Korean J Crit Care Med.
2017 Feb;32(1):1-8. 10.4266/kjccm.2016.00955.
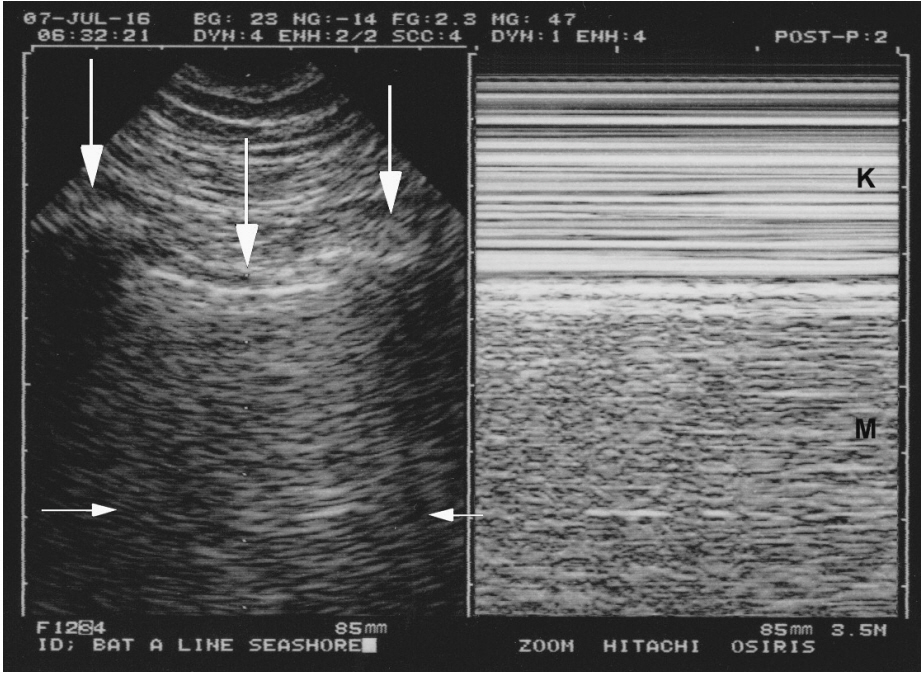
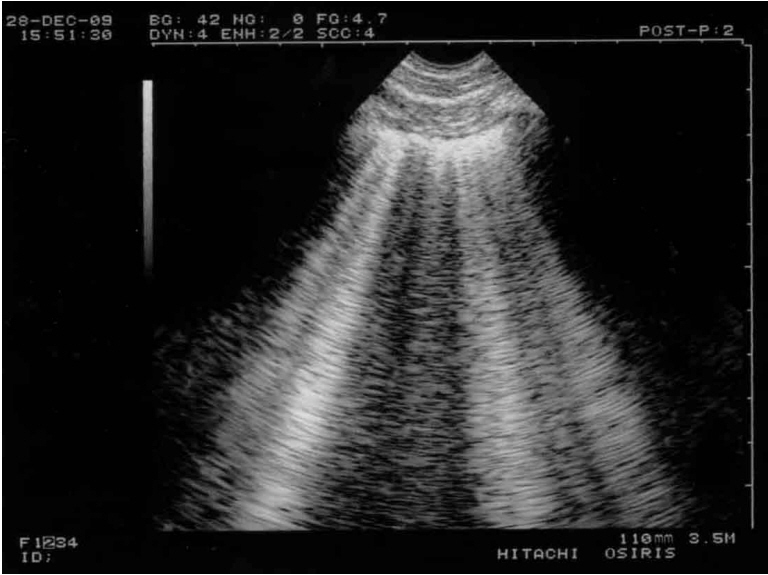
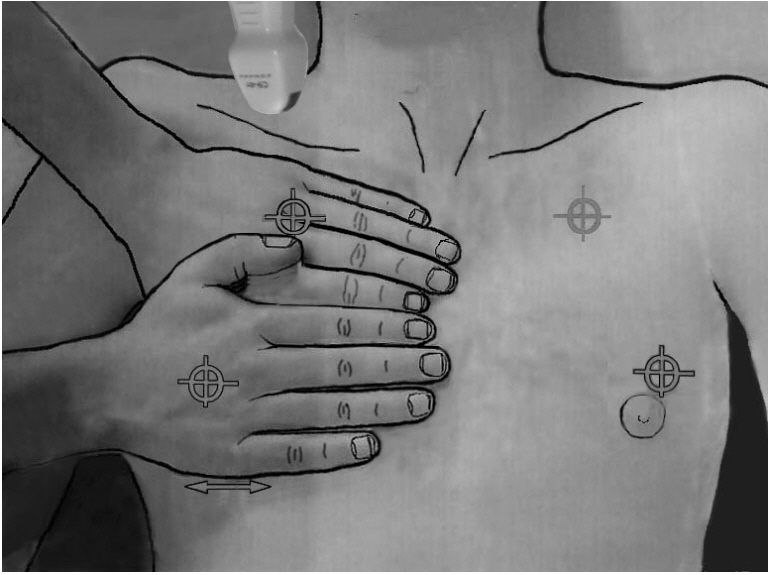
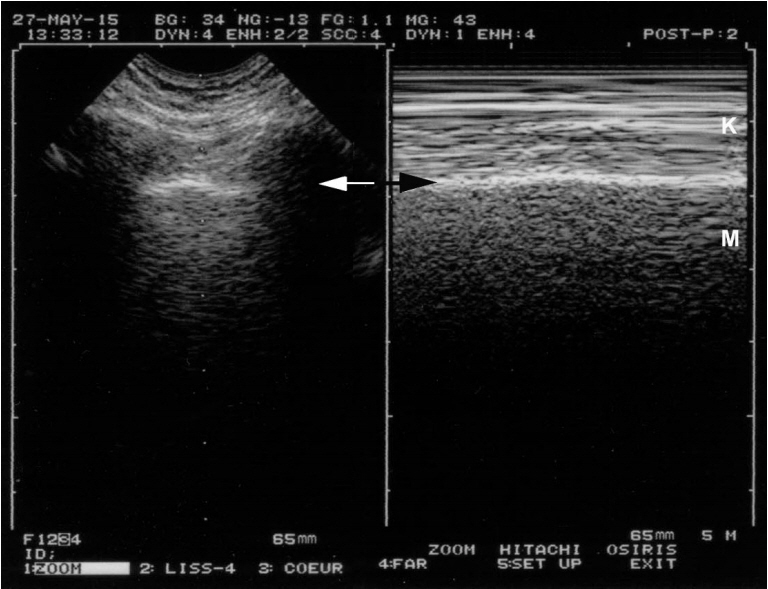
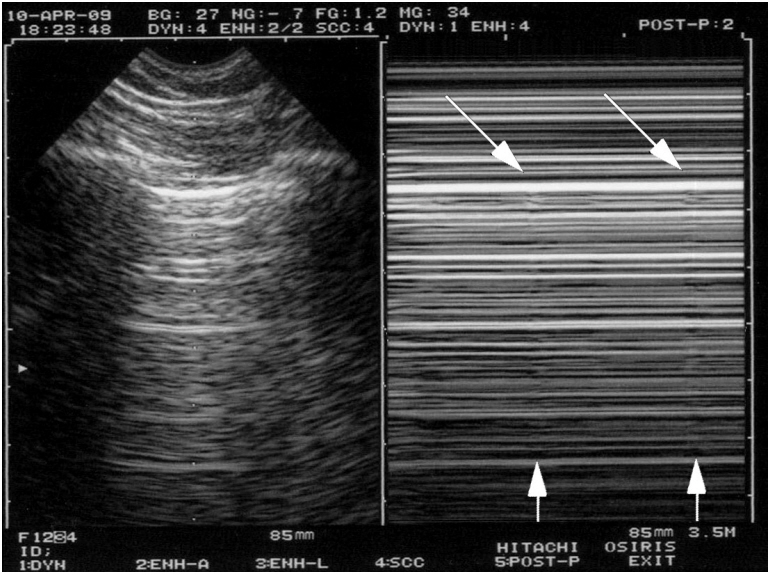
Lung Ultrasound (in the Critically Ill) Superior to CT: the Example of Lung Sliding
- Affiliations
-
- 1Hôpital Ambroise-Paré (Medical ICU), Paris-Ouest university, Boulogne, France. D.Licht@free.fr
- KMID: 2371148
- DOI: http://doi.org/10.4266/kjccm.2016.00955
Abstract
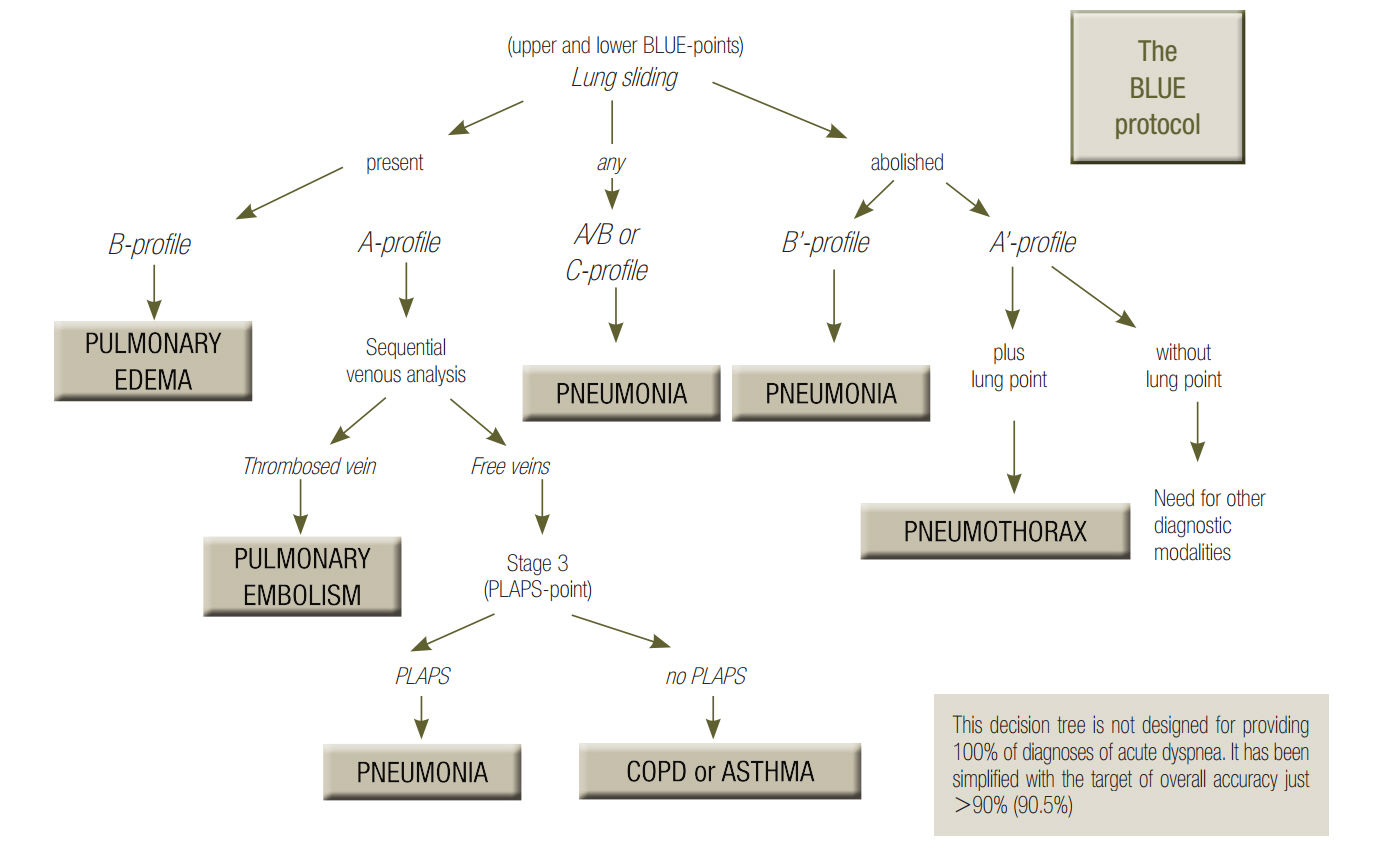
- This review article shows the potential of lung ultrasound in the critically ill (LUCI) to study lung sliding and describes the optimal equipment for its assessment. Then, it analyses the integration of lung sliding within lung ultrasound then whole body critical ultrasound. It describes the place of lung sliding in the BLUE-protocol (bedside lung ultrasound in emergency) (lung and venous ultrasound for diagnosing acute respiratory failure), the FALLS-protocol (fluid administration limited by lung sonography) (the role of lung sliding in circulatory failure), and the SESAME-protocol (sequential assessment of sonography assessing mechanism or origin of severe shock of indistinct cause) (whole body ultrasound in cardiac arrest). In the LUCIFLR project (LUCI favoring limitation of radiations), the consideration of lung sliding allows drastic reduction in irradiation and costs. In conclusion, lung sliding is proposed as a gold standard for indicating the presence of the lung at the chest wall and its correct expansion.
Keyword
Figure
Reference
-
References
1. Friedman J. Diagnostic procedures in respiratory diseases. Harrison’s principles of internal medicine. 12th ed. New York: McGraw-Hill;1992. p. 1043.2. Lichtenstein DA. Lung ultrasound in the critically ill. Ann Intensive Care. 2014; 1.
Article3. Lichtenstein DA. Lung Sliding. Lung Ultrasound in the Critically Ill - the BLUE-protocol. 6th ed. Heidelberg: Springer-Verlag International;2016. p. 67–78.4. Lichtenstein DA, Mezière GA. The BLUE-points: three standardized points used in the BLUE-protocol for ultrasound assessment of the lung in acute respiratory failure. Crit Ultrasound J. 2011; 3:109–10.
Article5. Guyton AC, Hall JE. Textbook of medical physiology. 9th ed. Philadelphia: W.B. Saunders Company;1996. p. 496–7.6. Lichtenstein DA, Mezière GA. Relevance of lung ultrasound in the diagnosis of acute respiratory failure: the BLUE-protocol. Chest. 2008; 134:117–25.7. van der Werf TS, Zijlstra JG. Ultrasound of the lung: just imagine. Intensive Care Med. 2004; 30:183–4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lung Ultrasound in Critically Ill Patients
- Usefulness of transthoracic lung ultrasound for the diagnosis of mild pneumothorax
- Lung Ultrasound in the Critically Ill
- Pediatric lung ultrasound: its role in the perioperative period
- Lung Cancer in patients with Idiopathic Pulmonary Fibrosis: Frequency and CT Findings