Clin Orthop Surg.
2016 Mar;8(1):84-91. 10.4055/cios.2016.8.1.84.
Biomechanical Comparison of the Latarjet Procedure with and without Capsular Repair
- Affiliations
-
- 1Department of Orthopaedic Surgery, University of Southern California, Keck School of Medicine, Los Angeles, CA, USA.
- 2Orthopaedic Biomechanics Laboratory, VA Long Beach Healthcare System, Long Beach, CA, USA. tqlee@med.va.gov
- 3Department of Orthopaedic Surgery, University of California, Irvine, Irvine, CA, USA.
- KMID: 2363950
- DOI: http://doi.org/10.4055/cios.2016.8.1.84
Abstract
- BACKGROUND
The purpose of this study was to determine if capsular repair used in conjunction with the Latarjet procedure results in significant alterations in glenohumeral rotational range of motion and translation.
METHODS
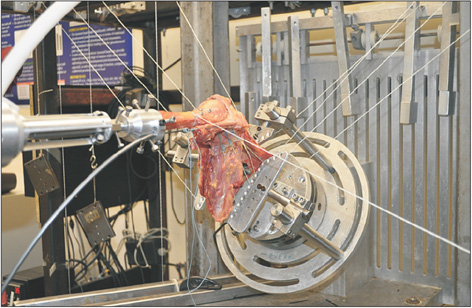
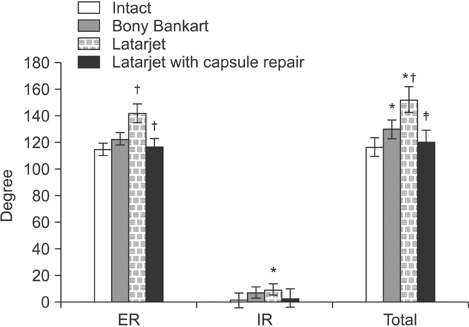
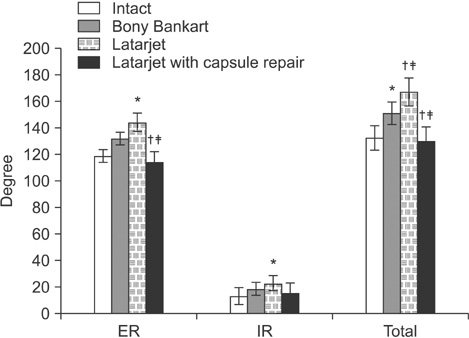
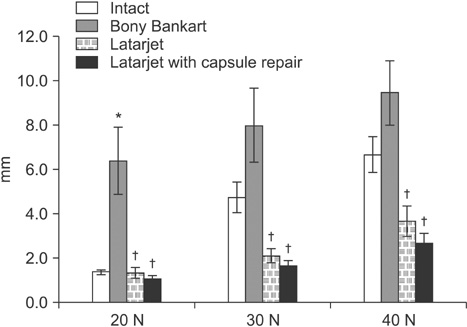
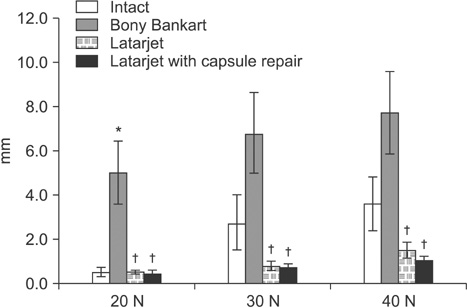
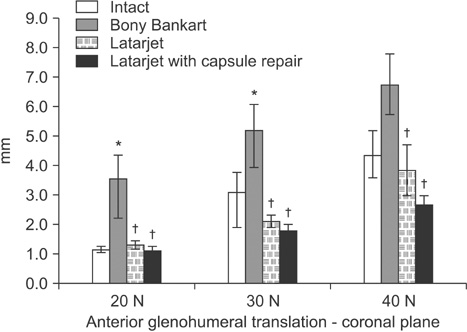
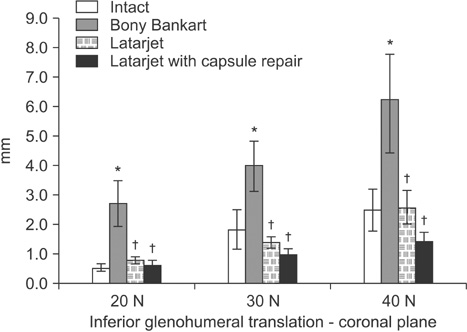
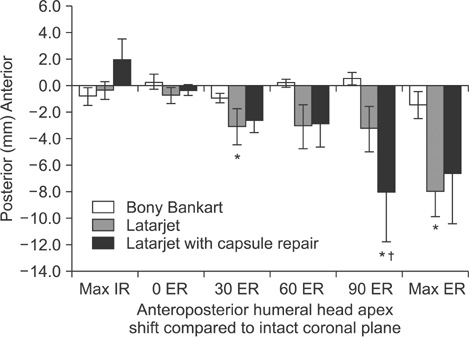
Glenohumeral rotational range of motion and translation were measured in eight cadaveric shoulders in 90degrees of abduction in both the scapular and coronal planes under the following four conditions: intact glenoid, 20% bony Bankart lesion, modified Latarjet without capsular repair, and modified Latarjet with capsular repair.
RESULTS
Creation of a 20% bony Bankart lesion led to significant increases in anterior and inferior glenohumeral translation and rotational range of motion (p < 0.005). The Latarjet procedure restored anterior and inferior stability compared to the bony Bankart condition. It also led to significant increases in glenohumeral internal and external rotational range of motion relative to both the intact and bony Bankart conditions (p < 0.05). The capsular repair from the coracoacromial ligament stump to the native capsule did not significantly affect translations relative to the Latarjet condition; however it did cause a significant decrease in external rotation in both the scapular and coronal planes (p < 0.005).
CONCLUSIONS
The Latarjet procedure is effective in restoring anteroinferior glenohumeral stability. The addition of a capsular repair does not result in significant added stability; however, it does appear to have the effect of restricting glenohumeral external rotational range of motion relative to the Latarjet procedure performed without capsular repair.
Keyword
MeSH Terms
Figure
Reference
-
1. Bankart AS, Cantab MC. Recurrent or habitual dislocation of the shoulder-joint: 1923. Clin Orthop Relat Res. 1993; (291):3–6.2. Speer KP, Deng X, Borrero S, Torzilli PA, Altchek DA, Warren RF. Biomechanical evaluation of a simulated Bankart lesion. J Bone Joint Surg Am. 1994; 76(12):1819–1826.
Article3. Kim SH, Ha KI, Cho YB, Ryu BD, Oh I. Arthroscopic anterior stabilization of the shoulder: two to six-year follow-up. J Bone Joint Surg Am. 2003; 85(8):1511–1518.4. Petrera M, Patella V, Patella S, Theodoropoulos J. A meta-analysis of open versus arthroscopic Bankart repair using suture anchors. Knee Surg Sports Traumatol Arthrosc. 2010; 18(12):1742–1747.
Article5. Tjoumakaris FP, Abboud JA, Hasan SA, Ramsey ML, Williams GR. Arthroscopic and open Bankart repairs provide similar outcomes. Clin Orthop Relat Res. 2006; 446:227–232.
Article6. Boileau P, Villalba M, Hery JY, Balg F, Ahrens P, Neyton L. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am. 2006; 88(8):1755–1763.
Article7. Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000; 16(7):677–694.
Article8. Porcellini G, Campi F, Pegreffi F, Castagna A, Paladini P. Predisposing factors for recurrent shoulder dislocation after arthroscopic treatment. J Bone Joint Surg Am. 2009; 91(11):2537–2542.
Article9. Tauber M, Resch H, Forstner R, Raffl M, Schauer J. Reasons for failure after surgical repair of anterior shoulder instability. J Shoulder Elbow Surg. 2004; 13(3):279–285.
Article10. Latarjet M. Treatment of recurrent dislocation of the shoulder. Lyon Chir. 1954; 49(8):994–997.11. Giles JW, Boons HW, Elkinson I, et al. Does the dynamic sling effect of the Latarjet procedure improve shoulder stability? A biomechanical evaluation. J Shoulder Elbow Surg. 2013; 22(6):821–827.
Article12. Wellmann M, de Ferrari H, Smith T, et al. Biomechanical investigation of the stabilization principle of the Latarjet procedure. Arch Orthop Trauma Surg. 2012; 132(3):377–386.
Article13. Yamamoto N, Muraki T, An KN, et al. The stabilizing mechanism of the Latarjet procedure: a cadaveric study. J Bone Joint Surg Am. 2013; 95(15):1390–1397.14. Hovelius L, Sandstrom B, Olofsson A, Svensson O, Rahme H. The effect of capsular repair, bone block healing, and position on the results of the Bristow-Latarjet procedure (study III): long-term follow-up in 319 shoulders. J Shoulder Elbow Surg. 2012; 21(5):647–660.
Article15. Barry TP, Lombardo SJ, Kerlan RK, et al. The coracoid transfer for recurrent anterior instability of the shoulder in adolescents. J Bone Joint Surg Am. 1985; 67(3):383–387.
Article16. Schroder DT, Provencher MT, Mologne TS, Muldoon MP, Cox JS. The modified Bristow procedure for anterior shoulder instability: 26-year outcomes in Naval Academy midshipmen. Am J Sports Med. 2006; 34(5):778–786.
Article17. Kephart CJ, Abdulian MH, McGarry MH, Tibone JE, Lee TQ. Biomechanical analysis of the modified Bristow procedure for anterior shoulder instability: is the bone block necessary? J Shoulder Elbow Surg. 2014; 23(12):1792–1799.
Article18. Itoi E, Morrey BF, An KN. Biomechanics of the shoulder. In : Rockwood CA, Matsen FA, editors. The shoulder. 4th ed. Philadelphia: Saunders;2009. p. 223–268.19. Lee TQ, Black AD, Tibone JE, McMahon PJ. Release of the coracoacromial ligament can lead to glenohumeral laxity: a biomechanical study. J Shoulder Elbow Surg. 2001; 10(1):68–72.
Article20. Tibone JE, McMahon PJ, Shrader TA, Sandusky MD, Lee TQ. Glenohumeral joint translation after arthroscopic, nonablative, thermal capsuloplasty with a laser. Am J Sports Med. 1998; 26(4):495–498.
Article21. Walch G, Boileau P. Latarjet-Bristow procedure for recurrent anterior instability. Tech Shoulder Elbow Surg. 2000; 1(4):256–261.
Article22. Young AA, Maia R, Berhouet J, Walch G. Open Latarjet procedure for management of bone loss in anterior instability of the glenohumeral joint. J Shoulder Elbow Surg. 2011; 20:2 Suppl. S61–S69.
Article23. Lee YS, Lee TQ. Specimen-specific method for quantifying glenohumeral joint kinematics. Ann Biomed Eng. 2010; 38(10):3226–3236.
Article24. Hovelius L, Vikerfors O, Olofsson A, Svensson O, Rahme H. Bristow-Latarjet and Bankart: a comparative study of shoulder stabilization in 185 shoulders during a seventeen-year follow-up. J Shoulder Elbow Surg. 2011; 20(7):1095–1101.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Arthroscopic Latarjet procedure: current concepts and surgical techniques
- Osseous Defects Seen in Patients with Anterior Shoulder Instability
- Concomitant Coracoid Process Fracture with Bony Bankart Lesion Treated with the Latarjet Procedure
- Superior capsular reconstruction for irreparable rotator cuff tear: a review of current methods
- Risk factors for unexpected readmission and reoperation following open procedures for shoulder instability: a national database study of 1,942 cases