The establishment of KORCC (KOrean Renal Cell Carcinoma) database
- Affiliations
-
- 1Department of Urology, Seoul National University Bundang Hospital, Seongnam, Korea. ssbyun@snubh.org
- 2Department of Urology, Seoul National University of Hospital, Seoul, Korea.
- 3Department of Urology, Seoul St. Mary's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea.
- 4Department of Urology, Chungbuk National University College of Medicine, Cheongju, Korea.
- 5Department of Urology, Chonnam National University Hwasun Hospital, Hwasun, Korea.
- 6Department of Urology, Kyungpook National University Medical Center, Kyungpook National University School of Medicine, Daegu, Korea.
- 7Department of Urology, Korea University Medical Center, Seoul, Korea.
- 8Department of Urology, National Cancer Center, Goyang, Korea.
- KMID: 2363124
- DOI: http://doi.org/10.4111/icu.2016.57.1.50
Abstract
- PURPOSE
The purpose of this article is to report establishment of the 1st Web-based database (DB) system to collect renal cell carcinoma (RCC) data in Korea.
MATERIALS AND METHODS
The new Web-based DB system was established to collect basic demographic and clinicopahtological characteristics of a large cohort of patients with RCC in Korea. Data from a total of 6,849 patients were collected from 8 tertiary care hospitals that agreed to participate in organizing the Korean Renal Cell Carcinoma (KORCC) study group as of 1 July 2015. Basic demographic and clinicopathological characteristics were collected. The data of patients who underwent surgical treatments were analyzed to characterize Korean RCC.
RESULTS
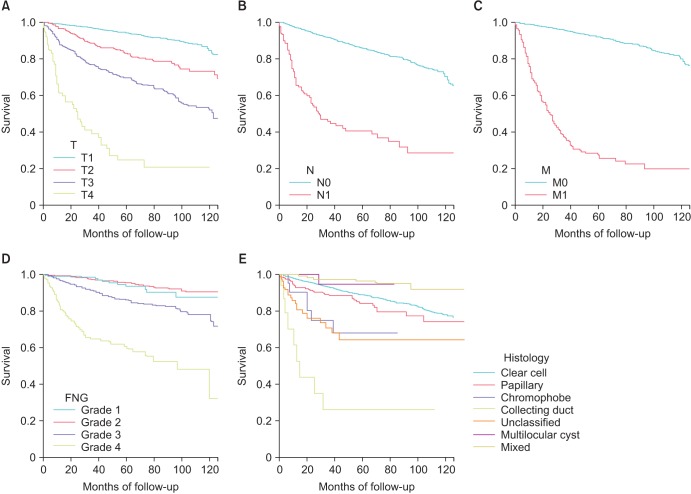
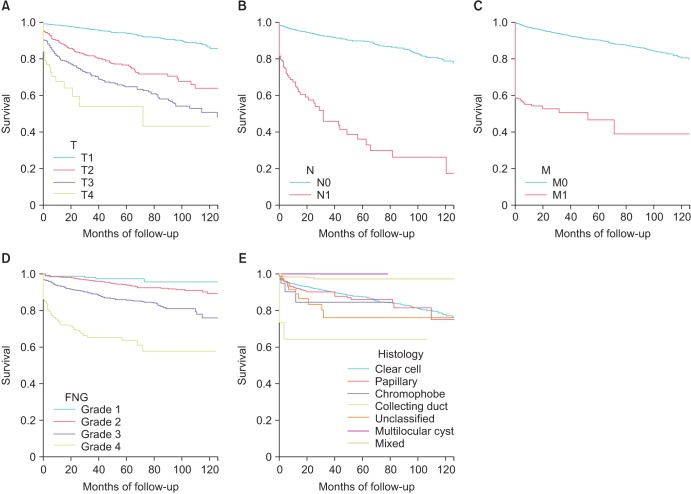
We established the 1st Web-based DB of Korean RCC, a database comprising renal mass management cases from multiple centers in Korea. The data of 5,281 patients who underwent surgical management (mean follow-up, 32 months) were analyzed. The most common symptom was incidentally detected renal mass (76.9%). Clinical T1a was the most common (54.3%) stage and mean tumor size was 4.8+/-4.2 cm. Radical nephrectomy accounted for 62.7% of cases and an open approach was used in 50.7% and 52.2% of radical and partial nephrectomies, respectively. The 5-year overall, cancer-specific and recurrence-free survival rates were 88.1%, 92.2%, and 88.0%, respectively.
CONCLUSIONS
We report the 1st establishment of a Web-based DB system to collect RCC data in Korea. This DB system will provide a solid basis for the characterization of Korean RCC.
MeSH Terms
Figure
Cited by 2 articles
-
Partial versus Radical Nephrectomy for T1-T2 Renal Cell Carcinoma in Patients with Chronic Kidney Disease Stage III: a Multiinstitutional Analysis of Kidney Function and Survival Rate
Jae-Seung Chung, Nak Hoon Son, Sang Eun Lee, Sung Kyu Hong, Chang Wook Jeong, Cheol Kwak, Hyeon Hoe Kim, Sung Hoo Hong, Yong June Kim, Seok Ho Kang, Jinsoo Chung, Tae Gyun Kwon, Eu Chang Hwang, Seok-Soo Byun
J Korean Med Sci. 2018;33(43):. doi: 10.3346/jkms.2018.33.e277.Trends in clinical, operative, and pathologic characteristics of surgically treated renal mass in a Korean center: A surgical series from 1988 through 2015
Ho Won Kang, Sung Pil Seo, Won Tae Kim, Seok Joong Yun, Sang-Cheol Lee, Wun-Jae Kim, Eu Chang Hwang, Seok Ho Kang, Sung-Hoo Hong, Jinsoo Chung, Tae Gyun Kwon, Hyeon Hoe Kim, Cheol Kwak, Seok-Soo Byun, Yong-June Kim,
Investig Clin Urol. 2019;60(3):184-194. doi: 10.4111/icu.2019.60.3.184.
Reference
-
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015; 65:5–29. PMID: 25559415.
Article2. Jung KW, Won YJ, Kong HJ, Oh CM, Cho H, Lee DH, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2012. Cancer Res Treat. 2015; 47:127–141. PMID: 25761484.
Article3. Clinical Research Office of the Endourological Society [Internet]. [New York]: Clinical Research Office of the Endourological Society;c2011. cited 2015 Oct 13. Available from: http://www.croesoffice.org/.4. Hew MN, Zondervan PJ, Guven S, de la Rosette J, Laguna MP. Prognostic models and factors for patients with renal-cell carcinoma: a survey on their use among urologists. J Endourol. 2013; 27:790–799. PMID: 23379666.
Article5. Brookman-May S, May M, Zigeuner R, Shariat SF, Scherr DS, Chromecki T, et al. Collecting system invasion and Fuhrman grade but not tumor size facilitate prognostic stratification of patients with pT2 renal cell carcinoma. J Urol. 2011; 186:2175–2181. PMID: 22014800.6. Aziz A, May M, Zigeuner R, Pichler M, Chromecki T, Cindolo L, et al. Do young patients with renal cell carcinoma feature a distinct outcome after surgery? A comparative analysis of patient age based on the multinational CORONA database. J Urol. 2014; 191:310–315. PMID: 23973516.
Article7. Brookman-May SD, May M, Wolff I, Zigeuner R, Hutterer GC, Cindolo L, et al. Evaluation of the prognostic significance of perirenal fat invasion and tumor size in patients with pT1-pT3a localized renal cell carcinoma in a comprehensive multicenter study of the CORONA project. Can we improve prognostic discrimination for patients with stage pT3a tumors? Eur Urol. 2015; 67:943–951. PMID: 25684695.8. Brookman-May SD, May M, Shariat SF, Novara G, Zigeuner R, Cindolo L, et al. Time to recurrence is a significant predictor of cancer-specific survival after recurrence in patients with recurrent renal cell carcinoma--results from a comprehensive multicentre database (CORONA/SATURN-Project). BJU Int. 2013; 112:909–916. PMID: 23890378.9. Brookman-May S, May M, Shariat SF, Xylinas E, Stief C, Zigeuner R, et al. Features associated with recurrence beyond 5 years after nephrectomy and nephron-sparing surgery for renal cell carcinoma: development and internal validation of a risk model (PRELANE score) to predict late recurrence based on a large multicenter database (CORONA/SATURN Project). Eur Urol. 2013; 64:472–477. PMID: 22748912.10. Hirono M, Kobayashi M, Tsushima T, Obara W, Shinohara N, Ito K, et al. Impacts of clinicopathologic and operative factors on short-term and long-term survival in renal cell carcinoma with venous tumor thrombus extension: a multi-institutional retrospective study in Japan. BMC Cancer. 2013; 13:447. PMID: 24083566.
Article11. Shinohara N, Obara W, Tatsugami K, Naito S, Kamba T, Takahashi M, et al. Prognosis of Japanese patients with previously untreated metastatic renal cell carcinoma in the era of molecular-targeted therapy. Cancer Sci. 2015; 106:618–626. PMID: 25711777.12. Park H, Byun SS, Kim HH, Lee SB, Kwon TG, Jeon SH, et al. Comparison of laparoscopic and open partial nephrectomies in t1a renal cell carcinoma: a Korean multicenter experience. Korean J Urol. 2010; 51:467–471. PMID: 20664779.
Article13. Jeon SH, Kwon TG, Rha KH, Sung GT, Lee W, Lim JS, et al. Comparison of laparoscopic versus open radical nephrectomy for large renal tumors: a retrospective analysis of multi-center results. BJU Int. 2011; 107:817–821. PMID: 21029315.
Article14. Chung JS, Son NH, Lee SE, Hong SK, Lee SC, Kwak C, et al. Overall survival and renal function after partial and radical nephrectomy among older patients with localised renal cell carcinoma: a propensity-matched multicentre study. Eur J Cancer. 2015; 51:489–497. PMID: 25576517.
Article15. Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, editors. AJCC cancer staging manual. 7th ed. New York: Springer;2010.16. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213. PMID: 15273542.17. Park YH, Lee ES, Kim HH, Kwak C, Ku JH, Lee SE, et al. Longterm oncologic outcomes of hand-assisted laparoscopic radical nephrectomy for clinically localized renal cell carcinoma: a multi-institutional comparative study. J Laparoendosc Adv Surg Tech A. 2014; 24:556–562. PMID: 25007232.
Article18. Oh JJ, Byun SS, Lee SE, Hong SK, Lee ES, Kim HH, et al. Partial nephrectomy versus radical nephrectomy for nonmetastatic pathological T3a renal cell carcinoma: a multiinstitutional comparative analysis. Int J Urol. 2014; 21:352–357. PMID: 24118633.
Article19. Pantuck AJ, Zisman A, Rauch MK, Belldegrun A. Incidental renal tumors. Urology. 2000; 56:190–196. PMID: 10925076.
Article20. Masson-Lecomte A, Yates DR, Hupertan V, Haertig A, Chartier-Kastler E, Bitker MO, et al. A prospective comparison of the pathologic and surgical outcomes obtained after elective treatment of renal cell carcinoma by open or robot-assisted partial nephrectomy. Urol Oncol. 2013; 31:924–929. PMID: 21906969.
Article21. Ficarra V, Minervini A, Antonelli A, Bhayani S, Guazzoni G, Longo N, et al. A multicentre matched-pair analysis comparing robot-assisted versus open partial nephrectomy. BJU Int. 2014; 113:936–941. PMID: 24219227.
Article22. Storkel S, Eble JN, Adlakha K, Amin M, Blute ML, Bostwick DG, et al. Classification of renal cell carcinoma: Workgroup No. 1. Union Internationale Contre le Cancer (UICC) and the American Joint Committee on Cancer (AJCC). Cancer. 1997; 80:987–989. PMID: 9307203.23. Rini BI, Campbell SC, Escudier B. Renal cell carcinoma. Lancet. 2009; 373:1119–1132. PMID: 19269025.
Article24. Delahunt B. Sarcomatoid renal carcinoma: the final common dedifferentiation pathway of renal epithelial malignancies. Pathology. 1999; 31:185–190. PMID: 10503259.
Article25. Cheville JC, Lohse CM, Zincke H, Weaver AL, Leibovich BC, Frank I, et al. Sarcomatoid renal cell carcinoma: an examination of underlying histologic subtype and an analysis of associations with patient outcome. Am J Surg Pathol. 2004; 28:435–441. PMID: 15087662.