. Wayne: Clinical and Laboratory Standards Institute;2009.8. The WHO Collaborating Centre for Drug Statistics Methodology. Guidelines for ATC classification and DDD assignment 2016 [Internet]. Oslo: WHO Collaborating Centre for Drug Statistics Methodology;c2016. [accessed on 20 May 2016]. Available from: http://www.whocc.no/atcddd/.9. Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013; 48:452–8.
Article10. Tamma PD, Han JH, Rock C, Harris AD, Lautenbach E, Hsu AJ, et al. Carbapenem therapy is associated with improved survival compared to piperacillin-tazobactam for patients with extended-spectrum β-lactamase bacteremia. Clin Infect Dis. 2015; 60:1319–25.11. Harris AD, McGregor JC, Johnson JA, Strauss SM, Moore AC, Standiford HC, et al. Risk factors for colonization with extended-spectrum β-lactamase-producing bacteria and intensive care unit admission. Emerg Infect Dis. 2007; 13:1144–9.
Article12. Azim A, Dwivedi M, Rao PB, Baronia AK, Singh RK, Prasad KN, et al. Epidemiology of bacterial colonization at intensive care unit admission with emphasis on extended-spectrum beta-lactamase- and metallo-beta-lactamase-producing Gram-negative bacteria--an Indian experience. J Med Microbiol. 2010; 59(Pt 8):955–60.13. Sidler JA, Battegay M, Tschudin-Sutter S, Widmer AF, Weisser M. Enterococci, Clostridium difficile and ESBL-producing bacteria: epidemiology, clinical impact and prevention in ICU patients. Swiss Med Wkly. 2014; 144:w14009.
Article14. Luvsansharav UO, Hirai I, Niki M, Nakata A, Yoshinaga A, Moriyama T, et al. Prevalence of fecal carriage of extended-spectrum β-lactamase-producing Enterobacteriaceae among healthy adult people in Japan. J Infect Chemother. 2011; 17:722–5.
Article15. Minami K, Shoji Y, Kasai M, Ogiso Y, Nakamura T, Kawakami Y, et al. Proportion of rectal carriage of extended-spectrum β-lactamase-producing Enterobacteriaceae in the inpatients of a pediatric tertiary care hospital in Japan. Jpn J Infect Dis. 2012; 65:548–50.16. Valverde A, Coque TM, Sánchez-Moreno MP, Rollán A, Baquero F, Cantón R. Dramatic increase in prevalence of fecal carriage of extended-spectrum beta-lactamase-producing Enterobacteriaceae during nonoutbreak situations in Spain. J Clin Microbiol. 2004; 42:4769–75.17. Malloy AM, Campos JM. Extended-spectrum beta-lactamases: a brief clinical update. Pediatr Infect Dis J. 2011; 30:1092–3.18. Ajao AO, Johnson JK, Harris AD, Zhan M, McGregor JC, Thom KA, et al. Risk of acquiring extended-spectrum β-lactamase-producing Klebsiella species and Escherichia coli from prior room occupants in the intensive care unit. Infect Control Hosp Epidemiol. 2013; 34:453–8.19. Razazi K, Derde LP, Verachten M, Legrand P, Lesprit P, Brun-Buisson C. Clinical impact and risk factors for colonization with extended-spectrum β-lactamase-producing bacteria in the intensive care unit. Intensive Care Med. 2012; 38:1769–78.
Article20. Christiaens G, Ciccarella Y, Damas P, Hayette MP, Melin P, Nys M, et al. Prospective survey of digestive tract colonization with enterobacteriaceae that produce extended-spectrum beta-lactamases in intensive care units. J Hosp Infect. 2006; 62:386–8.21. Titelman E, Hasan CM, Iversen A, Nauclér P, Kais M, Kalin M, et al. Faecal carriage of extended-spectrum β-lactamase-producing Enterobacteriaceae is common 12 months after infection and is related to strain factors. Clin Microbiol Infect. 2014; 20:O508–15.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevalence and Risk Factors for Extended-Spectrum β-Lactamase-Producing Klebsiella pneumoniae Colonization in Intensive Care Units
- Two Cases of Neonatal Osteomyelitis due to Extended Spectrum beta-lactamase Producing Klebsiella pneumoniae
- Prevalence of Fecal Carriage of CTX-M-15 Beta-Lactamase-Producing Escherichia coli in Healthy Children from a Rural Andean Village in Venezuela
- Clinical Significance of Extended-spectrum β-lactamase-producing Bacteria in First Pediatric Febrile Urinary Tract Infections and Differences between Age Groups
- Antibiotic-Resistant Gram-negative Bacteria Carriage in Healthcare Workers Working in an Intensive Care Unit