J Cardiovasc Ultrasound.
2016 Dec;24(4):317-323. 10.4250/jcu.2016.24.4.317.
Redefining Effusive-Constrictive Pericarditis with Echocardiography
- Affiliations
-
- 1Division of Cardiology, Department of Medicine, Faculty of Medicine and Health Sciences, Stellenbosch University and Tygerberg Academic Hospital, Parow, South Africa. pieter.vanderbijl@gmail.com
- KMID: 2364650
- DOI: http://doi.org/10.4250/jcu.2016.24.4.317
Abstract
- BACKGROUND
Effusive-constrictive pericarditis (ECP) is traditionally diagnosed by using the expensive and invasive technique of direct pressure measurements in the pericardial space and the right atrium. The aim of this study was to assess the diagnostic role of echocardiography in tuberculous ECP.
METHODS
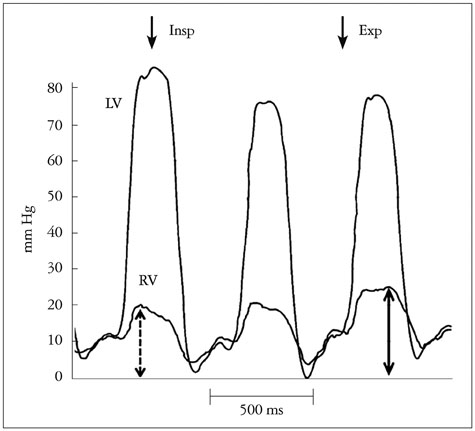
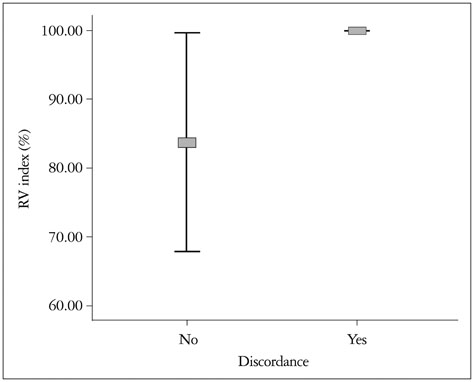
Intrapericardial and right atrial pressures were measured pre- and post-pericardiocentesis, and right ventricular and left ventricular pressures were measured post-pericardiocentesis in patients with tuberculous pericardial effusions. Echocardiography was performed post-pericardiocentesis. Traditional, pressure-based diagnostic criteria were compared with post-pericardiocentesis systolic discordance and echocardiographic evidence of constriction.
RESULTS
Thirty-two patients with tuberculous pericardial disease were included. Sixteen had ventricular discordance (invasively measured), 16 had ECP as measured by intrapericardial and right atrial invasive pressure measurements and 17 had ECP determined echocardiographically. The sensitivity and specificity of pressure-guided measurements (compared with discordance) for the diagnosis of ECP were both 56%. The positive and negative predictive values were both 56%. The sensitivity of echocardiography (compared with discordance) for the diagnosis of ECP was 81% and the specificity 75%, while the positive and the negative predictive values were 76% and 80%, respectively.
CONCLUSION
Echocardiography shows a better diagnostic performance than invasive, pressure-based measurements for the diagnosis of ECP when both these techniques are compared with the gold standard of invasively measured systolic discordance.
Keyword
MeSH Terms
Figure
Reference
-
1. Hancock EW. A clearer view of effusive-constrictive pericarditis. N Engl J Med. 2004; 350:435–437.2. Hancock EW. Subacute effusive-constrictive pericarditis. Circulation. 1971; 43:183–192.3. Cameron J, Oesterle SN, Baldwin JC, Hancock EW. The etiologic spectrum of constrictive pericarditis. Am Heart J. 1987; 113(2 Pt 1):354–360.4. Sagristà-Sauleda J, Angel J, Sánchez A, Permanyer-Miralda G, Soler-Soler J. Effusive-constrictive pericarditis. N Engl J Med. 2004; 350:469–475.5. Ntsekhe M, Matthews K, Syed FF, Deffur A, Badri M, Commerford PJ, Gersh BJ, Wilkinson KA, Wilkinson RJ, Mayosi BM. Prevalence, hemodynamics, and cytokine profile of effusive-constrictive pericarditis in patients with tuberculous pericardial effusion. PLoS One. 2013; 8:e77532.6. Ntsekhe M, Shey Wiysonge C, Commerford PJ, Mayosi BM. The prevalence and outcome of effusive constrictive pericarditis: a systematic review of the literature. Cardiovasc J Afr. 2012; 23:281–285.7. Zagol B, Minderman D, Munir A, D'Cruz I. Effusive constrictive pericarditis: 2D, 3D echocardiography and MRI imaging. Echocardiography. 2007; 24:1110–1114.8. Syed FF, Ntsekhe M, Mayosi BM, Oh JK. Effusive-constrictive pericarditis. Heart Fail Rev. 2013; 18:277–287.9. Oh JK, Tajik AJ, Appleton CP, Hatle LK, Nishimura RA, Seward JB. Preload reduction to unmask the characteristic Doppler features of constrictive pericarditis. A new observation. Circulation. 1997; 95:796–799.10. Boonyaratavej S, Oh JK, Tajik AJ, Appleton CP, Seward JB. Comparison of mitral inflow and superior vena cava Doppler velocities in chronic obstructive pulmonary disease and constrictive pericarditis. J Am Coll Cardiol. 1998; 32:2043–2048.11. Dal-Bianco JP, Sengupta PP, Mookadam F, Chandrasekaran K, Tajik AJ, Khandheria BK. Role of echocardiography in the diagnosis of constrictive pericarditis. J Am Soc Echocardiogr. 2009; 22:24–33. quiz 103-4.12. Reuter H, Burgess L, van Vuuren W, Doubell A. Diagnosing tuberculous pericarditis. QJM. 2006; 99:827–839.13. Hurrell DG, Nishimura RA, Higano ST, Appleton CP, Danielson GK, Holmes DR Jr, Tajik AJ. Value of dynamic respiratory changes in left and right ventricular pressures for the diagnosis of constrictive pericarditis. Circulation. 1996; 93:2007–2013.14. Badri M, Wilson D, Wood R. Effect of highly active antiretroviral therapy on incidence of tuberculosis in South Africa: a cohort study. Lancet. 2002; 359:2059–2064.15. Shabetai R. The pericardium. Boston: Kluwer Academic Publishers;2003.16. Nagueh SF, Kopelen HA, Zoghbi WA. Relation of mean right atrial pressure to echocardiographic and Doppler parameters of right atrial and right ventricular function. Circulation. 1996; 93:1160–1169.17. Kusunose K, Dahiya A, Popović ZB, Motoki H, Alraies MC, Zurick AO, Bolen MA, Kwon DH, Flamm SD, Klein AL. Biventricular mechanics in constrictive pericarditis comparison with restrictive cardiomyopathy and impact of pericardiectomy. Circ Cardiovasc Imaging. 2013; 6:399–406.18. Talreja DR, Nishimura RA, Oh JK, Holmes DR. Constrictive pericarditis in the modern era: novel criteria for diagnosis in the cardiac catheterization laboratory. J Am Coll Cardiol. 2008; 51:315–319.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Effusive-Constrictive Pericarditis in and Infant Treated by Pericardiectomy
- Clinical Studies on Acute Pericarditis with Effusion and Chronic Constrictive Pericarditis with or without Effusion
- Postoperative Effusive Constrictive Pericarditis in Ventricular Septal Defect Repair
- Recurrent Postoperative Effusive-Constrictive Pericarditis Associated with Steroid Discontinuation
- Echocardiographic Evaluation of Constrictive Pericarditis