Allergy Asthma Respir Dis.
2017 Jan;5(1):3-7. 10.4168/aard.2017.5.1.3.
Upper airway and obstructive sleep apnea in children
- Affiliations
-
- 1Department of Pediatrics, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea. hyemijee@gmail.com
- KMID: 2368569
- DOI: http://doi.org/10.4168/aard.2017.5.1.3
Abstract
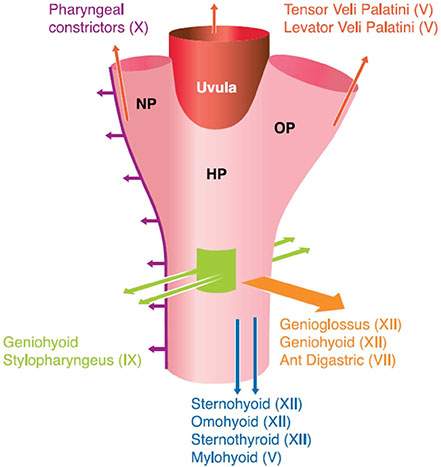
- Obstructive sleep apnea (OSA) is characterized by a disorder of breathing with prolonged partial and/or complete airway obstruction which causes frequent arousal during sleep. The prevalence of OSAS is approximately 2%-3.5% in children. It is mainly caused by enlarged tonsils and adenoids. Obesity, craniofacial abnormality, and neuromuscular disease are also relevant predisposing factors. Snoring is the most common presenting complaint in children with OSA, but the clinical presentation varies according to age. The pathogenesis of OSA is complex and involved in multifactorial, relative roles of anatomic and neurohumoral factors. The role of the nose is considered a component of the pathophysiology of OSA. It is unlikely that the first manifestation of OSA is intermittent snoring with nasal obstruction, often considered a coincidental finding. Childhood OSA should be diagnosed and treated, if clinically suspected, because various symptoms, signs, and consequences can be improved with proper management. Adenotonsillectomy is the first-line treatment modality in pediatric OSA with adenotonsillar hypertrophy. In addition, treatment of allergic rhinitis, nonallergic rhinitis, and other structural problems of the nasal cavity, if it is needed, may be included in the treatment of OSA.
Keyword
MeSH Terms
Figure
Reference
-
1. American Thoracic Society. Standards and indications for cardiopulmonary sleep studies in children. Am J Respir Crit Care Med. 1996; 153:866–878.2. Marcus CL. Sleep-disordered breathing in children. Curr Opin Pediatr. 2000; 12:208–212.
Article3. Marcus CL. Sleep-disordered breathing in children. Am J Respir Crit Care Med. 2001; 164:16–30.
Article4. O'Brien LM, Mervis CB, Holbrook CR, Bruner JL, Klaus CJ, Rutherford J, et al. Neurobehavioral implications of habitual snoring in children. Pediatrics. 2004; 114:44–49.5. Chay OM, Goh A, Abisheganaden J, Tang J, Lim WH, Chan YH, et al. Obstructive sleep apnea syndrome in obese Singapore children. Pediatr Pulmonol. 2000; 29:284–290.
Article6. Gislason T, Benediktsdóttir B. Snoring, apneic episodes, and nocturnal hypoxemia among children 6 months to 6 years old. An epidemiologic study of lower limit of prevalence. Chest. 1995; 107:963–966.
Article7. Shin C, Joo S, Kim J, Kim T. Prevalence and correlates of habitual snoring in high school students. Chest. 2003; 124:1709–1715.
Article8. Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002; 165:1217–1239.9. Li AM, Sadeh A, Au CT, Goh DY, Mindell JA. Prevalence of habitual snoring and its correlates in young children across the Asia Pacific. J Paediatr Child Health. 2013; 49:E153–E159.
Article10. Berry RB, Gamaldo CE, Harding SM, Brooks R, Lloyd RM, Vaughn BV, et al. AASM scoring manual version 2.2 updates: new chapters for scoring infant sleep staging and home sleep apnea testing. J Clin Sleep Med. 2015; 11:1253–1254.
Article11. Dempsey JA, Veasey SC, Morgan BJ, O'Donnell CP. Pathophysiology of sleep apnea. Physiol Rev. 2010; 90:47–112.
Article12. Ferris BG Jr, Mead J, Opie LH. Partitioning of respiratory flow resistance in man. J Appl Physiol. 1964; 19:653–658.
Article13. White DP. The pathogenesis of obstructive sleep apnea: advances in the past 100 years. Am J Respir Cell Mol Biol. 2006; 34:1–6.14. Sforza E, Petiau C, Weiss T, Thibault A, Krieger J. Pharyngeal critical pressure in patients with obstructive sleep apnea syndrome. Clinical implications. Am J Respir Crit Care Med. 1999; 159:149–157.
Article15. Epstein LJ, Kristo D, Strollo PJ Jr, Friedman N, Malhotra A, Patil SP, et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009; 5:263–276.16. Schwartz AR, Patil SP, Laffan AM, Polotsky V, Schneider H, Smith PL. Obesity and obstructive sleep apnea: pathogenic mechanisms and therapeutic approaches. Proc Am Thorac Soc. 2008; 5:185–192.
Article17. Phillips BG, Kato M, Narkiewicz K, Choe I, Somers VK. Increases in leptin levels, sympathetic drive, and weight gain in obstructive sleep apnea. Am J Physiol Heart Circ Physiol. 2000; 279:H234–H237.
Article18. Dobrosielski DA, Patil S, Schwartz AR, Bandeen-Roche K, Stewart KJ. Effects of exercise and weight loss in older adults with obstructive sleep apnea. Med Sci Sports Exerc. 2015; 47:20–26.
Article19. Bradley TD, Brown IG, Grossman RF, Zamel N, Martinez D, Phillipson EA, et al. Pharyngeal size in snorers, nonsnorers, and patients with obstructive sleep apnea. N Engl J Med. 1986; 315:1327–1331.
Article20. Brunetti L, Rana S, Lospalluti ML, Pietrafesa A, Francavilla R, Fanelli M, et al. Prevalence of obstructive sleep apnea syndrome in a cohort of 1,207 children of southern Italy. Chest. 2001; 120:1930–1935.
Article21. Friedman M, Wilson M, Lin HC, Chang HW. Updated systematic review of tonsillectomy and adenoidectomy for treatment of pediatric obstructive sleep apnea/hypopnea syndrome. Otolaryngol Head Neck Surg. 2009; 140:800–808.
Article22. Villa MP, Rizzoli A, Miano S, Malagola C. Efficacy of rapid maxillary expansion in children with obstructive sleep apnea syndrome: 36 months of follow-up. Sleep Breath. 2011; 15:179–184.
Article23. Fernbach SK, Brouillette RT, Riggs TW, Hunt CE. Radiologic evaluation of adenoids and tonsils in children with obstructive sleep apnea: plain films and fluoroscopy. Pediatr Radiol. 1983; 13:258–265.
Article24. Arens R, McDonough JM, Costarino AT, Mahboubi S, Tayag-Kier CE, Maislin G, et al. Magnetic resonance imaging of the upper airway structure of children with obstructive sleep apnea syndrome. Am J Respir Crit Care Med. 2001; 164:698–703.
Article25. Laurikainen E, Aitasalo K, Erkinjuntti M, Wanne O. Sleep apnea syndrome in children--secondary to adenotonsillar hypertrophy? Acta Otolaryngol Suppl. 1992; 492:38–41.
Article26. Choi JH, Kim EJ, Choi J, Kwon SY, Kim TH, Lee SH, et al. Obstructive sleep apnea syndrome: a child is not just a small adult. Ann Otol Rhinol Laryngol. 2010; 119:656–661.
Article27. Redline S, Tishler PV, Schluchter M, Aylor J, Clark K, Graham G. Risk factors for sleep-disordered breathing in children. Associations with obesity, race, and respiratory problems. Am J Respir Crit Care Med. 1999; 159(5 Pt 1):1527–1532.
Article28. Georgalas C. The role of the nose in snoring and obstructive sleep apnoea: an update. Eur Arch Otorhinolaryngol. 2011; 268:1365–1373.
Article29. Lavigne F, Petrof BJ, Johnson JR, Lavigne P, Binothman N, Kassissia GO, et al. Effect of topical corticosteroids on allergic airway inflammation and disease severity in obstructive sleep apnoea. Clin Exp Allergy. 2013; 43:1124–1133.30. Brouillette RT, Manoukian JJ, Ducharme FM, Oudjhane K, Earle LG, Ladan S, et al. Efficacy of fluticasone nasal spray for pediatric obstructive sleep apnea. J Pediatr. 2001; 138:838–844.
Article31. Goldbart AD, Greenberg-Dotan S, Tal A. Montelukast for children with obstructive sleep apnea: a double-blind, placebo-controlled study. Pediatrics. 2012; 130:e575–e580.
Article32. MacLean JE. Montelukast potentially efficacious in children with non-severe obstructive sleep apnoea in the short term. Evid Based Med. 2013; 18:173–174.
Article33. McNicholas WT, Tarlo S, Cole P, Zamel N, Rutherford R, Griffin D, et al. Obstructive apneas during sleep in patients with seasonal allergic rhinitis. Am Rev Respir Dis. 1982; 126:625–628.34. Craig TJ, Teets S, Lehman EB, Chinchilli VM, Zwillich C. Nasal congestion secondary to allergic rhinitis as a cause of sleep disturbance and daytime fatigue and the response to topical nasal corticosteroids. J Allergy Clin Immunol. 1998; 101:633–637.
Article35. Liistro G, Rombaux P, Belge C, Dury M, Aubert G, Rodenstein DO. High Mallampati score and nasal obstruction are associated risk factors for obstructive sleep apnoea. Eur Respir J. 2003; 21:248–252.
Article36. Kiely JL, Nolan P, McNicholas WT. Intranasal corticosteroid therapy for obstructive sleep apnoea in patients with co-existing rhinitis. Thorax. 2004; 59:50–55.37. Höijer U, Ejnell H, Hedner J, Petruson B, Eng LB. The effects of nasal dilation on snoring and obstructive sleep apnea. Arch Otolaryngol Head Neck Surg. 1992; 118:281–284.
Article38. Li HY, Lin Y, Chen NH, Lee LA, Fang TJ, Wang PC. Improvement in quality of life after nasal surgery alone for patients with obstructive sleep apnea and nasal obstruction. Arch Otolaryngol Head Neck Surg. 2008; 134:429–433.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Pediatric Obstructive Hypoventilation Managed with Upper Airway Surgery
- Upper airway studies in patients with obstructive sleep apnea syndrome
- Pathogenesis of Obstructive Sleep Apnea
- Upper airway myofunctional exercise: a systematic review
- Contemporary Methods of Upper Airway Evaluation in Obstructive Sleep Apnea Patients