Korean J Ophthalmol.
2017 Feb;31(1):9-15. 10.3341/kjo.2017.31.1.9.
Surgical Outcomes of Porcine Acellular Dermis Graft in Anophthalmic Socket: Comparison with Oral Mucosa Graft
- Affiliations
-
- 1Institute of Vision Research, Department of Ophthalmology, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. yoonjs@yuhs.ac
- 2Singapore National Eye Centre, Singapore, Singapore.
- 3Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2368673
- DOI: http://doi.org/10.3341/kjo.2017.31.1.9
Abstract
- PURPOSE
We describe our experience with the Permacol graft in anophthalmic socket reconstruction, and compare it to the autologous buccal mucosal graft, emphasizing the postoperative vascularization and contraction of each graft.
METHODS
This was a retrospective comparative study. We measured the time necessary for the graft surface to be completely vascularized, as well as the fornix depth of the conjunctival sac in anophthalmic patients.
RESULTS
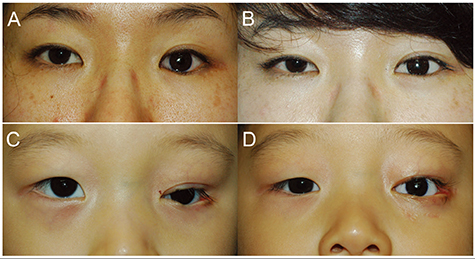
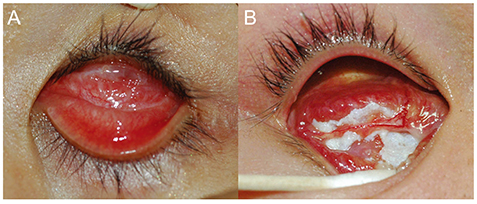
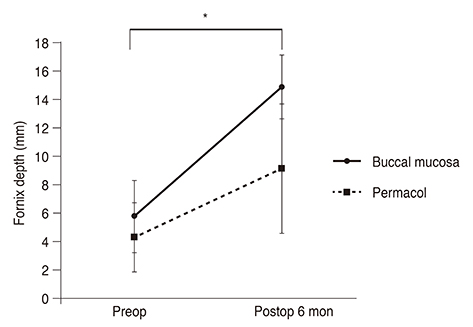
Ten patients underwent Permacol graft reconstruction, with 44 undergoing buccal mucosal graft reconstruction. Seven eyelids (70%) in the Permacol group had a good outcome, with improvement in lower eyelid position and prosthesis retention. Nine out of 10 eyelids (90%) in this group showed complete vascularization of the graft at 2.6 ± 1.9 months postoperatively, while the grafted buccal mucosa was fully vascularized at 1.1 ± 0.3 months postoperatively (p < 0.01). Postoperative fornix depth in the Permacol group was 9.1 ± 2.2 mm, compared to 14.9 ± 4.5 mm in the buccal mucosal graft group (p < 0.01). Mean increases in fornix depth were 33.1% and 67.9% of the mean vertical length of the implanted graft.
CONCLUSIONS
The Permacol graft can be useful as spacer graft material in anophthalmic socket patients. It takes longer to vascularize, and undergoes greater graft shrinkage with time, compared to the buccal mucosal graft.
Keyword
MeSH Terms
Figure
Reference
-
1. Hashikawa K, Terashi H, Tahara S. Therapeutic strategy for the triad of acquired anophthalmic orbit. Plast Reconstr Surg. 2007; 119:2182–2188.2. Yoshizawa M, Feinberg SE, Marcelo CL, Elner VM. Ex vivo produced human conjunctiva and oral mucosa equivalents grown in a serum-free culture system. J Oral Maxillofac Surg. 2004; 62:980–988.3. McCord C, Nahai FR, Codner MA, et al. Use of porcine acellular dermal matrix (Enduragen) grafts in eyelids: a review of 69 patients and 129 eyelids. Plast Reconstr Surg. 2008; 122:1206–1213.4. Belcher HJ, Zic R. Adverse effect of porcine collagen interposition after trapeziectomy: a comparative study. J Hand Surg Br. 2001; 26:159–164.5. Liyanage SH, Purohit GS, Frye JN, Giordano P. Anterior abdominal wall reconstruction with a Permacol implant. J Plast Reconstr Aesthet Surg. 2006; 59:553–555.6. Cheung D, Brown L, Sampath R. Localized inferior orbital fibrosis associated with porcine dermal collagen xenograft orbital floor implant. Ophthal Plast Reconstr Surg. 2004; 20:257–259.7. Peter NM, Kumar B. Permacol in eyelid reconstruction: a novel use. Orbit. 2013; 32:57–59.8. Klein M, Menneking H, Bier J. Reconstruction of the contracted ocular socket with free full-thickness mucosa graft. Int J Oral Maxillofac Surg. 2000; 29:96–98.9. Molgat YM, Hurwitz JJ, Webb MC. Buccal mucous membrane-fat graft in the management of the contracted socket. Ophthal Plast Reconstr Surg. 1993; 9:267–272.10. Liao SL, Wei YH. Correction of lower lid retraction using tarSys bioengineered grafts for graves ophthalmopathy. Am J Ophthalmol. 2013; 156:387–392.e1.11. Kim HJ, Grossniklaus HE, Wojno TH. A cyst-like foreign body reaction to porcine decellularized membrane (TarSys). Ophthal Plast Reconstr Surg. 2014; 30:e100–e102.12. Xie WG, Tan H, Zhao CL, Wang H. The histological changes and the revascularization process in the grafted dermal substitutes. Zhonghua Shao Shang Za Zhi. 2005; 21:37–39.13. Rubin PA, Fay AM, Remulla HD, Maus M. Ophthalmic plastic applications of acellular dermal allografts. Ophthalmology. 1999; 106:2091–2097.14. Liu Z, Tang R, Zhou Z, et al. Comparison of two porcine-derived materials for repairing abdominal wall defects in rats. PLoS One. 2011; 6:e20520.15. Sullivan SA, Dailey RA. Graft contraction: a comparison of acellular dermis versus hard palate mucosa in lower eyelid surgery. Ophthal Plast Reconstr Surg. 2003; 19:14–24.16. Owens KW, Yukna RA. Collagen membrane resorption in dogs: a comparative study. Implant Dent. 2001; 10:49–58.17. Gryskiewicz JM, Rohrich RJ, Reagan BJ, Schwartz BM. The use of Alloderm for the correction of nasal contour deformities. Plast Reconstr Surg. 2001; 107:571.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Observation on Reconstruction of the Contracted Anophthalmic Socket by the Dermis-fat Graft
- Anophthalmic Socket Reconstruction
- Reconstruction of Contracted Anophthalmic Socket with Acellular Dermal Allograft
- Anophthalmic Conjunctival Sac Reconstruction using Acellular Dermal Allograft
- Management of Acquired Anophthalmic Socket