J Clin Neurol.
2016 Jan;12(1):34-41. 10.3988/jcn.2016.12.1.34.
Adherence to Guidelines for Antithrombotic Therapy in Patients with Atrial Fibrillation According to CHADS2 Score before and after Stroke: A Multicenter Observational Study from Korea
- Affiliations
-
- 1Department of Neurology, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea.
- 2Department of Neurology, Eulji General Hospital, Eulji University, Seoul, Korea.
- 3Department of Neurology, Ilsan Paik Hospital, Inje University, Goyang, Korea.
- 4Department of Neurology, Eulji University Hospital, Eulji University, Daejeon, Korea.
- 5Department of Neurology, Soonchunhyang University College of Medicine, Seoul, Korea.
- 6Department of Neurology, Seoul Medical Center, Seoul, Korea.
- 7Department of Neurology, Yeungnam University Hospital, Daegu, Korea.
- 8Department of Neurology, College of Medicine, Dong-A University, Busan, Korea.
- 9Department of Neurology, Hallym University College of Medicine, Anyang, Korea.
- 10Department of Biostatistics, Korea University College of Medicine, Seoul, Korea.
- 11Department of Biostatistics, Clinical Research Center, Asan Medical Center, Seoul, Korea.
- 12Department of Neurology, Cerebrovascular Center, Seoul National University Bundang Hospital, Seongnam, Korea. braindoc@snu.ac.kr
- KMID: 2364917
- DOI: http://doi.org/10.3988/jcn.2016.12.1.34
Abstract
- BACKGROUND AND PURPOSE
A substantial proportion of patients with atrial fibrillation (AF) are not treated optimally; however, the inappropriateness of drug therapy has never been evaluated before or after a stroke event. We investigated the adherence to guidelines for therapy in AF patients hospitalized with acute ischemic stroke (AIS) before stroke onset and at discharge, with the aim of identifying the factors associated with inappropriate therapy.
METHODS
AIS patients with AF hospitalized within 7 days of onset were identified from a prospective nine-center stroke registry database. Two cohorts were defined: patients diagnosed with AF prior to the stroke event (admission cohort) and patients diagnosed with AF at discharge from hospital (discharge cohort). Any of the following conditions were regarded as nonadherence to guidelines in this study: use of anticoagulant or nonuse of antithrombotics with CHADS2 score=0, nonuse of antithrombotics with CHADS2 score=1, or nonuse of anticoagulant with CHADS2 score > or =2.
RESULTS
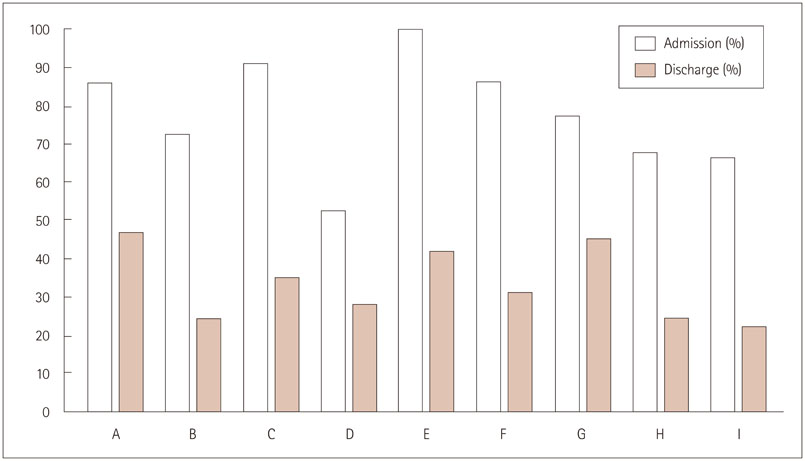
Overall, 406 patients were enrolled in the admission cohort and 518 in the discharge cohort. The rates of nonadherence before a stroke event and at discharge were 77.8% and 33.3%, respectively. These rates varied widely for both cohorts, with interhospital differences being statistically significant. Multivariable analysis revealed that old age, stroke history, and congestive heart failure were associated with nonadherence before stroke. At discharge, males, coronary heart disease, inappropriate antithrombotic use before stroke, and functional disability at discharge were associated with nonadherence.
CONCLUSIONS
This study shows that antithrombotic use in AIS patients with AF might be not optimal before and after stroke in Korea.
MeSH Terms
Figure
Reference
-
1. Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010; 137:263–272.
Article2. Singer DE, Albers GW, Dalen JE, Fang MC, Go AS, Halperin JL, et al. Antithrombotic therapy in atrial fibrillation: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008; 133:6 Suppl. 546S–592S.3. Fuster V, Rydén LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, et al. ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. 2006; 114:e257–e354.4. Clinical Research Center for Stroke. Clinical Practice Guidelines for Stroke. Revision. Seoul: Clinical Research Center for Stroke;2013. Available from: http://www.stroke.or.kr/image/CPGStrok(English)20130730.pdf.5. Goldstein LB, Bushnell CD, Adams RJ, Appel LJ, Braun LT, Chaturvedi S, et al. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/ American Stroke Association. Stroke. 2011; 42:517–584.6. ACTIVE Writing Group of the ACTIVE Investigators. Connolly S, Pogue J, Hart R, Pfeffer M, Hohnloser S, et al. Clopidogrel plus aspirin versus oral anticoagulation for atrial fibrillation in the Atrial fibrillation Clopidogrel Trial with Irbesartan for prevention of Vascular Events (ACTIVE W): a randomised controlled trial. Lancet. 2006; 367:1903–1912.
Article7. van Walraven C, Hart RG, Singer DE, Laupacis A, Connolly S, Petersen P, et al. Oral anticoagulants vs aspirin in nonvalvular atrial fibrillation: an individual patient meta-analysis. JAMA. 2002; 288:2441–2448.
Article8. van Walraven C, Hart RG, Connolly S, Austin PC, Mant J, Hobbs FD, et al. Effect of age on stroke prevention therapy in patients with atrial fibrillation: the atrial fibrillation investigators. Stroke. 2009; 40:1410–1416.
Article9. Kowey PR, Reiffel JA, Myerburg R, Naccarelli GV, Packer DL, Pratt CM, et al. Warfarin and aspirin use in atrial fibrillation among practicing cardiologist (from the AFFECTS Registry). Am J Cardiol. 2010; 105:1130–1134.
Article10. Friberg L, Hammar N, Ringh M, Pettersson H, Rosenqvist M. Stroke prophylaxis in atrial fibrillation: who gets it and who does not? Report from the Stockholm Cohort-study on Atrial Fibrillation (SCAF-study). Eur Heart J. 2006; 27:1954–1964.11. Monte S, Macchia A, Pellegrini F, Romero M, Lepore V, D'Ettorre A, et al. Antithrombotic treatment is strongly underused despite reducing overall mortality among high-risk elderly patients hospitalized with atrial fibrillation. Eur Heart J. 2006; 27:2217–2223.
Article12. Hylek EM, D'Antonio J, Evans-Molina C, Shea C, Henault LE, Regan S. Translating the results of randomized trials into clinical practice: the challenge of warfarin candidacy among hospitalized elderly patients with atrial fibrillation. Stroke. 2006; 37:1075–1080.
Article13. Gladstone DJ, Bui E, Fang J, Laupacis A, Lindsay MP, Tu JV, et al. Potentially preventable strokes in high-risk patients with atrial fibrillation who are not adequately anticoagulated. Stroke. 2009; 40:235–240.
Article14. Schwammenthal Y, Bornstein NM, Goldbourt U, Koton S, Schwartz R, Koren-Morag N, et al. Anticoagulation remains underused in prevention of stroke associated with atrial fibrillation: insights from two consecutive national surveys. Int J Cardiol. 2011; 152:356–361.
Article15. Kim BJ, Han MK, Park TH, Park SS, Lee KB, Lee BC, et al. Current status of acute stroke management in Korea: a report on a multicenter, comprehensive acute stroke registry. Int J Stroke. 2014; 9:514–518.
Article16. Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA. 2001; 285:2864–2870.
Article17. Hart RG, Pearce LA. Current status of stroke risk stratification in patients with atrial fibrillation. Stroke. 2009; 40:2607–2610.
Article18. Ahmad O, Ahmad KE, Dear KB, Harvey I, Hughes A, Lueck CJ. Atrial fibrillation and anticoagulation in a stroke unit population. Intern Med J. 2009; 39:752–756.
Article19. Gandolfo C, Balestrino M, Burrone A, Del Sette M, Finocchi C. Stroke due to atrial fibrillation and the attitude to prescribing anticoagulant prevention in Italy. A prospective study of a consecutive stroke population admitted to a comprehensive stroke unit. J Neurol. 2008; 255:796–802.
Article20. Sun MC, Hsiao PJ. In-hospital case management to increase anticoagulation therapy for stroke patients with atrial fibrillation: a hospital-based registry. J Formos Med Assoc. 2013; 112:263–268.
Article21. Lopes RD, Shah BR, Olson DM, Zhao X, Pan W, Bushnell CD, et al. Antithrombotic therapy use at discharge and 1 year in patients with atrial fibrillation and acute stroke: results from the AVAIL Registry. Stroke. 2011; 42:3477–3483.
Article22. Srivastava A, Hudson M, Hamoud I, Cavalcante J, Pai C, Kaatz S. Examining warfarin underutilization rates in patients with atrial fibrillation: detailed chart review essential to capture contraindications to warfarin therapy. Thromb J. 2008; 6:6.
Article23. Meiltz A, Zimmermann M, Urban P, Bloch A. Association of Cardiologists of the Canton of Geneva. Atrial fibrillation management by practice cardiologists: a prospective survey on the adherence to guidelines in the real world. Europace. 2008; 10:674–680.
Article24. Nieuwlaat R, Capucci A, Lip GY, Olsson SB, Prins MH, Nieman FH, et al. Antithrombotic treatment in real-life atrial fibrillation patients: a report from the Euro Heart Survey on Atrial Fibrillation. Eur Heart J. 2006; 27:3018–3026.
Article25. Atarashi H, Inoue H, Okumura K, Yamashita T, Kumagai N, Origasa H. J-RHYTHM Registry Investigators. Present status of anticoagulation treatment in Japanese patients with atrial fibrillation: a report from the J-RHYTHM Registry. Circ J. 2011; 75:1328–1333.
Article26. Barnes GD, Kaatz S, Winfield J, Gu X, Haymart B, Kline-Rogers E, et al. Warfarin use in atrial fibrillation patients at low risk for stroke: analysis of the Michigan Anticoagulation Quality Improvement Initiative [MAQI (2)]. J Thromb Thrombolysis. 2014; 37:171–176.
Article27. Fuster V, Rydén LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, et al. 2011 ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2011; 123:e269–e367.28. Partington SL, Abid S, Teo K, Oczkowski W, O'Donnell MJ. Pre-admission warfarin use in patients with acute ischemic stroke and atrial fibrillation: the appropriate use and barriers to oral anticoagulant therapy. Thromb Res. 2007; 120:663–669.
Article29. Deplanque D, Leys D, Parnetti L, Schmidt R, Ferro J, de Reuck J, et al. Secondary prevention of stroke in patients with atrial fibrillation: factors influencing the prescription of oral anticoagulation at discharge. Cerebrovasc Dis. 2006; 21:372–379.
Article30. You JJ, Singer DE, Howard PA, Lane DA, Eckman MH, Fang MC, et al. Antithrombotic therapy for atrial fibrillation: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012; 141:2 Suppl. e531S–e575S.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antithrombotic Therapy for Patients with Nonvalvular Atrial Fibrillation
- Practical Issues to Prevent Stroke Associated with Non-valvular Atrial Fibrillation
- The Korean Heart Rhythm Society's 2014 Statement on Antithrombotic Therapy for Patients with Nonvalvular Atrial Fibrillation: Korean Heart Rhythm Society
- Impact of CHADS2 Score on Neurological Severity and Long-Term Outcome in Atrial Fibrillation-Related Ischemic Stroke
- The Mechanism of and Preventive Therapy for Stroke in Patients with Atrial Fibrillation