J Korean Med Sci.
2017 Feb;32(2):335-342. 10.3346/jkms.2017.32.2.335.
Impact of the ASA Physical Status Score on Adjuvant Chemotherapy Eligibility and Survival of Upper Tract Urothelial Carcinoma Patients: a Multicenter Study
- Affiliations
-
- 1Department of Urology, Chungbuk National University College of Medicine, Cheongju, Korea. wjkim@chungbuk.ac.kr
- 2Department of Urology, Gangnam Severance Hospital, Urological Science Institute, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Urology, Kyungpook National University School of Medicine, Daegu, Korea.
- 4Department of Urology, Seoul National University Bundang Hospital, Seongnam, Korea.
- 5Department of Urology, Gyeongsang National University School of Medicine, Jinju, Korea.
- KMID: 2364180
- DOI: http://doi.org/10.3346/jkms.2017.32.2.335
Abstract
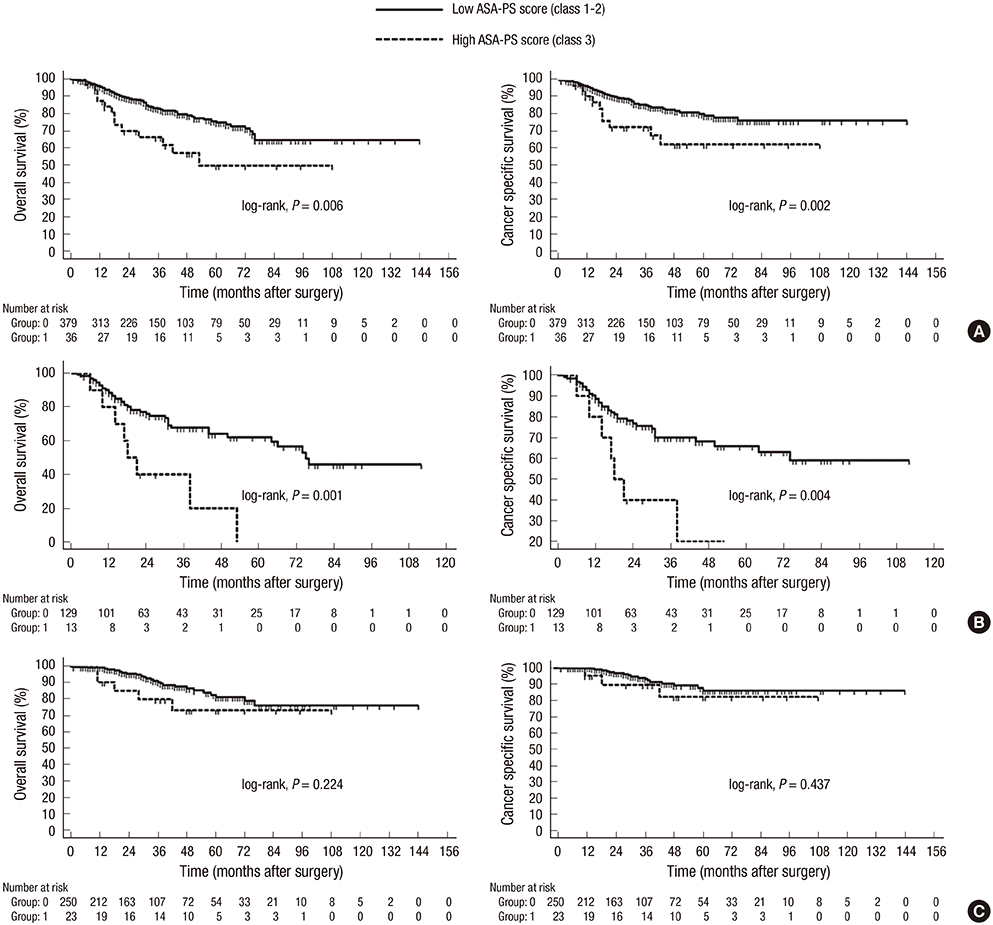
- The aim of the present multi-institutional study was to assess the influence of the American Society of Anesthesiologists Physical Status (ASA-PS) classification on adjuvant chemotherapy eligibility and survival in a multi-institutional cohort of patients treated with radical nephroureterectomy (RNU) for upper tract urothelial carcinoma (UTUC). We retrospectively reviewed data from 416 patients who underwent RNU for UTUC at four Korean institutions between 2001 and 2013. The ASA-PS classification was obtained from the anesthesia chart. Locally advanced UTUC was defined as ≥ pT3 and/or pN1 disease. The influence of ASA-PS score on survival was evaluated by Kaplan-Meier analyses and a multivariate Cox regression model. Patients with a higher ASA-PS class were less likely to be eligible for adjuvant chemotherapy in locally advanced UTUC (P = 0.016). Kaplan-Meier estimates showed that the high-risk ASA-PS group has a poorer overallsurvival (OS) and cancer-specific survival (CSS) compared to low risk ASA-PS groups in both the total and locally advanced UTUC cohorts. Based on multivariate Cox regression analysis, the high-risk ASA-PS category was an independent predictor for overall mortality (OM) (hazard ratio [HR], 1.919; 95% confidence interval [CI], 1.017-3.619; P = 0.044) and cancer-specific mortality (CSM) (HR, 2.120; 95% CI, 1.023-4.394; P = 0.043). In conclusion, high-risk ASA-PS score was independently associated with a lower survival rate in patients with UTUC after RNU. However, the influence of ASA-PS classification on survival was limited to locally advanced UTUC. The lower eligibility of patients in the high-risk ASA category for adjuvant chemotherapy may contribute to the lower survival rate in this group.
Keyword
MeSH Terms
Figure
Reference
-
1. Alva AS, Matin SF, Lerner SP, Siefker-Radtke AO. Perioperative chemotherapy for upper tract urothelial cancer. Nat Rev Urol. 2012; 9:266–273.2. Gayed BA, Thoreson GR, Margulis V. The role of systemic chemotherapy in management of upper tract urothelial cancer. Curr Urol Rep. 2013; 14:94–101.3. Kang HW, Jung HD, Ha YS, Kim TH, Kwon TG, Byun SS, Yun SJ, Kim WJ, Choi YD. Preoperative underweight patients with upper tract urothelial carcinoma survive less after radical nephroureterectomy. J Korean Med Sci. 2015; 30:1483–1489.4. Lin YK, Kaag M, Raman JD. Rationale and timing of perioperative chemotherapy for upper-tract urothelial carcinoma. Expert Rev Anticancer Ther. 2014; 14:543–551.5. Clark P, Agarwal N, Biagioli M. NCCN Clinical Practice Guidelines in Oncology: Bladder Cancer. Fort Washington, PA: National Comprehensive Cancer Network;2013.6. Fang D, Zhang Q, Li X, Qian C, Xiong G, Zhang L, Chen X, Zhang X, Yu W, He Z, et al. Nomogram predicting renal insufficiency after nephroureterectomy for upper tract urothelial carcinoma in the chinese population: exclusion of ineligible candidates for adjuvant chemotherapy. Biomed Res Int. 2014; 2014:529186.7. Xylinas E, Rink M, Margulis V, Clozel T, Lee RK, Comploj E, Novara G, Raman JD, Lotan Y, Weizer A, et al. Impact of renal function on eligibility for chemotherapy and survival in patients who have undergone radical nephro-ureterectomy. BJU Int. 2013; 112:453–461.8. Kawai K, Ichioka D, Inai H, Miyazaki J, Nishiyama H. Assessment and management of renal impairment in chemotherapy for urogenital cancer. Jpn J Clin Oncol. 2013; 43:1055–1063.9. Cullen DJ, Apolone G, Greenfield S, Guadagnoli E, Cleary P. ASA Physical Status and age predict morbidity after three surgical procedures. Ann Surg. 1994; 220:3–9.10. Miller TJ, Jeong HS, Davis K, Matthew A, Lysikowski J, Cho MJ, Reed G, Kenkel JM. Evaluation of the American Society of Anesthesiologists Physical Status classification system in risk assessment for plastic and reconstructive surgery patients. Aesthet Surg J. 2014; 34:448–456.11. Rouprêt M, Zigeuner R, Palou J, Boehle A, Kaasinen E, Sylvester R, Babjuk M, Oosterlinck W. European Association of Urology Guideline Group for urothelial cell carcinoma of the upper urinary tract. European guidelines for the diagnosis and management of upper urinary tract urothelial cell carcinomas: 2011 update. European Association of Urology Guideline Group for urothelial cell carcinoma of the upper urinary tract. Actas Urol Esp. 2012; 36:2–14.12. Greene FL. AJCC Cancer Staging Manual. 6th ed. New York, NY: Springer;2002.13. Epstein JI, Amin MB, Reuter VR, Mostofi FK. The World Health Organization/International Society of Urological Pathology consensus classification of urothelial (transitional cell) neoplasms of the urinary bladder. Bladder Consensus Conference Committee. Am J Surg Pathol. 1998; 22:1435–1448.14. Rouprêt M, Babjuk M, Compérat E, Zigeuner R, Sylvester R, Burger M, Cowan N, Böhle A, Van Rhijn BW, Kaasinen E, et al. European guidelines on upper tract urothelial carcinomas: 2013 update. Eur Urol. 2013; 63:1059–1071.15. Saklad M. Grading of patients for surgical procedures. Anesthesiology. 1941; 2:281–284.16. Wolters U, Wolf T, Stützer H, Schröder T. ASA classification and perioperative variables as predictors of postoperative outcome. Br J Anaesth. 1996; 77:217–222.17. Menke H, John KD, Klein A, Lorenz W, Junginger T. Preoperative risk assessment with the ASA classification. A prospective study of morbidity and mortality in various ASA classes in 2,937 patients in general surgery. Chirurg. 1992; 63:1029–1034.18. Mukkamala A, He C, Weizer AZ, Hafez KS, Miller DC, Montgomery JS, Wolf JS Jr. Long-term oncologic outcomes of minimally invasive partial nephrectomy for renal-cell carcinoma. J Endourol. 2014; 28:649–654.19. Froehner M, Koch R, Litz R, Heller A, Oehlschlaeger S, Wirth MP. Comparison of the American Society of Anesthesiologists Physical Status classification with the Charlson score as predictors of survival after radical prostatectomy. Urology. 2003; 62:698–701.20. Froehner M, Hentschel C, Koch R, Litz RJ, Hakenberg OW, Wirth MP. Which comorbidity classification best fits elderly candidates for radical prostatectomy? Urol Oncol. 2013; 31:461–467.21. Froehner M, Koch R, Litz RJ, Hakenberg OW, Oehlschlaeger S, Wirth MP. Interaction between age and comorbidity as predictors of mortality after radical prostatectomy. J Urol. 2008; 179:1823–1829.22. Boorjian SA, Kim SP, Tollefson MK, Carrasco A, Cheville JC, Thompson RH, Thapa P, Frank I. Comparative performance of comorbidity indices for estimating perioperative and 5-year all cause mortality following radical cystectomy for bladder cancer. J Urol. 2013; 190:55–60.23. Mayr R, May M, Martini T, Lodde M, Comploj E, Pycha A, Strobel J, Denzinger S, Otto W, Wieland W, et al. Comorbidity and performance indices as predictors of cancer-independent mortality but not of cancer-specific mortality after radical cystectomy for urothelial carcinoma of the bladder. Eur Urol. 2012; 62:662–670.24. Mayr R, Fritsche HM, Pycha A, Pycha A. Radical cystectomy and the implications of comorbidity. Expert Rev Anticancer Ther. 2014; 14:289–295.25. Berod AA, Colin P, Yates DR, Ouzzane A, Audouin M, Adam E, Arroua F, Marchand C, Bigot P, Soulié M, et al. The role of American Society of Anesthesiologists scores in predicting urothelial carcinoma of the upper urinary tract outcome after radical nephroureterectomy: results from a national multi-institutional collaborative study. BJU Int. 2012; 110:E1035–40.26. Aziz A, Fritsche HM, Gakis G, Kluth LA. Comparative analysis of comorbidity and performance indices for prediction of oncological outcomes in patients with upper tract urothelial carcinoma who were treated with radical nephroureterectomy. Urol Oncol. 2014; 32:1141–1150.27. Lee KS, Kim KH, Yoon YE, Choi KH, Yang SC, Han WK. Impact of adjuvant chemotherapy in patients with upper tract urothelial carcinoma and lymphovascular invasion after radical nephroureterectomy. Korean J Urol. 2015; 56:41–47.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Impact of adjuvant chemotherapy in patients with upper tract urothelial carcinoma and lymphovascular invasion after radical nephroureterectomy
- Update on Current Role of Perioperative Chemotherapy in Upper Tract Urothelial Carcinoma
- Prognostic Value of Lymphovascular Invasion in Node-Negative Upper Urinary Tract Urothelial Carcinoma Patients Undergoing Radical Nephroureterectomy
- Risk Factors for Subsequent Bladder Tumor in Upper Tract Urothelial Tumor
- The Characteristics of Recurrent Upper Tract Urothelial Carcinoma after Radical Nephroureterectomy without Bladder Cuff Excision