J Cardiovasc Ultrasound.
2016 Dec;24(4):294-302. 10.4250/jcu.2016.24.4.294.
Epicardial Fat Thickness and Neutrophil to Lymphocyte Ratio are Increased in Non-Dipper Hypertensive Patients
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Kosin University College of Medicine, Busan, Korea. kyoungim74@gmail.com
- KMID: 2364647
- DOI: http://doi.org/10.4250/jcu.2016.24.4.294
Abstract
- BACKGROUND
In this study, we aimed to investigate the relationship between echocardiographic epicardial fat thickness (EFT), neutrophil to lymphocyte ratio (NLR; an important inflammatory marker), and diurnal blood pressure (BP) changes in patients with recently diagnosed essential hypertension.
METHODS
A total of 647 patients underwent echocardiography and 24 hours of ambulatory BP monitoring. EFT was measured by echocardiography, while NLR was measured by dividing the neutrophil count by the lymphocyte count. Patients were categorized into three groups according to BP pattern: the normotensive group, the dipper group, and the non-dipper group.
RESULTS
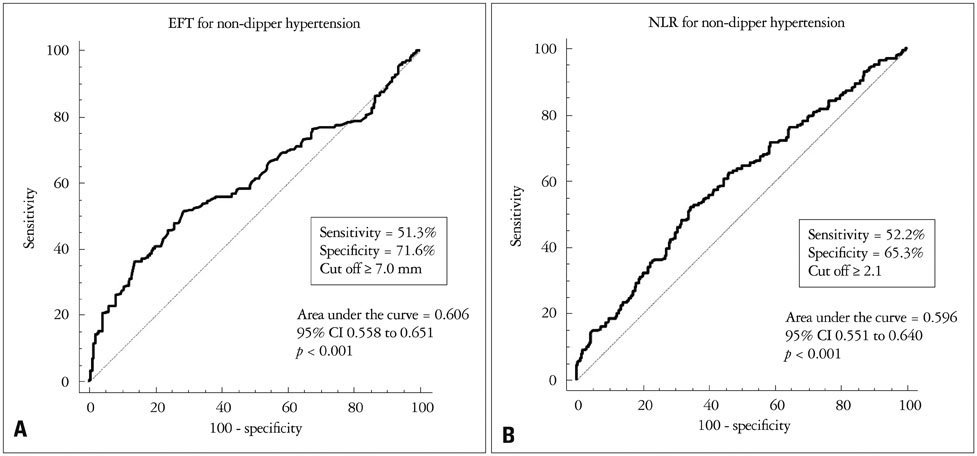
The mean EFT was highest in the non-dipper group (non-dipper group, 7.3 ± 3.0 mm; dipper group, 6.1 ± 2.0 mm; control group, 5.6 ± 2.0 mm; p < 0.001). NLR was also highest in the non-dipper group (non-dipper, 2.75 ± 2.81; dipper, 2.01 ± 1.32; control, 1.92 ± 1.11; p < 0.001). EFT was significantly correlated with age (r = 0.160, p < 0.001) and NLR (r = 0.353, p < 0.001). Furthermore, an EFT ≥ 7.0 mm was associated with the non-dipper BP pattern with 51.3% sensitivity and 71.6% specificity [95% confidence interval (CI) = 0.56-0.65, p < 0.001]. In a multivariate analysis, EFT [adjusted odds ratio (OR) = 3.99, 95% CI = 1.22-13.10, p = 0.022] and NLR (OR = 1.34, 95% CI = 1.05-1.71, p = 0.018) were independent parameters that distinguished a non-dipper pattern after adjustment for cardiovascular risk factors.
CONCLUSION
EFT and NLR are independently associated with impaired diurnal BP profiles in hypertensive individuals. EFT (as measured by echocardiography) and NLR appear to be helpful in stratifying cardiometabolic risk.
MeSH Terms
Figure
Reference
-
1. Verdecchia P, Schillaci G, Guerrieri M, Gatteschi C, Benemio G, Boldrini F, Porcellati C. Circadian blood pressure changes and left ventricular hypertrophy in essential hypertension. Circulation. 1990; 81:528–536.2. Cuspidi C, Macca G, Sampieri L, Fusi V, Severgnini B, Michev I, Salerno M, Magrini F, Zanchetti A. Target organ damage and non-dipping pattern defined by two sessions of ambulatory blood pressure monitoring in recently diagnosed essential hypertensive patients. J Hypertens. 2001; 19:1539–1545.3. Iacobellis G, Corradi D, Sharma AM. Epicardial adipose tissue: anatomic, biomolecular and clinical relationships with the heart. Nat Clin Pract Cardiovasc Med. 2005; 2:536–543.4. Shim IK, Cho KI, Kim HS, Heo JH, Cha TJ. Impact of gender on the association of epicardial fat thickness, obesity, and circadian blood pressure pattern in hypertensive patients. J Diabetes Res. 2015; 2015:924539.5. Dicker D, Atar E, Kornowski R, Bachar GN. Increased epicardial adipose tissue thickness as a predictor for hypertension: a cross-sectional observational study. J Clin Hypertens (Greenwich). 2013; 15:893–898.6. Mazurek T, Zhang L, Zalewski A, Mannion JD, Diehl JT, Arafat H, Sarov-Blat L, O’Brien S, Keiper EA, Johnson AG, Martin J, Goldstein BJ, Shi Y. Human epicardial adipose tissue is a source of inflammatory mediators. Circulation. 2003; 108:2460–2466.7. Cho KI, Ann SH, Singh GB, Her AY, Shin ES. Combined usefulness of the platelet-to-lymphocyte ratio and the neutrophil-to-lymphocyte ratio in predicting the long-term adverse events in patients who have undergone percutaneous coronary intervention with a drug-eluting stent. PLoS One. 2015; 10:e0133934.8. Fowler AJ, Agha RA. Neutrophil/lymphocyte ratio is related to the severity of coronary artery disease and clinical outcome in patients undergoing angiography--the growing versatility of NLR. Atherosclerosis. 2013; 228:44–45.9. Demir M. The relationship between neutrophil lymphocyte ratio and non-dipper hypertension. Clin Exp Hypertens. 2013; 35:570–573.10. Sunbul M, Gerin F, Durmus E, Kivrak T, Sari I, Tigen K, Cincin A. Neutrophil to lymphocyte and platelet to lymphocyte ratio in patients with dipper versus non-dipper hypertension. Clin Exp Hypertens. 2014; 36:217–221.11. O'Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, Clement D, de la Sierra A, de Leeuw P, Dolan E, Fagard R, Graves J, Head GA, Imai Y, Kario K, Lurbe E, Mallion JM, Mancia G, Mengden T, Myers M, Ogedegbe G, Ohkubo T, Omboni S, Palatini P, Redon J, Ruilope LM, Shennan A, Staessen JA, vanMontfrans G, Verdecchia P, Waeber B, Wang J, Zanchetti A, Zhang Y. European Society of Hypertension Working Group on Blood Pressure Monitoring. European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013; 31:1731–1768.12. Levy D, Savage DD, Garrison RJ, Anderson KM, Kannel WB, Castelli WP. Echocardiographic criteria for left ventricular hypertrophy: the Framingham Heart Study. Am J Cardiol. 1987; 59:956–960.13. Mahabadi AA, Massaro JM, Rosito GA, Levy D, Murabito JM, Wolf PA, O’Donnell CJ, Fox CS, Hoffmann U. Association of pericardial fat, intrathoracic fat, and visceral abdominal fat with cardiovascular disease burden: the Framingham Heart Study. Eur Heart J. 2009; 30:850–856.14. Sengul C, Duman D. The association of epicardial fat thickness with blunted heart rate recovery in patients with metabolic syndrome. Tohoku J Exp Med. 2011; 224:257–262.15. Rosito GA, Massaro JM, Hoffmann U, Ruberg FL, Mahabadi AA, Vasan RS, O’Donnell CJ, Fox CS. Pericardial fat, visceral abdominal fat, cardiovascular disease risk factors, and vascular calcification in a community-based sample: the Framingham Heart Study. Circulation. 2008; 117:605–613.16. Marchington JM, Mattacks CA, Pond CM. Adipose tissue in the mammalian heart and pericardium: structure, foetal development and biochemical properties. Comp Biochem Physiol B. 1989; 94:225–232.17. Manzella D, Barbieri M, Rizzo MR, Ragno E, Passariello N, Gambardella A, Marfella R, Giugliano D, Paolisso G. Role of free fatty acids on cardiac autonomic nervous system in noninsulin-dependent diabetic patients: effects of metabolic control. J Clin Endocrinol Metab. 2001; 86:2769–2774.18. Bambace C, Telesca M, Zoico E, Sepe A, Olioso D, Rossi A, Corzato F, Di Francesco V, Mazzucco A, Santini F, Zamboni M. Adiponectin gene expression and adipocyte diameter: a comparison between epicardial and subcutaneous adipose tissue in men. Cardiovasc Pathol. 2011; 20:e153–e156.19. Iacobellis G, Barbaro G. The double role of epicardial adipose tissue as proand anti-inflammatory organ. Horm Metab Res. 2008; 40:442–445.20. Mazurek T, Kiliszek M, Kobylecka M, Skubisz-Głuchowska J, Kochman J, Filipiak K, Królicki L, Opolski G. Relation of proinflammatory activity of epicardial adipose tissue to the occurrence of atrial fibrillation. Am J Cardiol. 2014; 113:1505–1508.21. Batal O, Schoenhagen P, Shao M, Ayyad AE, Van Wagoner DR, Halliburton SS, Tchou PJ, Chung MK. Left atrial epicardial adiposity and atrial fibrillation. Circ Arrhythm Electrophysiol. 2010; 3:230–236.22. Kaya H, Ertaş F, Soydinç MS. Association between neutrophil to lymphocyte ratio and severity of coronary artery disease. Clin Appl Thromb Hemost. 2014; 20:221.23. Papa A, Emdin M, Passino C, Michelassi C, Battaglia D, Cocci F. Predictive value of elevated neutrophil-lymphocyte ratio on cardiac mortality in patients with stable coronary artery disease. Clin Chim Acta. 2008; 395:27–31.24. Kim BJ, Cho SH, Cho KI, Kim HS, Heo JH, Cha TJ. The combined impact of neutrophil-to-lymphocyte ratio and type 2 diabetic mellitus on significant coronary artery disease and carotid artery atherosclerosis. J Cardiovasc Ultrasound. 2016; 24:115–122.25. Gibson PH, Cuthbertson BH, Croal BL, Rae D, El-Shafei H, Gibson G, Jeffrey RR, Buchan KG, Hillis GS. Usefulness of neutrophil/lymphocyte ratio as predictor of new-onset atrial fibrillation after coronary artery bypass grafting. Am J Cardiol. 2010; 105:186–191.26. Cavalcante JL, Tamarappoo BK, Hachamovitch R, Kwon DH, Alraies MC, Halliburton S, Schoenhagen P, Dey D, Berman DS, Marwick TH. Association of epicardial fat, hypertension, subclinical coronary artery disease, and metabolic syndrome with left ventricular diastolic dysfunction. Am J Cardiol. 2012; 110:1793–1798.27. Sengul C, Cevik C, Ozveren O, Duman D, Eroglu E, Oduncu V, Tanboga HI, Can MM, Akgun T, Dindar I. Epicardial fat thickness is associated with non-dipper blood pressure pattern in patients with essential hypertension. Clin Exp Hypertens. 2012; 34:165–170.28. Della Mea P, Lupia M, Bandolin V, Guzzon S, Sonino N, Vettor R, Fallo F. Adiponectin, insulin resistance, and left ventricular structure in dipper and nondipper essential hypertensive patients. Am J Hypertens. 2005; 18:30–35.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Relation of Epicardial Fat Thickness, Neutrophil to Lymphocyte Ratio and Circadian Rhythm of Blood Pressure
- Association among epicardial fat, heart rate recovery and circadian blood pressure variability in patients with hypertension
- Left Ventricular Geometric Patterns of Dippers and Non-Dippers in Essential Hypertension
- Clinical Significance of Preoperative Inflammatory Parameters in Gastric Cancer Patients
- Echocardiographic Epicardial Fat Thickness on Short Term Prognosis in Patients with Acute Coronary Syndrome