The Trends of Atrial Fibrillation-Related Hospital Visit and Cost, Treatment Pattern and Mortality in Korea: 10-Year Nationwide Sample Cohort Data
- Affiliations
-
- 1Division of Cardiology, National Health Insurance Service Ilsan Hospital, Goyang, Korea.
- 2Division of Cardiology, Department of Internal Medicine, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea. cby6908@yuhs.ac
- KMID: 2365283
- DOI: http://doi.org/10.4070/kcj.2016.0045
Abstract
- BACKGROUND AND OBJECTIVES
The change of in-hospital and out-hospital treatments, and hospital costs for atrial fibrillation (AF) were not well known in rapidly aging Asian countries. This study is to examine the trends of AF management and outcomes in Korea.
SUBJECTS AND METHODS
In the sample cohort from Korean National Health Insurance Data Sample Cohort (K-NHID-Sample Cohort) from 2004 through 2013, we identified patients with AF and hospital visit records using Korean Classification of Diseases, 6th Revision (KCD-6). Hospital cost, prescribed medications, radiofrequency catheter ablation (RFCA), morbidity and mortality were identified.
RESULTS
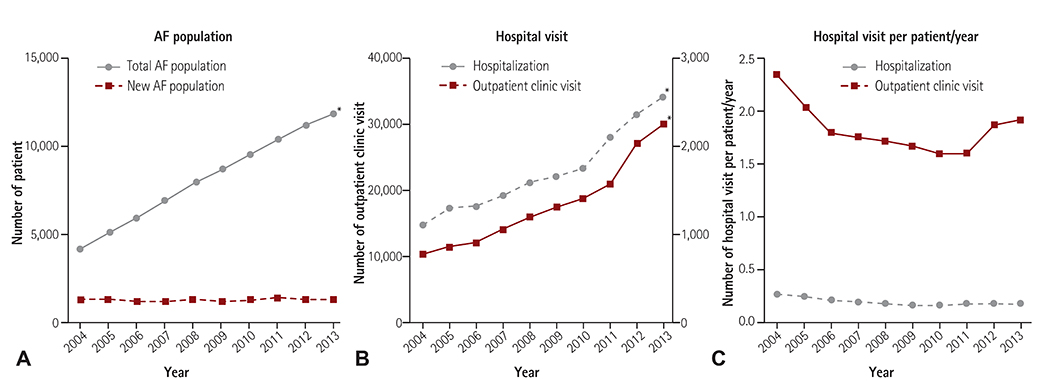
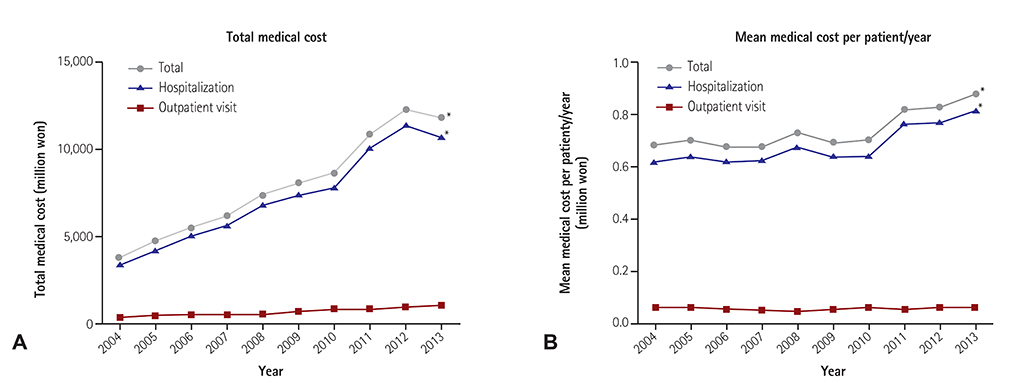
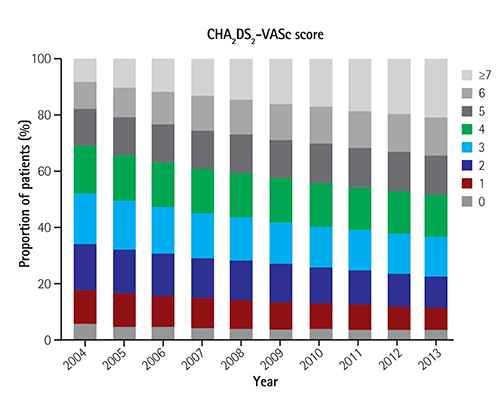
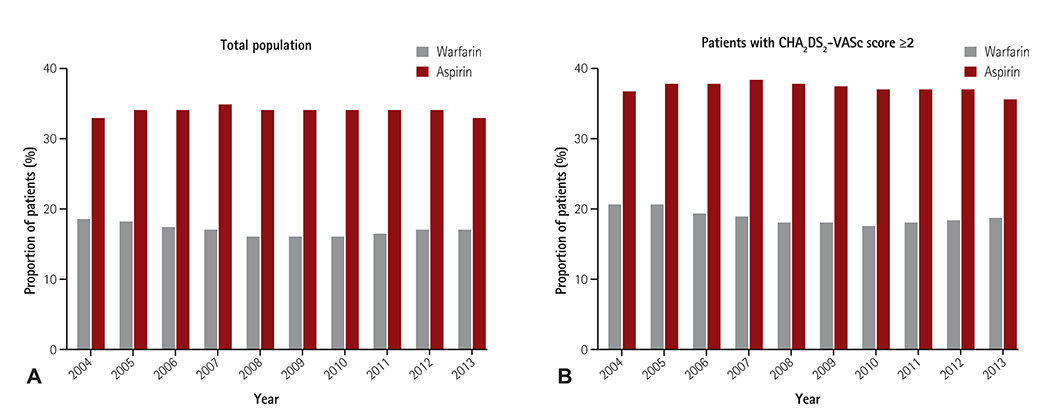
AF-related hospitalization and outpatient clinic visits increased by 2.19 and 3.06-fold, respectively. While the total cost increased from 3.6 to 11.3 billion won (p<0.001), the mean cost per patient increased from 0.68 to 0.83 million won (p<0.001). Although the mean CHAâ‚‚DSâ‚‚-VASc score increased from 3.5 to 4.4 in the total AF population, the proportion of patients who receive anticoagulation therapy with warfarin showed no significant change for the decade. The proportion of hospitalization for RFCA was increased (0.4% to 1.1%, p<0.001). All-cause mortality (6.7% to 5.0%), cardiovascular mortality (1.4% to 1.1%) and stroke-related death (1.3% to 0.8%) showed a modest decrease from 2004 to 2013.
CONCLUSION
During the last decade, AF-related hospitalization and outpatient clinic visits have increased with the increase of many other comorbidities, whereas the rate of anticoagulation did not improved. Although mortality in patients with AF showed a modest decrease from 2004 to 2013, proper anticoagulation therapy is warranted for the improvement of public health.
MeSH Terms
Figure
Cited by 12 articles
-
2018 Korean Guideline of Atrial Fibrillation Management
Boyoung Joung, Jung Myung Lee, Ki Hong Lee, Tae-Hoon Kim, Eue-Keun Choi, Woo-Hyun Lim, Ki-Woon Kang, Jaemin Shim, Hong Euy Lim, Junbeom Park, So-Ryoung Lee, Young Soo Lee, Jin-Bae Kim,
Korean Circ J. 2018;48(12):1033-1080. doi: 10.4070/kcj.2018.0339.Regional and Socioeconomic Inequality of Atrial Fibrillation with Regular Hospital Visit
Pil-Sung Yang, Boyoung Joung
Korean Circ J. 2018;48(7):635-636. doi: 10.4070/kcj.2018.0116.Gender Difference in Catheter Ablation: Atrial Fibrillations from Mars and Venus?
Hee Tae Yu, Hui-Nam Pak
Korean Circ J. 2018;48(7):619-621. doi: 10.4070/kcj.2018.0094.Evolution of Smart Health Wearables: Novel Application for Detection of Arrhythmia
Jumsuk Ko, Nam-Ho Kim
Korean Circ J. 2019;49(5):446-447. doi: 10.4070/kcj.2019.0078.Risk Factor Management for Atrial Fibrillation
Boyoung Joung
Korean Circ J. 2019;49(9):794-807. doi: 10.4070/kcj.2019.0212.Social Inequalities of Oral Anticoagulation after the Introduction of Non-Vitamin K Antagonists in Patients with Atrial Fibrillation
Hee Tae Yu, Pil-Sung Yang, Jinseub Hwang, Soorack Ryu, Eunsun Jang, Tae-Hoon Kim, Jae-Sun Uhm, Jong-Youn Kim, Hui-Nam Pak, Moon-Hyoung Lee, Gregory Y.H. Lip, Boyoung Joung
Korean Circ J. 2020;50(3):267-277. doi: 10.4070/kcj.2019.0207.Guideline of atrial fibrillation management
Boyoung Joung
J Korean Med Assoc. 2019;62(5):265-274. doi: 10.5124/jkma.2019.62.5.265.Percutaneous Left Atrial Appendage Occlusion Yields Favorable Neurological Outcomes in Patients with Non-Valvular Atrial Fibrillation
Oh-Hyun Lee, Young Dae Kim, Jung-Sun Kim, Nak-Hoon Son, Hui-Nam Pak, Boyoung Joung, Cheol-Woong Yu, Hyun-Jong Lee, Woong-Chol Kang, Eun-Seok Shin, Rak-kyeong Choi, Do-Sun Lim, Yo Han Jung, Hye-Yeon Choi, Kyung-Yul Lee, Bang-Hoon Cho, Sang Won Han, Joong Hyun Park, Han-Jin Cho, Hyung Jong Park, Hyo Suk Nam, Ji Hoe Heo, Chak-yu So, Gary Shing-Him Cheung, Yat-yin Lam, Xavier Freixa, Apostolos Tzikas, Yangsoo Jang, Jai-Wun Park
Korean Circ J. 2021;51(7):626-638. doi: 10.4070/kcj.2020.0527.Cost-Effectiveness of Rate- and Rhythm-Control Drugs for Treating Atrial Fibrillation in Korea
Min Kim, Woojin Kim, Changsoo Kim, Boyoung Joung
Yonsei Med J. 2019;60(12):1157-1163. doi: 10.3349/ymj.2019.60.12.1157.Antithrombotic Medication and the Risk of Vitreous Hemorrhage in Atrial Fibrillation: Korean National Health Insurance Service National Cohort
Ko Eun Kim, Pil-Sung Yang, Eunsun Jang, Sungjin Kim, Boyoung Joung
Yonsei Med J. 2019;60(1):65-72. doi: 10.3349/ymj.2019.60.1.65.Current Anticoagulant Usage Patterns and Determinants in Korean Patients with Nonvalvular Atrial Fibrillation
Hyun Su Ha, Joongmin Kim, Young Soo Lee, Tae-Hoon Kim, Jung Myung Lee, Junbeom Park, Jin-Kyu Park, Ki-Woon Kang, Jaemin Shim, Jae-Sun Uhm, Hyung Wook Park, Myung-Jin Cha, Eue-Keun Choi, Jun Kim, Jin-Bae Kim, Changsoo Kim, Boyoung Joung
Yonsei Med J. 2020;61(2):120-128. doi: 10.3349/ymj.2020.61.2.120.Optimal Rhythm Control Strategy in Patients With Atrial Fibrillation
Daehoon Kim, Pil-Sung Yang, Boyoung Joung
Korean Circ J. 2022;52(7):496-512. doi: 10.4070/kcj.2022.0078.
Reference
-
1. January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014; 64:e1–e76.2. Benjamin EJ, Wolf PA, D'Agostino RB, Silbershatz H, Kannel WB, Levy D. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation. 1998; 98:946–952.3. Wang TJ, Larson MG, Levy D, et al. Temporal relations of atrial fibrillation and congestive heart failure and their joint influence on mortality: the Framingham Heart Study. Circulation. 2003; 107:2920–2925.4. Go AS, Hylek EM, Phillips KA, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001; 285:2370–2375.5. Miyasaka Y, Barnes ME, Gersh BJ, et al. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 2006; 114:119–125.6. Lloyd-Jones DM, Wang TJ, Leip EP, et al. Lifetime risk for development of atrial fibrillation: the Framingham Heart Study. Circulation. 2004; 110:1042–1046.7. Heeringa J, van der Kuip DA, Hofman A, et al. Prevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam study. Eur Heart J. 2006; 27:949–953.8. Son MK, Lim NK, Cho MC, Park HY, Incidence and. the National Health Insurance Service Database (2002-2010). Korean Circ J. 2016; 46:515–521.9. Lee KS, Choi SJ, Park SH, Kim HL, Min H, Park HY. Prevalence of atrial fibrillation in middle-aged people in Korea: The Korean Genome and Epidemiology Study. Korean Circ J. 2008; 38:601–605.10. Coyne KS, Paramore C, Grandy S, Mercader M, Reynolds M, Zimetbaum P. Assessing the direct costs of treating nonvalvular atrial fibrillation in the United States. Value Health. 2006; 9:348–356.11. Stewart S, Murphy NF, Walker A, McGuire A, McMurray JJ. Cost of an emerging epidemic: an economic analysis of atrial fibrillation in the UK. Heart. 2004; 90:286–292.12. Lee WC, Lamas GA, Balu S, Spalding J, Wang Q, Pashos CL. Direct treatment cost of atrial fibrillation in the elderly American population: a Medicare perspective. J Med Econ. 2008; 11:281–298.13. Kim MH, Johnston SS, Chu BC, Dalal MR, Schulman KL. Estimation of total incremental health care costs in patients with atrial fibrillation in the United States. Circ Cardiovasc Qual Outcomes. 2011; 4:313–320.14. Chen SJ, Liu CJ, Chao TF, et al. Dental scaling and atrial fibrillation: a nationwide cohort study. Int J Cardiol. 2013; 168:2300–2303.15. Chao TF, Liu CJ, Tuan TC, et al. Rate-control treatment and mortality in atrial fibrillation. Circulation. 2015; 132:1604–1612.16. Wong CX, Brooks AG, Leong DP, Roberts-Thomson KC, Sanders P. The increasing burden of atrial fibrillation compared with heart failure and myocardial infarction: a 15-year study of all hospitalizations in Australia. Arch Intern Med. 2012; 172:739–741.17. Wattigney WA, Mensah GA, Croft JB. Increasing trends in hospitalization for atrial fibrillation in the United States, 1985 through 1999: implications for primary prevention. Circulation. 2003; 108:711–716.18. Ogilvie IM, Newton N, Welner SA, Cowell W, Lip GY. Underuse of oral anticoagulants in atrial fibrillation: a systematic review. Am J Med. 2010; 123:638–645.19. Cherubini A, Corsonello A, Lattanzio F. Underprescription of beneficial medicines in older people: causes, consequences and prevention. Drugs Aging. 2012; 29:463–475.20. Go AS, Hylek EM, Borowsky LH, Phillips KA, Selby JV, Singer DE. Warfarin use among ambulatory patients with nonvalvular atrial fibrillation: the anticoagulation and risk factors in atrial fibrillation (ATRIA) study. Ann Intern Med. 1999; 131:927–934.21. Mant J, Hobbs FD, Fletcher K, et al. Warfarin versus aspirin for stroke prevention in an elderly community population with atrial fibrillation (the Birmingham Atrial Fibrillation Treatment of the Aged Study, BAFTA): a randomised controlled trial. Lancet. 2007; 370:493–503.22. Turakhia MP, Santangeli P, Winkelmayer WC, et al. Increased mortality associated with digoxin in contemporary patients with atrial fibrillation: findings from the TREAT-AF study. J Am Coll Cardiol. 2014; 64:660–668.23. Chugh SS, Havmoeller R, Narayanan K, et al. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation. 2014; 129:837–847.24. Patel NJ, Deshmukh A, Pant S, et al. Contemporary trends of hospitalization for atrial fibrillation in the United States, 2000 through 2010: implications for healthcare planning. Circulation. 2014; 129:2371–2379.25. Page RL, Joglar JA, Caldwell MA, et al. 2015 ACC/AHA/HRS Guideline for the Management of Adult Patients With Supraventricular Tachycardia: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2016; 67:e27–e115.26. Jung BC, Kim NH, Nam GB, et al. The Korean Heart Rhythm Society’s 2014 Statement on Antithrombotic Therapy for Patients with Nonvalvular Atrial Fibrillation: Korean Heart Rhythm Society. Korean Circ J. 2015; 45:9–19.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pathophysiology and Diagnosis in Atrial Fibrillation
- Pharmacological Treatment of Atrial Fibrillation
- Non-medication Treatment of Atrial Fibrillation
- Resolution of atrial fibrillation with induction of general anesthesia: A case report
- A Concealed Brugada Electrocardiogram Pattern Revealed after Administering Propafenone to a Patient with Atrial Fibrillation