J Periodontal Implant Sci.
2017 Feb;47(1):51-63. 10.5051/jpis.2017.47.1.51.
A comparison of different compressive forces on graft materials during alveolar ridge preservation
- Affiliations
-
- 1Department of Periodontology, Dankook University College of Dentistry, Cheonan, Korea. perioshin@dankook.ac.kr
- KMID: 2368887
- DOI: http://doi.org/10.5051/jpis.2017.47.1.51
Abstract
- PURPOSE
Following tooth extraction, alveolar ridge preservation (ARP) can maintain the dimensions of ridge height and width. Although previous studies have demonstrated the effects of ARP, few if any studies have investigated the compressive force applied during grafting. The aim of this study was to determine the effects of different compressive forces on the graft materials during ARP.
METHODS
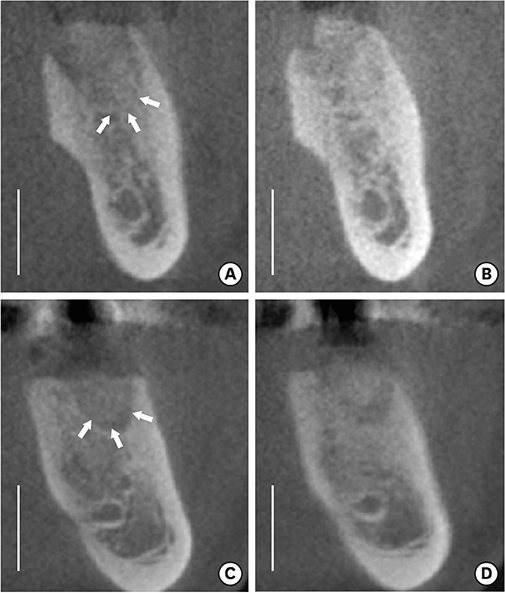
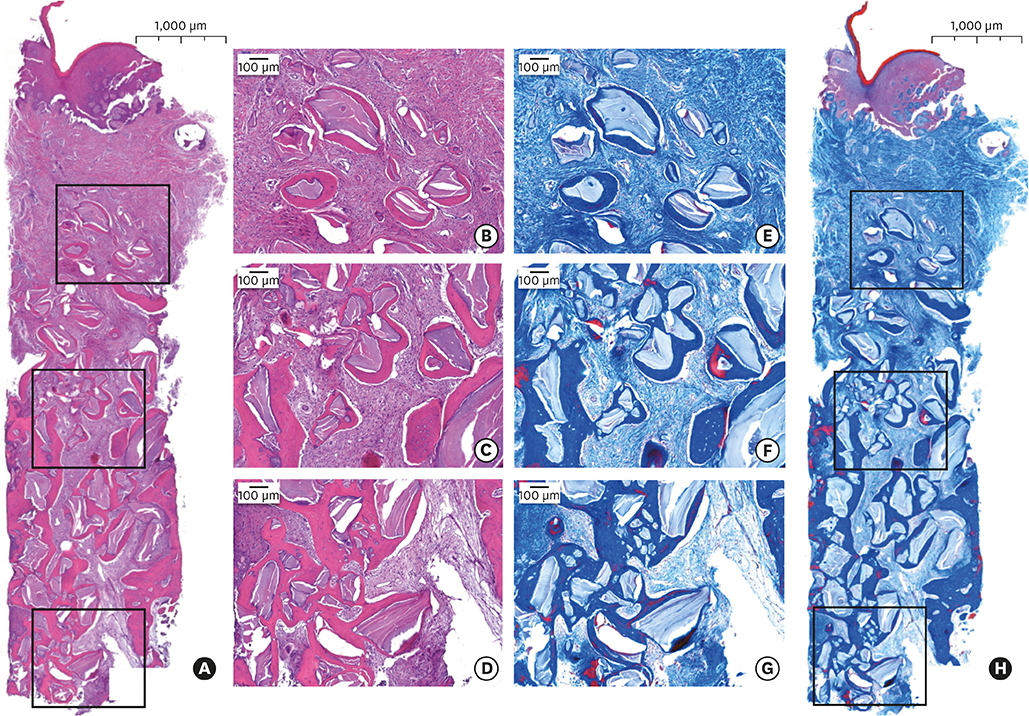
After tooth extraction, sockets were filled with deproteinized bovine bone mineral with 10% porcine collagen and covered by a resorbable collagen membrane in a double-layered fashion. The graft materials were compressed using a force of 5 N in the test group (n=12) and a force of 30 N in the control group (n=12). A hidden X suture was performed to secure the graft without primary closure. Cone-beam computed tomography (CBCT) was performed immediately after grafting and 4 months later, just before implant surgery. Tissue samples were retrieved using a trephine bur from the grafted sites during implant surgery for histologic and histomorphometric evaluations. Periotest values (PTVs) were measured to assess the initial stability of the dental implants.
RESULTS
Four patients dropped out from the control group and 20 patients finished the study. Both groups healed without any complications. The CBCT measurements showed that the ridge volume was comparably preserved vertically and horizontally in both groups (P>0.05). Histomorphometric analysis demonstrated that the ratio of new bone formation was significantly greater in the test group (P<0.05). The PTVs showed no significant differences between the 2 groups (P>0.05).
CONCLUSIONS
The application of a greater compressive force on biomaterials during ARP significantly enhanced new bone formation while preserving the horizontal and vertical dimensions of the alveolar ridge. Further studies are required to identity the optimal compressive force for ARP.
MeSH Terms
Figure
Cited by 1 articles
-
Alveolar ridge preservation with an open-healing approach using single-layer or double-layer coverage with collagen membranes
Ho-Keun Choi, Hag-Yeon Cho, Sung-Jo Lee, In-Woo Cho, Hyun-Seung Shin, Ki-Tae Koo, Hyun-Chang Lim, Jung-Chul Park
J Periodontal Implant Sci. 2017;47(6):372-380. doi: 10.5051/jpis.2017.47.6.372.
Reference
-
1. Araújo MG, Lindhe J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J Clin Periodontol. 2005; 32:212–218.
Article2. Cardaropoli G, Araújo M, Lindhe J. Dynamics of bone tissue formation in tooth extraction sites. An experimental study in dogs. J Clin Periodontol. 2003; 30:809–818.3. Devlin H, Sloan P. Early bone healing events in the human extraction socket. Int J Oral Maxillofac Surg. 2002; 31:641–645.
Article4. Trombelli L, Farina R, Marzola A, Bozzi L, Liljenberg B, Lindhe J. Modeling and remodeling of human extraction sockets. J Clin Periodontol. 2008; 35:630–639.
Article5. Ten Heggeler JM, Slot DE, Van der Weijden GA. Effect of socket preservation therapies following tooth extraction in non-molar regions in humans: a systematic review. Clin Oral Implants Res. 2011; 22:779–788.
Article6. Buser D, Dahlin C, Schenk RK. Guided bone regeneration in implant dentistry. Chicago (IL): Quintessence;1994.7. Esposito M, Grusovin MG, Coulthard P, Worthington HV. The efficacy of various bone augmentation procedures for dental implants: a Cochrane systematic review of randomized controlled clinical trials. Int J Oral Maxillofac Implants. 2006; 21:696–710.8. Esposito M, Grusovin MG, Polyzos IP, Felice P, Worthington HV. Timing of implant placement after tooth extraction: immediate, immediate-delayed or delayed implants? A Cochrane systematic review. Eur J Oral Implantology. 2010; 3:189–205.9. Nyman S, Lang NP, Buser D, Brägger U. Bone regeneration adjacent to titanium dental implants using guided tissue regeneration: a report of two cases. Int J Oral Maxillofac Implants. 1990; 5:9–14.10. Mayfield L. Immediate, delayed and late submerged and transmucosal implants. In : Proceedings of the 3rd European Workshop on Periodontology: Implant Dentistry; 1999 Jan 30–Feb 3; Thurgau, Switzerland. Berlin: Quintessenz;1999.11. Evans CD, Chen ST. Esthetic outcomes of immediate implant placements. Clin Oral Implants Res. 2008; 19:73–80.
Article12. Waasdorp JA, Evian CI, Mandracchia M. Immediate placement of implants into infected sites: a systematic review of the literature. J Periodontol. 2010; 81:801–808.
Article13. Araújo MG, Lindhe J. Ridge preservation with the use of Bio-Oss collagen: a 6-month study in the dog. Clin Oral Implants Res. 2009; 20:433–440.
Article14. Cardaropoli D, Tamagnone L, Roffredo A, Gaveglio L, Cardaropoli G. Socket preservation using bovine bone mineral and collagen membrane: a randomized controlled clinical trial with histologic analysis. Int J Periodontics Restorative Dent. 2012; 32:421–430.15. Vignoletti F, Matesanz P, Rodrigo D, Figuero E, Martin C, Sanz M. Surgical protocols for ridge preservation after tooth extraction. A systematic review. Clin Oral Implants Res. 2012; 23:Suppl 5. 22–38.
Article16. Avila-Ortiz G, Elangovan S, Kramer KW, Blanchette D, Dawson DV. Effect of alveolar ridge preservation after tooth extraction: a systematic review and meta-analysis. J Dent Res. 2014; 93:950–958.
Article17. Mardas N, Trullenque-Eriksson A, MacBeth N, Petrie A, Donos N. Does ridge preservation following tooth extraction improve implant treatment outcomes: a systematic review: Group 4: therapeutic concepts & methods. Clin Oral Implants Res. 2015; 26:Suppl 11. 180–201.
Article18. Romanos GE, Delgado-Ruiz RA, Gómez-Moreno G, López-López PJ, Mate Sanchez de Val JE, Calvo-Guirado JL. Role of mechanical compression on bone regeneration around a particulate bone graft material: an experimental study in rabbit calvaria. Clin Oral Implants Res. Forthcoming. 2015.
Article19. Krauser JT, Schetritt A. Implant site development: socket preservation. Sonick M, Hwang D. Implant site development. Chichester: Wiley-Blackwell;2012. p. 121–135.20. Delgado-Ruiz R, Romanos GE, Alexandre Gerhke S, Gomez-Moreno G, Maté-Sánchez de Val JE, Calvo-Guirado JL. Biological effects of compressive forces exerted on particulate bone grafts during socket preservation: animal study. Clin Oral Implants Res. Forthcoming. 2016.
Article21. Park JC, Koo KT, Lim HC. The hidden X suture: a technical note on a novel suture technique for alveolar ridge preservation. J Periodontal Implant Sci. 2016; 46:415–425.
Article22. Kim SH, Kim DY, Kim KH, Ku Y, Rhyu IC, Lee YM. The efficacy of a double-layer collagen membrane technique for overlaying block grafts in a rabbit calvarium model. Clin Oral Implants Res. 2009; 20:1124–1132.
Article23. Kozlovsky A, Aboodi G, Moses O, Tal H, Artzi Z, Weinreb M, et al. Bio-degradation of a resorbable collagen membrane (Bio-Gide®) applied in a double-layer technique in rats. Clin Oral Implants Res. 2009; 20:1116–1123.
Article24. Jung RE, Philipp A, Annen BM, Signorelli L, Thoma DS, Hämmerle CH, et al. Radiographic evaluation of different techniques for ridge preservation after tooth extraction: a randomized controlled clinical trial. J Clin Periodontol. 2013; 40:90–98.
Article25. Lindhe J, Cecchinato D, Donati M, Tomasi C, Liljenberg B. Ridge preservation with the use of deproteinized bovine bone mineral. Clin Oral Implants Res. 2014; 25:786–790.
Article26. Engler-Hamm D, Cheung WS, Yen A, Stark PC, Griffin T. Ridge preservation using a composite bone graft and a bioabsorbable membrane with and without primary wound closure: a comparative clinical trial. J Periodontol. 2011; 82:377–387.
Article27. Kim DM, De Angelis N, Camelo M, Nevins ML, Schupbach P, Nevins M. Ridge preservation with and without primary wound closure: a case series. Int J Periodontics Restorative Dent. 2013; 33:71–78.
Article28. Yildirim M, Spiekermann H, Biesterfeld S, Edelhoff D. Maxillary sinus augmentation using xenogenic bone substitute material Bio-Oss in combination with venous blood. A histologic and histomorphometric study in humans. Clin Oral Implants Res. 2000; 11:217–229.
Article29. McKenzie JA, Silva MJ. Comparing histological, vascular and molecular responses associated with woven and lamellar bone formation induced by mechanical loading in the rat ulna. Bone. 2011; 48:250–258.
Article30. Carmagnola D, Adriaens P, Berglundh T. Healing of human extraction sockets filled with Bio-Oss. Clin Oral Implants Res. 2003; 14:137–143.31. Zitzmann NU, Schärer P, Marinello CP, Schüpbach P, Berglundh T. Alveolar ridge augmentation with Bio-Oss: a histologic study in humans. Int J Periodontics Restorative Dent. 2001; 21:288–295.32. Araújo M, Linder E, Wennström J, Lindhe J. The influence of Bio-Oss Collagen on healing of an extraction socket: an experimental study in the dog. Int J Periodontics Restorative Dent. 2008; 28:123–135.33. Park JY, Koo KT, Kim TI, Seol YJ, Lee YM, Ku Y, et al. Socket preservation using deproteinized horse-derived bone mineral. J Periodontal Implant Sci. 2010; 40:227–231.
Article34. Sennerby L, Meredith N. Implant stability measurements using resonance frequency analysis: biological and biomechanical aspects and clinical implications. Periodontol 2000. 2008; 47:51–66.
Article35. Lotke PA, Carolan GF, Puri N. Technique for impaction bone grafting of large bone defects in revision total knee arthroplasty. J Arthroplasty. 2006; 21:57–60.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Histological comparison of different compressive forces on particulate grafts during alveolar ridge preservation: a prospective proof-of-concept study
- Implant Placement Using Alveolar Ridge Split in Atrophic Maxillary Alveolar Bone
- Improving oral rehabilitation through the preservation of the tissues through alveolar preservation
- The study on ridge preservation for implant site development
- Retrospective radiographic and clinical analysis of implant survival placed after alveolar ridge preservation