Korean J Ophthalmol.
2017 Feb;31(1):58-70. 10.3341/kjo.2017.31.1.58.
Prevalence and Factors Associated with the Use of Eye Care Services in South Korea: Korea National Health and Nutrition Examination Survey 2010–2012
- Affiliations
-
- 1Department of Ophthalmology, Chonnam National University Hospital, Chonnam National University Medical School, Gwangju, Korea.
- 2Department of Occupational and Environmental Medicine, Dong-A University Hospital, Dong-A University College of Medicine, Busan, Korea.
- 3Department of Ophthalmology, Korea University College of Medicine, Seoul, Korea.
- 4Department of Ophthalmology and Visual Science, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 5Department of Ophthalmology, Ewha Womans University Mokdong Hospital, Ewha Womans University School of Medicine, Seoul, Korea.
- 6Department of Ophthalmology, Soonchunhyang University Seoul Hospital, Seoul, Korea.
- 7Department of Ophthalmology, Kim's Eye Hospital, Konyang University College of Medicine, Seoul, Korea. drslitlamp@kimeye.com
- KMID: 2368680
- DOI: http://doi.org/10.3341/kjo.2017.31.1.58
Abstract
- PURPOSE
To estimate the factors and prevalence of eye care service utilization in the South Korean population.
METHODS
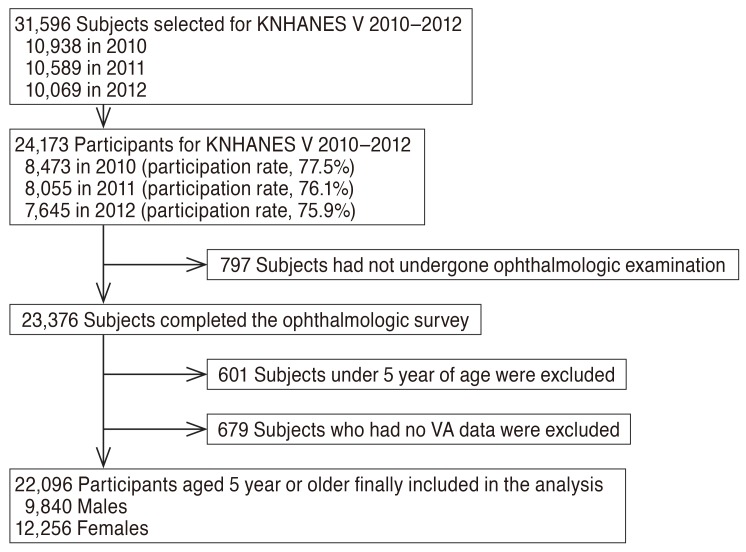
This cross-sectional, population-based study included data from 22,550 Koreans aged ≥5 years who participated in the Korea National Health and Nutrition Examination Survey from 2010 to 2012. For people aged 5 to 11 years (young children), information was based on self-reports of contact with eye care service in the past year; for people aged ≥12 years (older population), the information was based on the self-reported lifetime contact with eye care service. Univariate and multivariate logistic regression analyses of the complex sample survey data were performed.
RESULTS
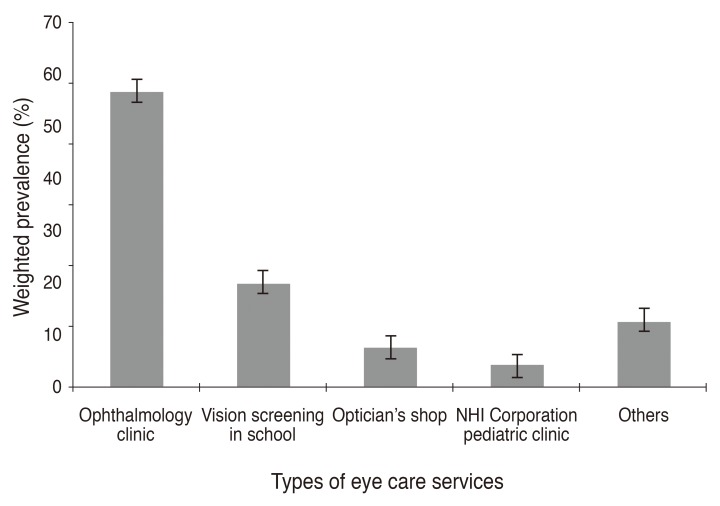
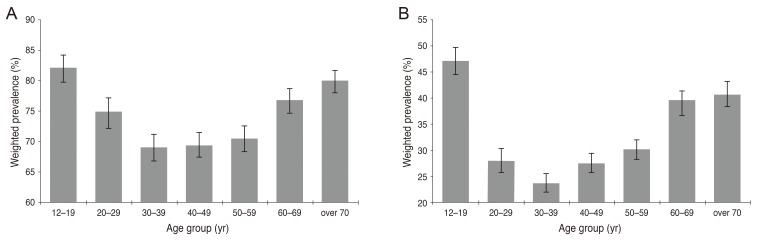
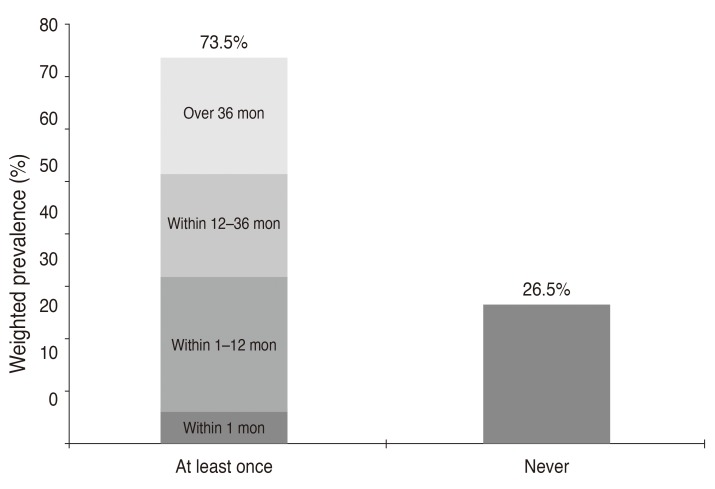
The prevalence of eye care service use in young children during the past year was 61.1% (95% confidence interval, 58.1%-64.1%), while that in the older population during their lifetime was 73.5%. Subjects aged 7 to 11 years were more likely to have had an eye examination in the past year than subjects aged 5 to 6 years (odds ratio, 3.83; 95% confidence interval, 2.37-6.19). Multivariate logistic regression analysis indicated that higher monthly household income, being a National Health Insurance holder, and having private health insurance were related to more frequent use of eye care services in young children. For the older population and women, those living in an urban area and those with a best-corrected visual acuity less than 20 / 40 in the worse-seeing eye were more likely to have had an eye examination during their lifetime. Low education level was associated with low lifetime use of eye care services in the older population.
CONCLUSIONS
There are sociodemographic disparities with use of eye care services in South Korea. This population-based study provides information that is useful for determining different intervention programs based on sociodemographic disparities to promote eye care service utilization in South Korea.
Keyword
MeSH Terms
Figure
Reference
-
1. Congdon N, O'Colmain B, Klaver CC, et al. Causes and prevalence of visual impairment among adults in the United States. Arch Ophthalmol. 2004; 122:477–485. PMID: 15078664.2. Ganz ML, Xuan Z, Hunter DG. Prevalence and correlates of children's diagnosed eye and vision conditions. Ophthalmology. 2006; 113:2298–2306. PMID: 16962175.
Article3. Wong HB, Machin D, Tan SB, et al. Visual impairment and its impact on health-related quality of life in adolescents. Am J Ophthalmol. 2009; 147:505–511. PMID: 19056077.
Article4. Chadha RK, Subramanian A. The effect of visual impairment on quality of life of children aged 3-16 years. Br J Ophthalmol. 2011; 95:642–645. PMID: 20852314.
Article5. Eye examination and vision screening in infants, children, and young adults: American Academy of Pediatrics Committee on Practice and Ambulatory Medicine, Section on Ophthalmology. Pediatrics. 1996; 98:153–157. PMID: 8668393.6. American Academy of Pediatrics; Section on Ophthalmology; American Association for Pediatric Ophthalmology and Strabismus, et al. Red reflex examination in neonates, infants, and children. Pediatrics. 2008; 122:1401–1404. PMID: 19047263.7. Beauchamp GR, Ellepola C, Beauchamp CL. Evidence-based medicine: the value of vision screening. Am Orthopt J. 2010; 60:23–27. PMID: 21061880.
Article8. Solebo AL, Cumberland PM, Rahi JS. Whole-population vision screening in children aged 4-5 years to detect amblyopia. Lancet. 2015; 385:2308–2319. PMID: 25499167.
Article9. Moradabadi AS, Ghanbarnejad A, Bani-Hashemi A, et al. Amblyopia screening in children in Bandar Abbas (Iran) during 2011-2012. Electron Physician. 2014; 6:906–911. PMID: 25763166.10. Hoeg TB, Moldow B, Ellervik C, et al. Danish Rural Eye Study: the association of preschool vision screening with the prevalence of amblyopia. Acta Ophthalmol. 2015; 93:322–329. PMID: 25545299.
Article11. Chen X, Fu Z, Yu J, et al. Prevalence of amblyopia and strabismus in Eastern China: results from screening of preschool children aged 36-72 months. Br J Ophthalmol. 2016; 100:515–519. PMID: 26261229.12. Cho W, Lee S, Kang HY, Kang M. Setting national priorities for quality assessment of health care services in Korea. Int J Qual Health Care. 2005; 17:157–165. PMID: 15723820.
Article13. Choi YJ, Kim HC, Kim HM, et al. Prevalence and management of diabetes in Korean adults: Korea National Health and Nutrition Examination Surveys 1998-2005. Diabetes Care. 2009; 32:2016–2020. PMID: 19675201.14. Kim Y. The Korea National Health and Nutrition Examination Survey (KNHANES): current status and challenges. Epidemiol Health. 2014; 36:e2014002. PMID: 24839580.
Article15. Kweon S, Kim Y, Jang MJ, et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol. 2014; 43:69–77. PMID: 24585853.
Article16. Yoon KC, Mun GH, Kim SD, et al. Prevalence of eye diseases in South Korea: data from the Korea National Health and Nutrition Examination Survey 2008-2009. Korean J Ophthalmol. 2011; 25:421–433. PMID: 22131780.
Article17. Park Y, Shin JA, Yang SW, et al. The relationship between visual impairment and health-related quality of life in Korean adults: The Korea National Health and Nutrition Examination Survey (2008-2012). PLoS One. 2015; 10:e0132779. PMID: 26192763.
Article18. Park SH, Lee JS, Heo H, et al. A nationwide population-based study of low vision and blindness in South Korea. Invest Ophthalmol Vis Sci. 2014; 56:484–493. PMID: 25525165.
Article19. Lim HT, Yoon JS, Hwang SS, Lee SY. Prevalence and associated sociodemographic factors of myopia in Korean children: the 2005 third Korea National Health and Nutrition Examination Survey (KNHANES III). Jpn J Ophthalmol. 2012; 56:76–81. PMID: 21975827.
Article20. Ahn JM, Lee SH, Rim TH, et al. Prevalence of and risk factors associated with dry eye: the Korea National Health and Nutrition Examination Survey 2010-2011. Am J Ophthalmol. 2014; 158:1205–1214. PMID: 25149910.
Article21. Yoon KC, Choi W, Lee HS, et al. An overview of ophthalmologic survey methodology in the 2008-2015 Korean National Health and Nutrition Examination Surveys. Korean J Ophthalmol. 2015; 29:359–367. PMID: 26635451.
Article22. Ganz M, Xuan Z, Hunter DG. Patterns of eye care use and expenditures among children with diagnosed eye conditions. J AAPOS. 2007; 11:480–487. PMID: 17434774.
Article23. Rowe S, MacLean CH, Shekelle PG. Preventing visual loss from chronic eye disease in primary care: scientific review. JAMA. 2004; 291:1487–1495. PMID: 15039416.
Article24. Su Z, Marvin EK, Wang BQ, et al. Identifying barriers to follow-up eye care for children after failed vision screening in a primary care setting. J AAPOS. 2013; 17:385–390. PMID: 23993718.
Article25. Williams S, Wajda BN, Alvi R, et al. The challenges to ophthalmologic follow-up care in at-risk pediatric populations. J AAPOS. 2013; 17:140–143. PMID: 23622446.
Article26. Moon S, Shin J. Performance of universal health insurance: lessons from South Korea. World Health Popul. 2007; 9:95–113. PMID: 18270509.
Article27. Lee DJ, Lam BL, Arora S, et al. Reported eye care utilization and health insurance status among US adults. Arch Ophthalmol. 2009; 127:303–310. PMID: 19273794.
Article28. Morales LS, Varma R, Paz SH, et al. Self-reported use of eye care among Latinos: the Los Angeles Latino Eye Study. Ophthalmology. 2010; 117:207–215. PMID: 20018380.29. McGwin G, Khoury R, Cross J, Owsley C. Vision impairment and eye care utilization among Americans 50 and older. Curr Eye Res. 2010; 35:451–458. PMID: 20465437.
Article30. Jin YP, Trope GE. Eye care utilization in Canada: disparity in the publicly funded health care system. Can J Ophthalmol. 2011; 46:133–138. PMID: 21708079.
Article31. Puent BD, Klein BE, Klein R, et al. Factors related to vision care in an older adult cohort. Optom Vis Sci. 2005; 82:612–616. PMID: 16044073.
Article32. Nirmalan PK, Katz J, Robin AL, et al. Utilisation of eye care services in rural south India: the Aravind Comprehensive Eye Survey. Br J Ophthalmol. 2004; 88:1237–1241. PMID: 15377541.
Article33. Emamian MH, Zeraati H, Majdzadeh R, et al. Economic inequality in eye care utilization and its determinants: a Blinder-Oaxaca decomposition. Int J Health Policy Manag. 2014; 3:307–313. PMID: 25396206.
Article34. Perruccio AV, Badley EM, Trope GE. A Canadian population-based study of vision problems: assessing the significance of socioeconomic status. Can J Ophthalmol. 2010; 45:477–483. PMID: 20729934.
Article35. Ulldemolins AR, Lansingh VC, Valencia LG, et al. Social inequalities in blindness and visual impairment: a review of social determinants. Indian J Ophthalmol. 2012; 60:368–375. PMID: 22944744.
Article36. Robinson B, Feng Y, Woods CA, et al. Prevalence of visual impairment and uncorrected refractive error: report from a Canadian urban population-based study. Ophthalmic Epidemiol. 2013; 20:123–130. PMID: 23713914.37. Ferraz FH, Corrente JE, Opromolla P, Schellini SA. Influence of uncorrected refractive error and unmet refractive error on visual impairment in a Brazilian population. BMC Ophthalmol. 2014; 14:84. PMID: 24965318.
Article38. Courtright P, Bassett K. Gender and blindness: eye disease and the use of eye care services. Community Eye Health. 2003; 16:11–12. PMID: 17491863.39. Fang YT, Chou YJ, Liu CY, et al. Factors associated with subsequent eye care for children in Taiwan: a population-based historical cohort study. Ophthalmic Epidemiol. 2012; 19:350–357. PMID: 23171204.
Article40. Do YK, Eggleston KN. Educational disparities in quality of diabetes care in a universal health insurance system: evidence from the 2005 Korea National Health and Nutrition Examination Survey. Int J Qual Health Care. 2011; 23:397–404. PMID: 21705771.
Article41. Wang D, Ding X, He M, et al. Use of eye care services among diabetic patients in urban and rural China. Ophthalmology. 2010; 117:1755–1762. PMID: 20471689.
Article42. Centers for Disease Control and Prevention (CDC). Eye-care utilization among women aged > or =40 years with eye diseases: 19 states, 2006-2008. MMWR Morb Mortal Wkly Rep. 2010; 59:588–591. PMID: 20489682.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationship between Dry Eye Syndrome and Frequency of Coffee Consumption in Korean Adults: Korea National Health and Nutrition Examination Survey V, 2010–2012
- The prevalence and risk factors for pterygium in South Korea: the Korea National Health and Nutrition Examination Survey (KNHANES) 2009-2010
- Factors Associated with Dry Eye Symptoms in Elderly Koreans: The Fifth Korea National Health and Nutrition Examination Survey 2010–2012
- Comparison of estimates and time series stability of Korea Community Health Survey and Korea National Health and Nutrition Examination Survey
- The 2016 Korea National Health and Nutritional Examination Survey of the Prevalence of Amblyopia