Korean J Physiol Pharmacol.
2016 Nov;20(6):657-667. 10.4196/kjpp.2016.20.6.657.
Increasing injection frequency enhances the survival of injected bone marrow derived mesenchymal stem cells in a critical limb ischemia animal model
- Affiliations
-
- 1Cardiology, Gachon University Gil Medical Center, Incheon 21565, Korea.
- 2Department of Anatomy and Cell Biology, Graduate School of Medicine, Gachon University, Incheon 21936, Korea. khbyun1@gachon.ac.kr
- 3Functional Cellular Networks Laboratory, Lee Gil Ya Cancer and Diabetes Institute, Gachon University, Incheon 21999, Korea.
- KMID: 2364270
- DOI: http://doi.org/10.4196/kjpp.2016.20.6.657
Abstract
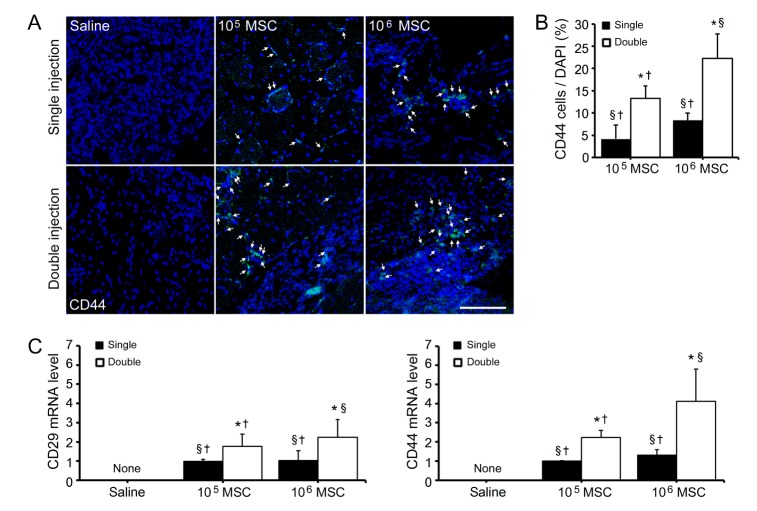
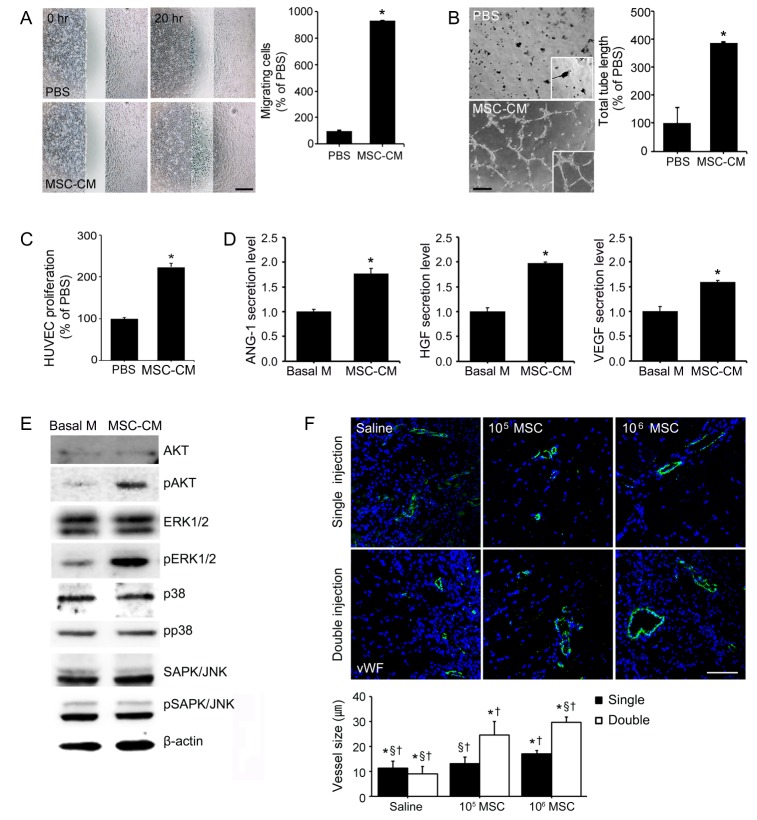
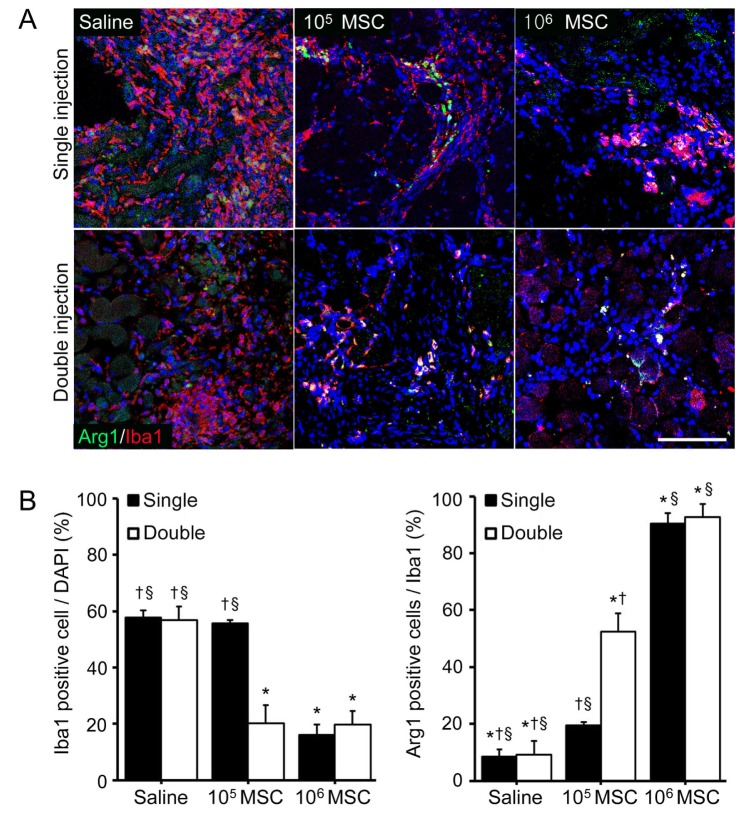
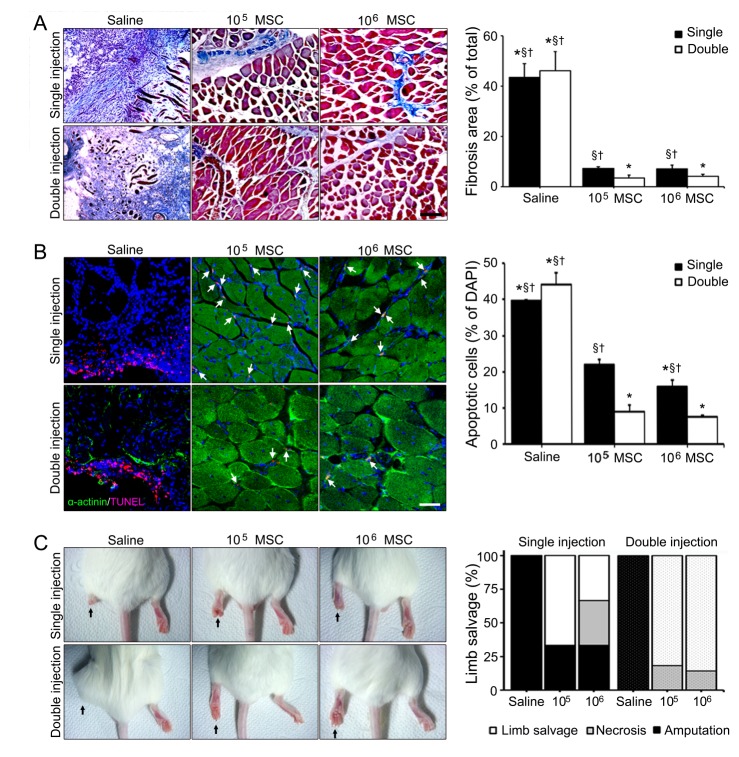
- Critical limb ischemia (CLI) is one of the most severe forms of peripheral artery diseases, but current treatment strategies do not guarantee complete recovery of vascular blood flow or reduce the risk of mortality. Recently, human bone marrow derived mesenchymal stem cells (MSCs) have been reported to have a paracrine influence on angiogenesis in several ischemic diseases. However, little evidence is available regarding optimal cell doses and injection frequencies. Thus, the authors undertook this study to investigate the effects of cell dose and injection frequency on cell survival and paracrine effects. MSCs were injected at 10ⶠor 10ⵠper injection (high and low doses) either once (single injection) or once in two consecutive weeks (double injection) into ischemic legs. Mice were sacrificed 4 weeks after first injection. Angiogenic effects were confirmed in vitro and in vivo, and M2 macrophage infiltration into ischemic tissues and rates of limb salvage were documented. MSCs were found to induce angiogenesis through a paracrine effect in vitro, and were found to survive in ischemic muscle for up to 4 weeks dependent on cell dose and injection frequency. In addition, double high dose and low dose of MSC injections increased vessel formation, and decreased fibrosis volumes and apoptotic cell numbers, whereas a single high dose did not. Our results showed MSCs protect against ischemic injury in a paracrine manner, and suggest that increasing injection frequency is more important than MSC dosage for the treatment CLI.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Evaluation of Human MSCs Treatment Frequency on Airway Inflammation in a Mouse Model of Acute Asthma
Jung Hur, Ji Young Kang, Young Kyoon Kim, Sook Young Lee, Sora Jeon, Yourha Kim, Chan Kwon Jung, Chin Kook Rhee
J Korean Med Sci. 2020;35(23):e188. doi: 10.3346/jkms.2020.35.e188.
Reference
-
1. Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG, Bell K, Caporusso J, Durand-Zaleski I, Komori K, Lammer J, Liapis C, Novo S, Razavi M, Robbs J, Schaper N, Shigematsu H, Sapoval M, White C, White J, Clement D, Creager M, Jaff M, Mohler E 3rd, Rutherford RB, Sheehan P, Sillesen H, Rosenfield K. TASC II Working Group. Inter-society consensus for the management of peripheral arterial disease (TASC II). Eur J Vasc Endovasc Surg. 2007; 33(Suppl 1):S1–S75. PMID: 17140820.
Article2. Furie B, Furie BC. Thrombus formation in vivo. J Clin Invest. 2005; 115:3355–3362. PMID: 16322780.
Article3. Barani J, Nilsson JA, Mattiasson I, Lindblad B, Gottsäter A. Inflammatory mediators are associated with 1-year mortality in critical limb ischemia. J Vasc Surg. 2005; 42:75–80. PMID: 16012455.
Article4. Lyden SP. Endovascular treatment of acute limb ischemia: review of current plasminogen activators and mechanical thrombectomy devices. Perspect Vasc Surg Endovasc Ther. 2010; 22:219–222. PMID: 21411460.
Article5. Kingsnorth A, Bowley D. Fundamentals of surgical practice: a preparation guide for the intercollegiate MRCS examination. 3rd ed. Leiden: Cambridge University Press;2011.6. Andaz S, Shields DA, Scurr JH, Smith PD. Thrombolysis in acute lower limb ischaemia. Eur J Vasc Surg. 1993; 7:595–603. PMID: 8270059.
Article7. Rosales OR, Mathewkutty S, Gnaim C. Drug eluting stents for below the knee lesions in patients with critical limb ischemia : longterm follow-up. Catheter Cardiovasc Interv. 2008; 72:112–115. PMID: 18412272.8. Cai L, Johnstone BH, Cook TG, Tan J, Fishbein MC, Chen PS, March KL. IFATS collection: human adipose tissue-derived stem cells induce angiogenesis and nerve sprouting following myocardial infarction, in conjunction with potent preservation of cardiac function. Stem Cells. 2009; 27:230–237. PMID: 18772313.
Article9. van Velthoven CT, Kavelaars A, Heijnen CJ. Mesenchymal stem cells as a treatment for neonatal ischemic brain damage. Pediatr Res. 2012; 71:474–481. PMID: 22430383.
Article10. Kawasaki K, Smith RS Jr, Hsieh CM, Sun J, Chao J, Liao JK. Activation of the phosphatidylinositol 3-kinase/protein kinase Akt pathway mediates nitric oxide-induced endothelial cell migration and angiogenesis. Mol Cell Biol. 2003; 23:5726–5737. PMID: 12897144.
Article11. Forte G, Minieri M, Cossa P, Antenucci D, Sala M, Gnocchi V, Fiaccavento R, Carotenuto F, De Vito P, Baldini PM, Prat M, Di Nardo P. Hepatocyte growth factor effects on mesenchymal stem cells: proliferation, migration, and differentiation. Stem Cells. 2006; 24:23–33. PMID: 16100005.
Article12. Kinnaird T, Stabile E, Burnett MS, Lee CW, Barr S, Fuchs S, Epstein SE. Marrow-derived stromal cells express genes encoding a broad spectrum of arteriogenic cytokines and promote in vitro and in vivo arteriogenesis through paracrine mechanisms. Circ Res. 2004; 94:678–685. PMID: 14739163.
Article13. Tang YL, Zhao Q, Zhang YC, Cheng L, Liu M, Shi J, Yang YZ, Pan C, Ge J, Phillips MI. Autologous mesenchymal stem cell transplantation induce VEGF and neovascularization in ischemic myocardium. Regul Pept. 2004; 117:3–10. PMID: 14687695.
Article14. Onda T, Honmou O, Harada K, Houkin K, Hamada H, Kocsis JD. Therapeutic benefits by human mesenchymal stem cells (hMSCs) and Ang-1 gene-modified hMSCs after cerebral ischemia. J Cereb Blood Flow Metab. 2008; 28:329–340. PMID: 17637706.
Article15. Li TS, Cheng K, Malliaras K, Smith RR, Zhang Y, Sun B, Matsushita N, Blusztajn A, Terrovitis J, Kusuoka H, Marbán L, Marbán E. Direct comparison of different stem cell types and subpopulations reveals superior paracrine potency and myocardial repair efficacy with cardiosphere-derived cells. J Am Coll Cardiol. 2012; 59:942–953. PMID: 22381431.
Article16. van Poll D, Parekkadan B, Borel Rinkes IHM, Tilles AW, Yarmush ML. Mesenchymal stem cell therapy for protection and repair of injured vital organs. Cell Mol Bioeng. 2008; 1:42–50.
Article17. Chen L, Tredget EE, Wu PY, Wu Y. Paracrine factors of mesenchymal stem cells recruit macrophages and endothelial lineage cells and enhance wound healing. PLoS One. 2008; 3:e1886. PMID: 18382669.
Article18. Selleri S, Bifsha P, Civini S, Pacelli C, Dieng MM, Lemieux W, Jin P, Bazin R, Patey N, Marincola FM, Moldovan F, Zaouter C, Trudeau LE, Benabdhalla B, Louis I, Beauséjour C, Stroncek D, Le Deist F, Haddad E. Human mesenchymal stromal cell-secreted lactate induces M2-macrophage differentiation by metabolic reprogramming. Oncotarget. 2016; 7:30193–30210. PMID: 27070086.
Article19. Yamada K, Uchiyama A, Uehara A, Perera B, Ogino S, Yokoyama Y, Takeuchi Y, Udey MC, Ishikawa O, Motegi S. MFG-E8 drives melanoma growth by stimulating mesenchymal stromal cell-induced angiogenesis and M2 polarization of tumor-associated macrophages. Cancer Res. 2016; 76:4283–4292. PMID: 27197197.
Article20. Jetten N, Verbruggen S, Gijbels MJ, Post MJ, De Winther MP, Donners MM. Anti-inflammatory M2, but not pro-inflammatory M1 macrophages promote angiogenesis in vivo. Angiogenesis. 2014; 17:109–118. PMID: 24013945.
Article21. Bergers G, Brekken R, McMahon G, Vu TH, Itoh T, Tamaki K, Tanzawa K, Thorpe P, Itohara S, Werb Z, Hanahan D. Matrix metalloproteinase-9 triggers the angiogenic switch during carcinogenesis. Nat Cell Biol. 2000; 2:737–744. PMID: 11025665.
Article22. Giraudo E, Inoue M, Hanahan D. An amino-bisphosphonate targets MMP-9-expressing macrophages and angiogenesis to impair cervical carcinogenesis. J Clin Invest. 2004; 114:623–633. PMID: 15343380.
Article23. Liew A, O'Brien T. Therapeutic potential for mesenchymal stem cell transplantation in critical limb ischemia. Stem Cell Res Ther. 2012; 3:28. PMID: 22846185.
Article24. Friedenstein AJ, Gorskaja JF, Kulagina NN. Fibroblast precursors in normal and irradiated mouse hematopoietic organs. Exp Hematol. 1976; 4:267–274. PMID: 976387.25. Zuk PA, Zhu M, Ashjian P, De Ugarte DA, Huang JI, Mizuno H, Alfonso ZC, Fraser JK, Benhaim P, Hedrick MH. Human adipose tissue is a source of multipotent stem cells. Mol Biol Cell. 2002; 13:4279–4295. PMID: 12475952.
Article26. Gluckman E, Broxmeyer HA, Auerbach AD, Friedman HS, Douglas GW, Devergie A, Esperou H, Thierry D, Socie G, Lehn P, et al. Hematopoietic reconstitution in a patient with Fanconi's anemia by means of umbilical-cord blood from an HLA-identical sibling. N Engl J Med. 1989; 321:1174–1178. PMID: 2571931.
Article27. Dominici M, Le Blanc K, Mueller I, Slaper-Cortenbach I, Marini F, Krause D, Deans R, Keating A, Prockop Dj, Horwitz E. The International Society for Cellular Therapy position statement. Minimal criteria for defining multipotent mesenchymal stromal cells. Cytotherapy. 2006; 8:315–317. PMID: 16923606.28. Satterthwaite AB, Burn TC, Le Beau MM, Tenen DG. Structure of the gene encoding CD34, a human hematopoietic stem cell antigen. Genomics. 1992; 12:788–794. PMID: 1374051.
Article29. Thomas ML. The leukocyte common antigen family. Annu Rev Immunol. 1989; 7:339–369. PMID: 2523715.
Article30. Zhang P, Dong L, Yan K, Long H, Yang TT, Dong MQ, Zhou Y, Fan QY, Ma BA. CXCR4-mediated osteosarcoma growth and pulmonary metastasis is promoted by mesenchymal stem cells through VEGF. Oncol Rep. 2013; 30:1753–1761. PMID: 23863999.
Article31. Bang OY, Lee JS, Lee PH, Lee G. Autologous mesenchymal stem cell transplantation in stroke patients. Ann Neurol. 2005; 57:874–882. PMID: 15929052.
Article32. Chen SL, Fang WW, Ye F, Liu YH, Qian J, Shan SJ, Zhang JJ, Chunhua RZ, Liao LM, Lin S, Sun JP. Effect on left ventricular function of intracoronary transplantation of autologous bone marrow mesenchymal stem cell in patients with acute myocardial infarction. Am J Cardiol. 2004; 94:92–95. PMID: 15219514.
Article33. Tateishi-Yuyama E, Matsubara H, Murohara T, Ikeda U, Shintani S, Masaki H, Amano K, Kishimoto Y, Yoshimoto K, Akashi H, Shimada K, Iwasaka T, Imaizumi T. Therapeutic angiogenesis for patients with limb ischaemia by autologous transplantation of bone-marrow cells: a pilot study and a randomised controlled trial. Lancet. 2002; 360:427–435. PMID: 12241713.
Article34. Sultan S, Hynes N. Critical appraisal of stem cell therapy in peripheral arterial disease: Do current scientific breakthroughs offer true promise or false hope? J Biomed Sci Eng. 2014; 7:75–85.
Article35. Lu D, Chen B, Liang Z, Deng W, Jiang Y, Li S, Xu J, Wu Q, Zhang Z, Xie B, Chen S. Comparison of bone marrow mesenchymal stem cells with bone marrow-derived mononuclear cells for treatment of diabetic critical limb ischemia and foot ulcer: a double-blind, randomized, controlled trial. Diabetes Res Clin Pract. 2011; 92:26–36. PMID: 21216483.
Article36. Lee HC, An SG, Lee HW, Park JS, Cha KS, Hong TJ, Park JH, Lee SY, Kim SP, Kim YD, Chung SW, Bae YC, Shin YB, Kim JI, Jung JS. Safety and effect of adipose tissue-derived stem cell implantation in patients with critical limb ischemia: a pilot study. Circ J. 2012; 76:1750–1760. PMID: 22498564.37. Gnecchi M, Zhang Z, Ni A, Dzau VJ. Paracrine mechanisms in adult stem cell signaling and therapy. Circ Res. 2008; 103:1204–1219. PMID: 19028920.
Article38. Olsson AK, Dimberg A, Kreuger J, Claesson-Welsh L. VEGF receptor signalling - in control of vascular function. Nat Rev Mol Cell Biol. 2006; 7:359–371. PMID: 16633338.
Article39. Cho DI, Kim MR, Jeong HY, Jeong HC, Jeong MH, Yoon SH, Kim YS, Ahn Y. Mesenchymal stem cells reciprocally regulate the M1/M2 balance in mouse bone marrow-derived macrophages. Exp Mol Med. 2014; 46:e70. PMID: 24406319.
Article40. Richards J, Gabunia K, Kelemen SE, Kako F, Choi ET, Autieri MV. Interleukin-19 increases angiogenesis in ischemic hind limbs by direct effects on both endothelial cells and macrophage polarization. J Mol Cell Cardiol. 2015; 79:21–31. PMID: 25450612.
Article41. Arnold L, Henry A, Poron F, Baba-Amer Y, van Rooijen N, Plonquet A, Gherardi RK, Chazaud B. Inflammatory monocytes recruited after skeletal muscle injury switch into antiinflammatory macrophages to support myogenesis. J Exp Med. 2007; 204:1057–1069. PMID: 17485518.
Article42. Bréchot N, Gomez E, Bignon M, Khallou-Laschet J, Dussiot M, Cazes A, Alanio-Bréchot C, Durand M, Philippe J, Silvestre JS, Van Rooijen N, Corvol P, Nicoletti A, Chazaud B, Germain S. Modulation of macrophage activation state protects tissue from necrosis during critical limb ischemia in thrombospondin-1-deficient mice. PLoS One. 2008; 3:e3950. PMID: 19079608.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Study of BD-MSC Therapy against Critical Limb Ischemia
- Therapeutic Angiogenesis with Somatic Stem Cell Transplantation
- The Role of Bone Marrow Mononuclear Cells in Angiogenesis in Mouse Hind Limb Ischemic Model
- Clinical Safety and Efficacy of Autologous Bone Marrow-Derived Mesenchymal Stem Cell Transplantation in Sensorineural Hearing Loss Patients
- Clinical Use of Mesenchymal Stem Cells in Bone Regeneration