Anesth Pain Med.
2017 Jan;12(1):37-41. 10.17085/apm.2017.12.1.37.
The effect of pre-anesthetic administration of dexmedetomidine on the consumption of opioids in postoperative gynecologic patients
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea. sunnyrhee@paik.ac.kr
- KMID: 2369664
- DOI: http://doi.org/10.17085/apm.2017.12.1.37
Abstract
- BACKGROUND
This study was designed to assess whether pre-anesthetic administration of dexmedetomidine reduces the postoperative consumption of opioids, in patients receiving patient-controlled fentanyl after gynecological laparotomy.
METHODS
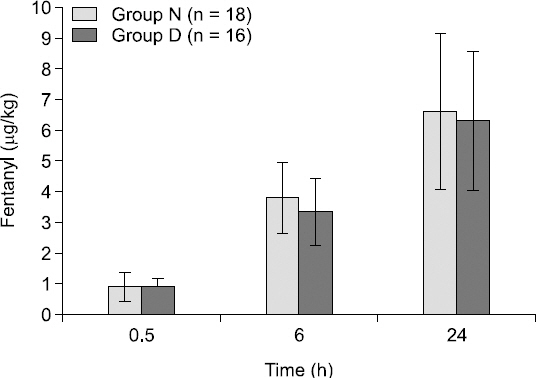
This was a prospective, randomized, double-blind, controlled study. Ten minutes before induction of anesthesia, 36 patients scheduled for elective gynecological laparotomy were assigned to receive either normal saline (group N) or dexmedetomidine 1 µg/kg (group D). A patient-controlled analgesia (PCA) device was used to administer fentanyl for the postoperative 24 h period. Cumulative fentanyl consumption and pain score were assessed at postoperative 30 min, 6 h and 24 h. Patient's satisfaction for pain control and other side effects (nausea, sedation score) were recorded for all corresponding time points.
RESULTS
There was no significant difference between the groups in cumulative fentanyl consumption (Group N: 11.1 ± 3.2 µg/kg, Group D: 10.3 ± 2.9 µg/kg, P value: 0.706). The incidence of side-effects did not differ between the groups. Both groups showed similar blood pressure after anesthesia induction. However, 10 min after anesthesia induction, the heart rates in group D were significantly lower than group N (P = 0.0002).
CONCLUSIONS
In patients undergoing gynecological laparotomy, the pre-anesthetic administration of single loading dose dexmedetomidine (1 µg/kg) given 10 min before anesthesia induction did not reduce the PCA consumption of postoperative fentanyl or the pain score.
Keyword
MeSH Terms
-
Adrenergic alpha-2 Receptor Agonists
Analgesia, Patient-Controlled
Analgesics, Opioid*
Anesthesia
Blood Pressure
Dexmedetomidine*
Fentanyl
Heart Rate
Humans
Incidence
Laparotomy
Pain, Postoperative
Passive Cutaneous Anaphylaxis
Prospective Studies
Adrenergic alpha-2 Receptor Agonists
Analgesics, Opioid
Dexmedetomidine
Fentanyl
Figure
Reference
-
1. Lam KK, Kunder S, Wong J, Doufas AG, Chung F. Obstructive sleep apnea, pain, and opioids: is the riddle solved? Curr Opin Anaesthesiol. 2016; 29:134–40. DOI: 10.1097/ACO.0000000000000265. PMID: 26545144. PMCID: PMC4927322.2. Collins SA, Joshi G, Quiroz LH, Steinberg AC, Nihira MA. Pain management strategies for urogynecologic surgery: a review. Female Pelvic Med Reconstr Surg. 2014; 20:310–5. DOI: 10.1097/SPV.0000000000000134. PMID: 25185632.3. Bang SR, Yu SK, Kim TH. Can gabapentin help reduce postoperative pain in arthroscopic rotator cuff repair? A prospective, randomized, double-blind study. Arthroscopy. 2010; 26(9 Suppl):S106–11. DOI: 10.1016/j.arthro.2009.11.010. PMID: 20810085.4. Siddiqui KM, Khan FA. Effect of preinduction low-dose ketamine bolus on intra operative and immediate postoperative analgesia requirement in day care surgery: A randomized controlled trial. Saudi J Anaesth. 2015; 9:422–7. DOI: 10.4103/1658-354X.159468. PMID: 26543461. PMCID: PMC4610088.5. Grewal A. Dexmedetomidine: New avenues. J Anaesthesiol Clin Pharmacol. 2011; 27:297–302. DOI: 10.4103/0970-9185.83670. PMID: 21897496. PMCID: PMC3161450.6. Jaakola ML, Salonen M, Lehtinen R, Scheinin H. The analgesic action of dexmedetomidine--a novel alpha 2-adrenoceptor agonist--in healthy volunteers. Pain. 1991; 46:281–5. DOI: 10.1016/0304-3959(91)90111-A.7. Venn RM, Karol MD, Grounds RM. Pharmacokinetics of dexmedetomidine infusions for sedation of postoperative patients requiring intensive caret. Br J Anaesth. 2002; 88:669–75. DOI: 10.1093/bja/88.5.669. PMID: 12067004.8. Gopalakrishna KN, Dash PK, Chatterjee N, Easwer HV, Ganesamoorthi A. Dexmedetomidine as an anesthetic adjuvant in patients undergoing transsphenoidal resection of pituitary tumor. J Neurosurg Anesthesiol. 2015; 27:209–15. DOI: 10.1097/ANA.0000000000000144. PMID: 25493927.9. Venn RM, Bradshaw CJ, Spencer R, Brealey D, Caudwell E, Naughton C, et al. Preliminary UK experience of dexmedetomidine, a novel agent for postoperative sedation in the intensive care unit. Anaesthesia. 1999; 54:1136–42. DOI: 10.1046/j.1365-2044.1999.01114.x. PMID: 10594409.10. Wang K, Li C, Shi J, Wei H. Effects of patient-controlled intravenous analgesia with dexmedetomidine and sufentanil on postoperative cognition in elderly patients after spine surgery. Zhonghua Yi Xue Za Zhi. 2015; 95:2437–41. PMID: 26711204.11. Das A, Dutta S, Chattopadhyay S, Chhaule S, Mitra T, Banu R, et al. Pain relief after ambulatory hand surgery: A comparison between dexmedetomidine and clonidine as adjuvant in axillary brachial plexus block: A prospective, double-blinded, randomized controlled study. Saudi J Anaesth. 2016; 10:6–12. DOI: 10.4103/1658-354X.169443.12. Unlugenc H, Gunduz M, Guler T, Yagmur O, Isik G. The effect of pre-anaesthetic administration of intravenous dexmedetomidine on postoperative pain in patients receiving patient-controlled morphine. Eur J Anaesthesiol. 2005; 22:386–91. DOI: 10.1017/S0265021505000669. PMID: 15918389.13. Naik BI, Nemergut EC, Kazemi A, Fernández L, Cederholm SK, McMurry TL, et al. The effect of dexmedetomidine on postoperative opioid consumption and pain after major spine surgery. Anesth Analg. 2016; 122:1646–53. DOI: 10.1213/ANE.0000000000001226. PMID: 27003917.14. Hertzog MA. Considerations in determining sample size for pilot studies. Res Nurs Health. 2008; 31:180–91. DOI: 10.1002/nur.20247. PMID: 18183564.15. Del Angel García R, Castellanos Olivares A, Munguia Miranda C. Dexmedetomidine as preventive postoperative analgesia in inguinal hernioplasty. Gac Med Mex. 2006; 142:9–12. PMID: 16548286.16. You HJ, Lei J, Xiao Y, Ye G, Sun ZH, Yang L, et al. Pre-emptive analgesia and its supraspinal mechanisms: enhanced descending inhibition and decreased descending facilitation by dexmedetomidine. J Physiol. 2016; 594:1875–90. DOI: 10.1113/JP271991. PMID: 26732231.17. Xiang H, Hu B, Li Z, Li J. Dexmedetomidine controls systemic cytokine levels through the cholinergic anti-inflammatory pathway. Inflammation. 2014; 37:1763–70. DOI: 10.1007/s10753-014-9906-1. PMID: 24803295.18. Beilin B, Bessler H, Mayburd E, Smirnov G, Dekel A, Yardeni I, et al. Effects of preemptive analgesia on pain and cytokine production in the postoperative period. Anesthesiology. 2003; 98:151–5. DOI: 10.1097/00000542-200301000-00024. PMID: 12502991.19. Doyle E, Robinson D, Morton NS. Comparison of patient-controlled analgesia with and without a background infusion after lower abdominal surgery in children. Br J Anaesth. 1993; 71:670–3. DOI: 10.1093/bja/71.6.818. PMID: 8251277.20. Owen H, Szekely SM, Plummer JL, Cushnie JM, Mather LE. Variables of patient-controlled analgesia. 2. Concurrent infusion. Anaesthesia. 1989; 44:11–3. DOI: 10.1111/j.1365-2044.1989.tb11088.x. PMID: 2929900.21. Hansen LA, Noyes MA, Lehman ME. Evaluation of patient-controlled analgesia (PCA) versus PCA plus continuous infusion in postoperative cancer patients. J Pain Symptom Manage. 1991; 6:4–14. DOI: 10.1016/0885-3924(91)90066-D.22. Etches RC. Respiratory depression associated with patient-controlled analgesia: a review of eight cases. Can J Anaesth. 1994; 41:125–32. DOI: 10.1007/BF03009805. PMID: 8131227.23. Looi-Lyons LC, Chung FF, Chan VW, McQuestion M. Respiratory depression: an adverse outcome during patient controlled analgesia therapy. J Clin Anesth. 1996; 8:151–6. DOI: 10.1016/0952-8180(95)00202-2.24. Kim KM. Analysis of the current state of postoperativepatient-controlled analgesia in Korea. Anesth Pain Med. 2016; 11:28–35. DOI: 10.17085/apm.2016.11.1.28.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intranasally Administered Adjunctive Dexmedetomidine Reduces Perioperative Anesthetic Requirements in General Anesthesia
- Preanesthetic dexmedetomidine 1 microg/kg single infusion is a simple, easy, and economic adjuvant for general anesthesia
- Comparison of Dexmedetomidine and Fentanyl as an Adjuvant to Ropivacaine for Postoperative Epidural Analgesia in Pediatric Orthopedic Surgery
- The Effect of Perineural Administration of Dexmedetomidine on Narcotic Consumption and Pain Intensity in Patients Undergoing Femoral Shaft Fracture Surgery; A Randomized Single-Blind Clinical Trial
- Effect of preoperative administration of systemic alpha-2 agonists on postoperative pain: a systematic review and meta-analysis