Korean J Ophthalmol.
2015 Apr;29(2):115-120. 10.3341/kjo.2015.29.2.115.
Clinical Outcomes of Individualized Botulinum Neurotoxin Type A Injection Techniques in Patients with Essential Blepharospasm
- Affiliations
-
- 1Department of Ophthalmology, CHA Bundang Medical Center, CHA University, Seongnam, Korea. eye@cha.ac.kr
- KMID: 2363717
- DOI: http://doi.org/10.3341/kjo.2015.29.2.115
Abstract
- PURPOSE
To assess the clinical outcomes following botulinum neurotoxin type A (BoNT-A) treatment with an individualized injection technique based on the types of spasms and to compare the results of the individualized injection technique with those of the conventional injection technique in the same patients.
METHODS
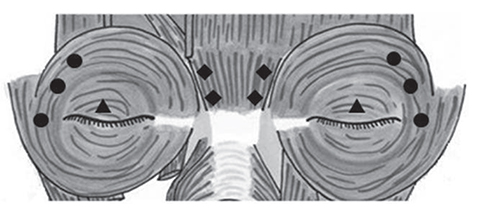
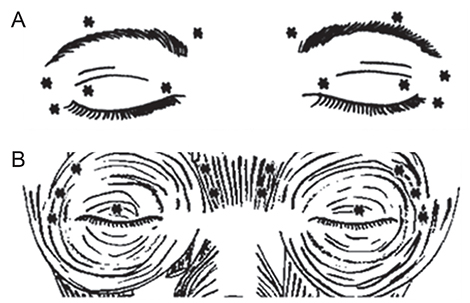
From November 2011 to July 2013, 77 BoNT-A injections were performed in 38 patients. Eighteen patients were treated with conventional BoNT-A injections before 2011, and 20 patients were referred to our hospital for unsatisfactory results after a conventional injection technique. We classified the patients by spasm-dominant sites: the lateral orbital area, representing the orbital orbicularis-dominant group (ODG); the glabella, representing the corrugator-dominant group (CDG); and the ptosis, representing the palpebral part of the orbicularis-dominant group (PDG). We increased the injection dose into the spasm-dominant sites of the blepharospasm groups. We assessed subjective symptom scores (functional disability score, FDS) after treatment.
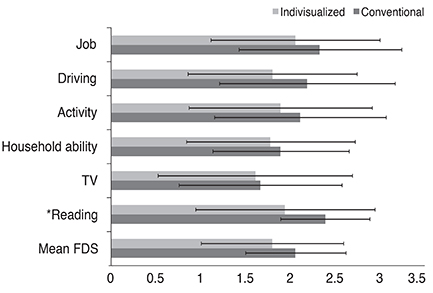
RESULTS
This study included 38 patients (26 women, 12 men; mean age, 60.6 +/- 10.9 years). There were 21 patients in the ODG, 10 patients in the CDG, and 7 patients in the PDG. Mean ages were 59.7 +/- 12.6, 59.8 +/- 8.5, and 66.8 +/- 9.0 years, and mean BoNT-A injection dose was 38.8 +/- 11.2, 38.8 +/- 11.2, and 38.8 +/- 10.8 U in each group, respectively (p = 0.44, 0.82 Kruskal-Wallis test). Mean FDS after injection was 1.7 +/- 0.7 in the ODG, 1.4 +/- 0.8 in the CDG, and 1.2 +/- 0.3 in the PDG. There were significant differences in reading and job scale among the three groups. In a comparison between the conventional and individualized injection techniques, there was a significant improvement in mean FDS and in the reading scale in the PDG with the individualized injection technique. The success rate was 92.1% in the conventional injection group and 94.1% in the individualized injection group.
CONCLUSIONS
The individualized injection technique of BoNT-A according to the spasm-dominant site is an effective and safe treatment method for essential blepharospasm patients.
MeSH Terms
-
Aged
Blepharospasm/*drug therapy/physiopathology
Botulinum Toxins, Type A/*administration & dosage
Dose-Response Relationship, Drug
Eye Movements/*drug effects
Female
Follow-Up Studies
Humans
Injections
Male
Middle Aged
Neuromuscular Agents/administration & dosage
Oculomotor Muscles/*physiopathology
Retrospective Studies
Treatment Outcome
Botulinum Toxins, Type A
Neuromuscular Agents
Figure
Cited by 1 articles
-
Long-term Efficacy of Botulinum Neurotoxin-A Treatment for Essential Blepharospasm
Seunghyun Lee, Sangrye Park, Helen Lew
Korean J Ophthalmol. 2018;32(1):1-7. doi: 10.3341/kjo.2017.0030.
Reference
-
1. Henderson JW. Essential blepharospasm. Trans Am Ophthalmol Soc. 1956; 54:453–520.2. Kim YD, Levine MR. Treatment of blepharospasm with botulinum A toxin. Korean J Ophthalmol. 1987; 1:102–108.3. Jankovic J. Clinical features, differential diagnosis and pathogenesis of blepharospasm and cranial-cervical dystonia. Adv Ophthalmic Plast Reconstr Surg. 1985; 4:67–82.4. Dortzbach RK. Complications in surgery for blepharospasm. Am J Ophthalmol. 1973; 75:142–147.5. Frueh BR, Callahan A, Dortzbach RK, et al. The effects of differential section of the VIITH nerve on patients with intractable blepharospasm. Trans Sect Ophthalmol Am Acad Ophthalmol Otolaryngol. 1976; 81(4 Pt 1):OP595–OP602.6. Reynolds DH, Smith JL, Walsh TJ. Differential section of the facial nerve for blepharospasm. Trans Am Acad Ophthalmol Otolaryngol. 1967; 71:656–664.7. Battista AF. Surgical therapy for blepharospasm. Adv Neurol. 1983; 37:215–224.8. Putterman AM, Urist M. Treatment of essential blepharospasm with a frontalis sling. Arch Ophthalmol. 1972; 88:278–281.9. Callahan A. Blepharospasm with resection of part of orbicularis nerve supply: correction of intractable cases. Arch Ophthalmol. 1963; 70:508–511.10. Fox SA. Relief of intractable blepharospasm: a preliminary report. Am J Ophthalmol. 1951; 34:1351–1356.11. Fox SA. Essential (idiopathic) blepharospasm. Arch Ophthalmol. 1966; 76:318–321.12. Gillum WN, Anderson RL. Blepharospasm surgery: an anatomical approach. Arch Ophthalmol. 1981; 99:1056–1062.13. Albanese A, Asmus F, Bhatia KP, et al. EFNS guidelines on diagnosis and treatment of primary dystonias. Eur J Neurol. 2011; 18:5–18.14. Colosimo C, Suppa A, Fabbrini G, et al. Craniocervical dystonia: clinical and pathophysiological features. Eur J Neurol. 2010; 17:Suppl 1. 15–21.15. Simpson DM, Blitzer A, Brashear A, et al. Assessment: botulinum neurotoxin for the treatment of movement disorders (an evidence-based review). Report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2008; 70:1699–1706.16. Czyz CN, Burns JA, Petrie TP, et al. Long-term botulinum toxin treatment of benign essential blepharospasm, hemifacial spasm, and Meige syndrome. Am J Ophthalmol. 2013; 156:173–177.e2.17. Grivet D, Robert PY, Thuret G, et al. Assessment of blepharospasm surgery using an improved disability scale: study of 138 patients. Ophthal Plast Reconstr Surg. 2005; 21:230–234.18. Bodker FS, Olson JJ, Putterman AM. Acquired blepharoptosis secondary to essential blepharospasm. Ophthalmic Surg. 1993; 24:546–550.19. Ababneh OH, Cetinkaya A, Kulwin DR. Long-term efficacy and safety of botulinum toxin A injections to treat blepharospasm and hemifacial spasm. Clin Experiment Ophthalmol. 2014; 42:254–261.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Long-term Efficacy of Botulinum Neurotoxin-A Treatment for Essential Blepharospasm
- Management of Essential Blepharospasm: Botulinum Toxin A Treatment and Orbicularis Myectomy Operation
- Clinical Comparability of Dysport and Botox in Essential Blepharospasm
- Influence of Botulinum Toxin A on Corneal Astigmatism
- Treatment of blepharospasm with botulinum A toxin