J Korean Med Sci.
2017 Feb;32(2):195-203. 10.3346/jkms.2017.32.2.195.
Tandem High-Dose Chemotherapy and Autologous Stem Cell Transplantation for High-Grade Gliomas in Children and Adolescents
- Affiliations
-
- 1Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 2Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Department of Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 4Department of Neurosurgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. shinhj@skku.edu
- KMID: 2364162
- DOI: http://doi.org/10.3346/jkms.2017.32.2.195
Abstract
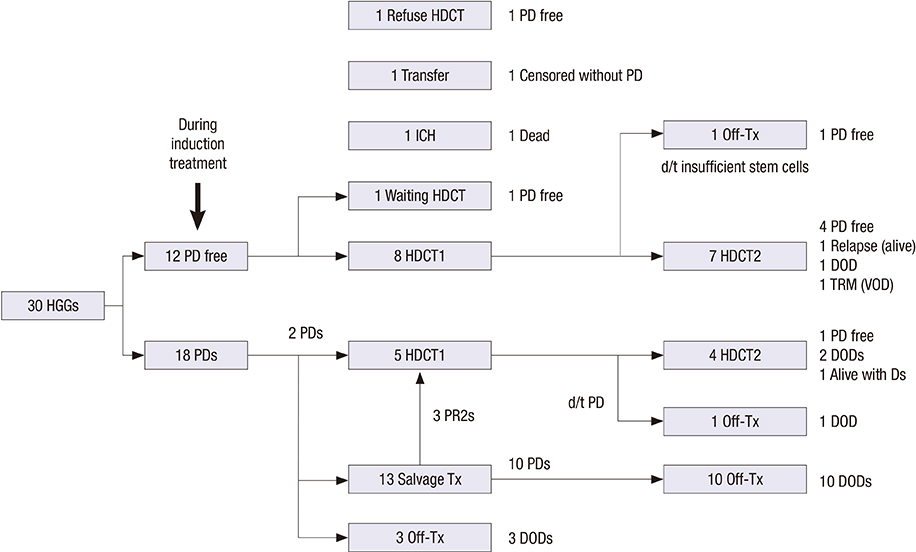
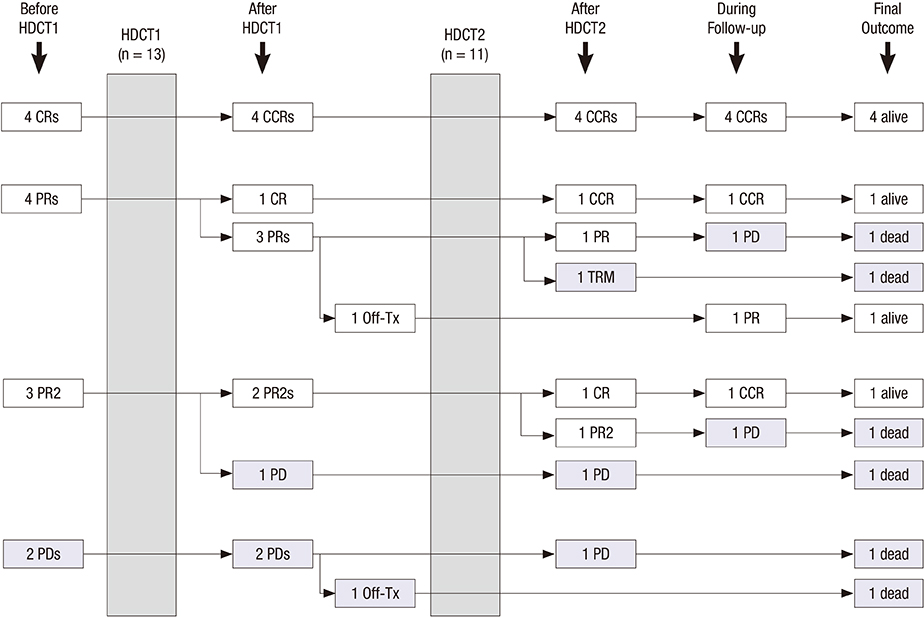
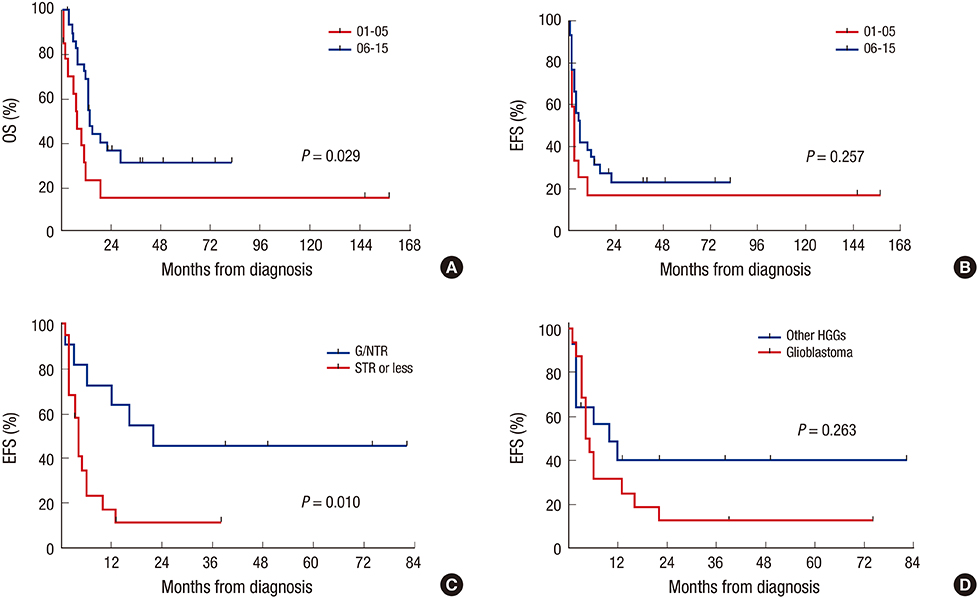
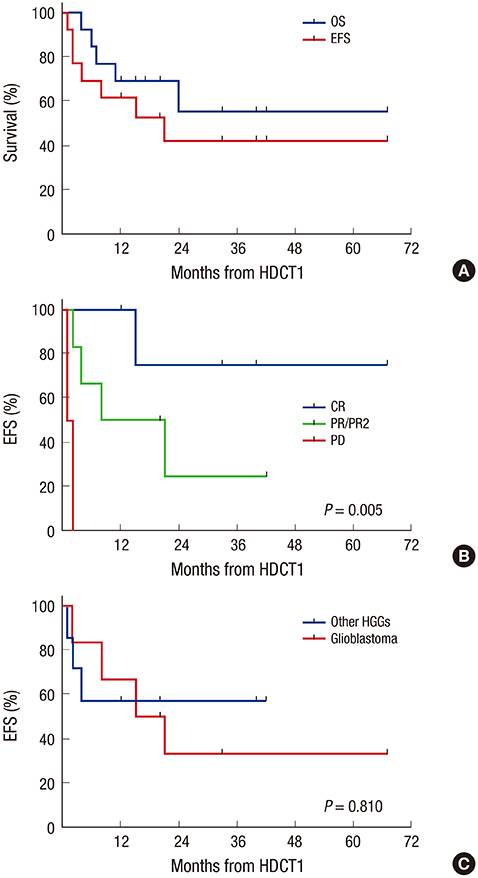
- With the aim to investigate the outcome of tandem high-dose chemotherapy and autologous stem cell transplantation (HDCT/auto-SCT) for high-grade gliomas (HGGs), we retrospectively reviewed the medical records of 30 patients with HGGs (16 glioblastomas, 7 anaplastic astrocytomas, and 7 other HGGs) between 2006 and 2015. Gross or near total resection was possible in 11 patients. Front-line treatment after surgery was radiotherapy (RT) in 14 patients and chemotherapy in the remaining 16 patients including 3 patients less than 3 years of age. Eight of 12 patients who remained progression free and 5 of the remaining 18 patients who experienced progression during induction treatment underwent the first HDCT/auto-SCT with carboplatin + thiotepa + etoposide (CTE) regimen and 11 of them proceeded to the second HDCT/auto-SCT with cyclophosphamide + melphalan (CyM) regimen. One patient died from hepatic veno-occlusive disease (VOD) during the second HDCT/auto-SCT; otherwise, toxicities were manageable. Four patients in complete response (CR) and 3 of 7 patients in partial response (PR) or second PR at the first HDCT/auto-SCT remained event free: however, 2 patients with progressive tumor experienced progression again. The probabilities of 3-year overall survival (OS) after the first HDCT/auto-SCT in 11 patients in CR, PR, or second PR was 58.2% ± 16.9%. Tumor status at the first HDCT/auto-SCT was the only significant factor for outcome after HDCT/auto-SCT. There was no difference in survival between glioblastoma and other HGGs. This study suggests that the outcome of HGGs in children and adolescents after HDCT/auto-SCT is encouraging if the patient could achieve CR or PR before HDCT/auto-SCT.
Keyword
MeSH Terms
-
Adolescent*
Astrocytoma
Brain Neoplasms
Carboplatin
Child*
Cyclophosphamide
Drug Therapy*
Etoposide
Glioblastoma
Glioma*
Hepatic Veno-Occlusive Disease
Humans
Medical Records
Melphalan
Radiotherapy
Retrospective Studies
Stem Cell Transplantation*
Stem Cells*
Thiotepa
Carboplatin
Cyclophosphamide
Etoposide
Melphalan
Thiotepa
Figure
Cited by 1 articles
-
Tandem High-dose Chemotherapy and Autologous Stem Cell Transplantation in Children with Brain Tumors : Review of Single Center Experience
Ki Woong Sung, Do Hoon Lim, Hyung Jin Shin
J Korean Neurosurg Soc. 2018;61(3):393-401. doi: 10.3340/jkns.2018.0039.
Reference
-
1. Bondy ML, Scheurer ME, Malmer B, Barnholtz-Sloan JS, Davis FG, Il’yasova D, Kruchko C, McCarthy BJ, Rajaraman P, Schwartzbaum JA, et al. Brain tumor epidemiology: consensus from the Brain Tumor Epidemiology Consortium. Cancer. 2008; 113:1953–1968.2. Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, Scheithauer BW, Kleihues P. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007; 114:97–109.3. Broniscer A, Gajjar A. Supratentorial high-grade astrocytoma and diffuse brainstem glioma: two challenges for the pediatric oncologist. Oncologist. 2004; 9:197–206.4. Cohen KJ, Pollack IF, Zhou T, Buxton A, Holmes EJ, Burger PC, Brat DJ, Rosenblum MK, Hamilton RL, Lavey RS, et al. Temozolomide in the treatment of high-grade gliomas in children: a report from the Children’s Oncology Group. Neuro-oncol. 2011; 13:317–323.5. Finlay JL, Zacharoulis S. The treatment of high grade gliomas and diffuse intrinsic pontine tumors of childhood and adolescence: a historical - and futuristic - perspective. J Neurooncol. 2005; 75:253–266.6. Finlay JL, Boyett JM, Yates AJ, Wisoff JH, Milstein JM, Geyer JR, Bertolone SJ, McGuire P, Cherlow JM, Tefft M, et al. Randomized phase III trial in childhood high-grade astrocytoma comparing vincristine, lomustine, and prednisone with the eight-drugs-in-1-day regimen. Childrens cancer group. J Clin Oncol. 1995; 13:112–123.7. Sposto R, Ertel IJ, Jenkin RD, Boesel CP, Venes JL, Ortega JA, Evans AE, Wara W, Hammond D. The effectiveness of chemotherapy for treatment of high grade astrocytoma in children: results of a randomized trial. A report from the Childrens Cancer Study Group. J Neurooncol. 1989; 7:165–177.8. Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005; 352:987–996.9. Lashford LS, Thiesse P, Jouvet A, Jaspan T, Couanet D, Griffiths PD, Doz F, Ironside J, Robson K, Hobson R, et al. Temozolomide in malignant gliomas of childhood: a United Kingdom Children’s Cancer Study Group and French Society for Pediatric Oncology Intergroup Study. J Clin Oncol. 2002; 20:4684–4691.10. Nicholson HS, Kretschmar CS, Krailo M, Bernstein M, Kadota R, Fort D, Friedman H, Harris MB, Tedeschi-Blok N, Mazewski C, et al. Phase 2 study of temozolomide in children and adolescents with recurrent central nervous system tumors: a report from the Children’s Oncology Group. Cancer. 2007; 110:1542–1550.11. Matthay KK, Reynolds CP, Seeger RC, Shimada H, Adkins ES, Haas-Kogan D, Gerbing RB, London WB, Villablanca JG. Long-term results for children with high-risk neuroblastoma treated on a randomized trial of myeloablative therapy followed by 13-cis-retinoic acid: a children’s oncology group study. J Clin Oncol. 2009; 27:1007–1013.12. Philip T, Ladenstein R, Lasset C, Hartmann O, Zucker JM, Pinkerton R, Pearson AD, Klingebiel T, Garaventa A, Kremens B, et al. 1070 myeloablative megatherapy procedures followed by stem cell rescue for neuroblastoma: 17 years of European experience and conclusions. European Group for Blood and Marrow Transplant Registry Solid Tumour Working Party. Eur J Cancer. 1997; 33:2130–2135.13. Fangusaro J, Finlay J, Sposto R, Ji L, Saly M, Zacharoulis S, Asgharzadeh S, Abromowitch M, Olshefski R, Halpern S, et al. Intensive chemotherapy followed by consolidative myeloablative chemotherapy with autologous hematopoietic cell rescue (AuHCR) in young children with newly diagnosed supratentorial primitive neuroectodermal tumors (sPNETs): report of the Head Start I and II experience. Pediatr Blood Cancer. 2008; 50:312–318.14. Mason WP, Grovas A, Halpern S, Dunkel IJ, Garvin J, Heller G, Rosenblum M, Gardner S, Lyden D, Sands S, et al. Intensive chemotherapy and bone marrow rescue for young children with newly diagnosed malignant brain tumors. J Clin Oncol. 1998; 16:210–221.15. Modak S, Gardner S, Dunkel IJ, Balmaceda C, Rosenblum MK, Miller DC, Halpern S, Finlay JL. Thiotepa-based high-dose chemotherapy with autologous stem-cell rescue in patients with recurrent or progressive CNS germ cell tumors. J Clin Oncol. 2004; 22:1934–1943.16. Gajjar A, Chintagumpala M, Ashley D, Kellie S, Kun LE, Merchant TE, Woo S, Wheeler G, Ahern V, Krasin MJ, et al. Risk-adapted craniospinal radiotherapy followed by high-dose chemotherapy and stem-cell rescue in children with newly diagnosed medulloblastoma (St Jude Medulloblastoma-96): long-term results from a prospective, multicentre trial. Lancet Oncol. 2006; 7:813–820.17. Sung KW, Lim DH, Lee SH, Yoo KH, Koo HH, Kim JH, Suh YL, Joung YS, Shin HJ. Tandem high-dose chemotherapy and auto-SCT for malignant brain tumors in children under 3 years of age. Bone Marrow Transplant. 2013; 48:932–938.18. Sung KW, Lim DH, Son MH, Lee SH, Yoo KH, Koo HH, Kim JH, Suh YL, Joung YS, Shin HJ. Reduced-dose craniospinal radiotherapy followed by tandem high-dose chemotherapy and autologous stem cell transplantation in patients with high-risk medulloblastoma. Neuro-oncol. 2013; 15:352–359.19. Sung KW, Lim DH, Yi ES, Choi YB, Lee JW, Yoo KH, Koo HH, Kim JH, Suh YL, Joung YS, et al. Tandem high-dose chemotherapy and autologous stem cell transplantation for atypical teratoid/rhabdoid tumor. Cancer Res Treat. 2016; 48:1408–1419.20. Finlay JL, Dhall G, Boyett JM, Dunkel IJ, Gardner SL, Goldman S, Yates AJ, Rosenblum MK, Stanley P, Zimmerman RA, et al. Myeloablative chemotherapy with autologous bone marrow rescue in children and adolescents with recurrent malignant astrocytoma: outcome compared with conventional chemotherapy: a report from the Children’s Oncology Group. Pediatr Blood Cancer. 2008; 51:806–811.21. Guruangan S, Dunkel IJ, Goldman S, Garvin JH, Rosenblum M, Boyett JM, Gardner S, Merchant TE, Gollamudi S, Finlay JL. Myeloablative chemotherapy with autologous bone marrow rescue in young children with recurrent malignant brain tumors. J Clin Oncol. 1998; 16:2486–2493.22. Grovas AC, Boyett JM, Lindsley K, Rosenblum M, Yates AJ, Finlay JL. Regimen-related toxicity of myeloablative chemotherapy with BCNU, thiotepa, and etoposide followed by autologous stem cell rescue for children with newly diagnosed glioblastoma multiforme: report from the Children’s Cancer Group. Med Pediatr Oncol. 1999; 33:83–87.23. Heideman RL, Douglass EC, Krance RA, Fontanesi J, Langston JA, Sanford RA, Kovnar EH, Ochs J, Kuttesch J, Jenkins JJ, et al. High-dose chemotherapy and autologous bone marrow rescue followed by interstitial and external-beam radiotherapy in newly diagnosed pediatric malignant gliomas. J Clin Oncol. 1993; 11:1458–1465.24. Massimino M, Gandola L, Luksch R, Spreafico F, Riva D, Solero C, Giangaspero F, Locatelli F, Podda M, Bozzi F, et al. Sequential chemotherapy, high-dose thiotepa, circulating progenitor cell rescue, and radiotherapy for childhood high-grade glioma. Neuro-oncol. 2005; 7:41–48.25. Lee SH, Son MH, Sung KW, Choi YB, Lee NH, Yoo KH, Koo HH, Lim DH, Shin HJ. Toxicity of tandem high-dose chemotherapy and autologous stem cell transplantation using carboplatin-thiotepa-etoposide and cyclophosphamide-melphalan regimens for malignant brain tumors in children and young adults. J Neurooncol. 2014; 120:507–513.26. Lee EQ, Puduvalli VK, Reid JM, Kuhn JG, Lamborn KR, Cloughesy TF, Chang SM, Drappatz J, Yung WK, Gilbert MR, et al. Phase I study of vorinostat in combination with temozolomide in patients with high-grade gliomas: North American Brain Tumor Consortium Study 04-03. Clin Cancer Res. 2012; 18:6032–6039.27. Narayana A, Golfinos JG, Fischer I, Raza S, Kelly P, Parker E, Knopp EA, Medabalmi P, Zagzag D, Eagan P, et al. Feasibility of using bevacizumab with radiation therapy and temozolomide in newly diagnosed high-grade glioma. Int J Radiat Oncol Biol Phys. 2008; 72:383–389.28. Reardon DA, Groves MD, Wen PY, Nabors L, Mikkelsen T, Rosenfeld S, Raizer J, Barriuso J, McLendon RE, Suttle AB, et al. A phase I/II trial of pazopanib in combination with lapatinib in adult patients with relapsed malignant glioma. Clin Cancer Res. 2013; 19:900–908.29. Gajjar A, Bowers DC, Karajannis MA, Leary S, Witt H, Gottardo NG. Pediatric brain tumors: innovative genomic information is transforming the diagnostic and clinical landscape. J Clin Oncol. 2015; 33:2986–2998.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Tandem High-dose Chemotherapy and Autologous Stem Cell Transplantation in Children with Brain Tumors : Review of Single Center Experience
- Hematologic Recovery after Tandem High-Dose Chemotherapy and Autologous Stem Cell Transplantation in Children with High-Risk Solid Tumors
- Evaluation of Cardiac Function in Children with Solid Tumors, who Underwent Tandem High-Dose Chemotherapy and Autologous Stem Cell Transplantation
- The Evolving Role of Myeloablative Chemotherapy with Stem Cell Transplantation for the Treatment of Autoimmune Disease
- Overview of CNS Gliomas in Childhood