Ann Hepatobiliary Pancreat Surg.
2016 Nov;20(4):173-179. 10.14701/ahbps.2016.20.4.173.
Incidence of underlying biliary neoplasm in patients after major hepatectomy for preoperative benign hepatolithiasis
- Affiliations
-
- 1Department of Surgery, Chonnam National University College of Medicine, Hwasun, Korea. surgihur@naver.com
- KMID: 2362467
- DOI: http://doi.org/10.14701/ahbps.2016.20.4.173
Abstract
- BACKGROUNDS/AIMS
Despite hepatolithiasis being a risk factor for biliary neoplasm including cholangiocarcinoma, the incidence of underlying biliary neoplasm is unknown in patients with preoperative benign hepatolithiasis. The aim of this study was to evaluate the incidence of underlying biliary neoplasm in patients who underwent major hepatectomy for preoperative benign hepatolithiasis.
METHODS
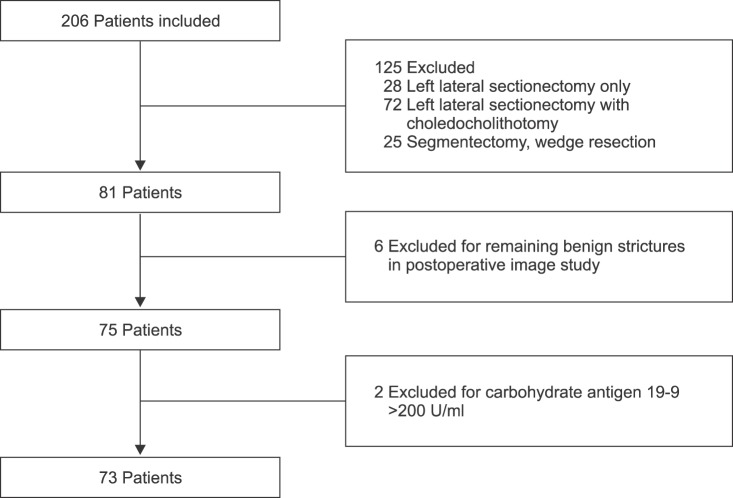
Between March 2005 and December 2015, 73 patients who underwent major hepatectomy for preoperative benign hepatolithiasis were enrolled in this study. The incidence and pathological differentiation of concomitant biliary neoplasm were retrospectively determined by review of medical records. Postoperative complications after major hepatectomy were evaluated.
RESULTS
Concomitant biliary neoplasm was pathologically confirmed in 20 patients (27.4%). Biliary intraepithelial neoplasia (BIN) was detected in 12 patients (16.4%), and 1 patient (1.4%) had intraductal papillary mucinous neoplasm (IPMN), as the premalignant lesion. Cholangiocarcinoma was pathologically confirmed in 7 patients (9.6%). Preoperative imaging of the 73 patients revealed biliary stricture at the first branch of bile duct in 31 patients (42.5%), and at the second branch of bile duct in 39 patients (53.4%). Postoperative complications developed in 14 patients (19.1%). Almost all patients recovered from complications, including intra-abdominal abscess (9.6%), bile leakage (4.1%), pleural effusion (2.7%), and wound infection (1.4%). Only 1 patient (1.4%) died from aspiration pneumonia.
CONCLUSIONS
The incidence of underlying biliary neoplasm was not negligible in the patients with hepatolithiasis, despite meticulous preoperative evaluations.
MeSH Terms
Figure
Reference
-
1. Lee TY, Chen YL, Chang HC, Chan CP, Kuo SJ. Outcomes of hepatectomy for hepatolithiasis. World J Surg. 2007; 31:479–482. PMID: 17334864.
Article2. Chen DW, Tung-Ping Poon R, Liu CL, Fan ST, Wong J. Immediate and long-term outcomes of hepatectomy for hepatolithiasis. Surgery. 2004; 135:386–393. PMID: 15041962.
Article3. Blechacz B, Komuta M, Roskams T, Gores GJ. Clinical diagnosis and staging of cholangiocarcinoma. Nat Rev Gastroenterol Hepatol. 2011; 8:512–522. PMID: 21808282.
Article4. Tyson GL, El-Serag HB. Risk factors for cholangiocarcinoma. Hepatology. 2011; 54:173–184. PMID: 21488076.
Article5. Lee SK, Seo DW, Myung SJ, Park ET, Lim BC, Kim HJ, et al. Percutaneous transhepatic cholangioscopic treatment for hepatolithiasis: an evaluation of long-term results and risk factors for recurrence. Gastrointest Endosc. 2001; 53:318–323. PMID: 11231390.
Article6. Jeng KS, Sheen IS, Yang FS. Percutaneous transhepatic cholangioscopy in the treatment of complicated intrahepatic biliary strictures and hepatolithiasis with internal metallic stent. Surg Laparosc Endosc Percutan Tech. 2000; 10:278–283. PMID: 11083209.
Article7. Yeh YH, Huang MH, Yang JC, Mo LR, Lin J, Yueh SK. Percutaneous trans-hepatic cholangioscopy and lithotripsy in the treatment of intrahepatic stones: a study with 5 year follow-up. Gastrointest Endosc. 1995; 42:13–18. PMID: 7557170.
Article8. Kim HJ, Kim JS, Suh SJ, Lee BJ, Park JJ, Lee HS, et al. Cholangiocarcinoma risk as long-term outcome after hepatic resection in the hepatolithiasis patients. World J Surg. 2015; 39:1537–1542. PMID: 25648078.
Article9. Van Beers BE. Diagnosis of cholangiocarcinoma. HPB (Oxford). 2008; 10:87–93. PMID: 18773062.
Article10. Juntermanns B, Radunz S, Heuer M, Hertel S, Reis H, Neuhaus JP, et al. Tumor markers as a diagnostic key for hilar cholangiocarcinoma. Eur J Med Res. 2010; 15:357–361. PMID: 20947473.
Article11. Fan ST. Hepatocellular carcinoma--resection or transplant? Nat Rev Gastroenterol Hepatol. 2012; 9:732–737. PMID: 22965432.
Article12. Zhou Q, Gong Y, Huang F, Lin Q, Zeng B, Li Z, et al. Expression levels and significance of nuclear factor-κB and epidermal growth factor receptor in hepatolithiasis associated with intrahepatic cholangiocarcinoma. Dig Surg. 2013; 30:309–316. PMID: 24008372.
Article13. Lee KT, Chang WT, Wang SN, Chuang SC, Chai CY, Hu SW. Expression of DPC4/Smad4 gene in stone-containing intrahepatic bile duct. J Surg Oncol. 2006; 94:338–343. PMID: 16917866.
Article14. Kuroki T, Tajima Y, Kanematsu T. Hepatolithiasis and intrahepatic cholangiocarcinoma: carcinogenesis based on molecular mechanisms. J Hepatobiliary Pancreat Surg. 2005; 12:463–466. PMID: 16365819.
Article15. Uenishi T, Hamba H, Takemura S, Oba K, Ogawa M, Yamamoto T, et al. Outcomes of hepatic resection for hepatolithiasis. Am J Surg. 2009; 198:199–202. PMID: 19249730.
Article16. Cheon YK, Cho YD, Moon JH, Lee JS, Shim CS. Evaluation of long-term results and recurrent factors after operative and nonoperative treatment for hepatolithiasis. Surgery. 2009; 146:843–853. PMID: 19744434.
Article17. Lin CC, Lin PY, Chen YL. Comparison of concomitant and subsequent cholangiocarcinomas associated with hepatolithiasis: clinical implications. World J Gastroenterol. 2013; 19:375–380. PMID: 23372360.
Article18. Suzuki Y, Mori T, Abe N, Sugiyama M, Atomi Y. Predictive factors for cholangiocarcinoma associated with hepatolithiasis determined on the basis of Japanese Multicenter study. Hepatol Res. 2012; 42:166–170. PMID: 22151748.
Article19. Suzuki Y, Mori T, Yokoyama M, Nakazato T, Abe N, Nakanuma Y, et al. Hepatolithiasis: analysis of Japanese nationwide surveys over a period of 40 years. J Hepatobiliary Pancreat Sci. 2014; 21:617–622. PMID: 24824191.
Article20. Catena M, Aldrighetti L, Finazzi R, Arzu G, Arru M, Pulitanò C, et al. Treatment of non-endemic hepatolithiasis in a Western country. The role of hepatic resection. Ann R Coll Surg Engl. 2006; 88:383–389. PMID: 16834860.
Article21. Khan SA, Davidson BR, Goldin R, Pereira SP, Rosenberg WM, Taylor-Robinson SD, et al. Guidelines for the diagnosis and treatment of cholangiocarcinoma: consensus document. Gut. 2002; 51(Suppl 6):VI1–VI9. PMID: 12376491.
Article22. Dodson RM, Weiss MJ, Cosgrove D, Herman JM, Kamel I, Anders R, et al. Intrahepatic cholangiocarcinoma: management options and emerging therapies. J Am Coll Surg. 2013; 217:736–750.e4. PMID: 23890842.
Article23. Jan YY, Chen MF, Wang CS, Jeng LB, Hwang TL, Chen SC. Surgical treatment of hepatolithiasis: long-term results. Surgery. 1996; 120:509–514. PMID: 8784405.
Article24. Sato M, Watanabe Y, Horiuchi S, Nakata Y, Sato N, Kashu Y, et al. Long-term results of hepatic resection for hepatolithiasis. HPB Surg. 1995; 9:37–41. PMID: 8857452.
Article25. Otani K, Shimizu S, Chijiiwa K, Ogawa T, Morisaki T, Sugitani A, et al. Comparison of treatments for hepatolithiasis: hepatic resection versus cholangioscopic lithotomy. J Am Coll Surg. 1999; 189:177–182. PMID: 10437840.26. Jeng KS, Yang FS, Ohta I, Chiang HJ. Dilatation of intrahepatic biliary strictures in patients with hepatolithiasis. World J Surg. 1990; 14:587–592. PMID: 2238657.
Article27. Jeng KS, Yang FS, Chiang HJ, Ohta I. Bile duct stents in the management of hepatolithiasis with long-segment intrahepatic biliary strictures. Br J Surg. 1992; 79:663–666. PMID: 1643480.
Article28. Nakanuma Y, Terada T, Tanaka Y, Ohta G. Are hepatolithiasis and cholangiocarcinoma aetiologically related? A morphological study of 12 cases of hepatolithiasis associated with cholangiocarcinoma. Virchows Arch A Pathol Anat Histopathol. 1985; 406:45–58. PMID: 2986349.29. Rizvi S, Gores GJ. Pathogenesis, diagnosis, and management of cholangiocarcinoma. Gastroenterology. 2013; 145:1215–1229. PMID: 24140396.
Article30. Wakabayashi H, Akamoto S, Yachida S, Okano K, Izuishi K, Nishiyama Y, et al. Significance of fluorodeoxyglucose PET imaging in the diagnosis of malignancies in patients with biliary stricture. Eur J Surg Oncol. 2005; 31:1175–1179. PMID: 16019182.
Article31. Itatsu K, Zen Y, Ohira S, Ishikawa A, Sato Y, Harada K, et al. Immunohistochemical analysis of the progression of flat and papillary preneoplastic lesions in intrahepatic cholangiocarcinogenesis in hepatolithiasis. Liver Int. 2007; 27:1174–1184. PMID: 17919228.
Article32. Zen Y, Sasaki M, Fujii T, Chen TC, Chen MF, Yeh TS, et al. Different expression patterns of mucin core proteins and cytokeratins during intrahepatic cholangiocarcinogenesis from biliary intraepithelial neoplasia and intraductal papillary neoplasm of the bile duct--an immunohistochemical study of 110 cases of hepatolithiasis. J Hepatol. 2006; 44:350–358. PMID: 16360234.
Article33. Ohta T, Nagakawa T, Ueda N, Nakamura T, Akiyama T, Ueno K, et al. Mucosal dysplasia of the liver and the intraductal variant of peripheral cholangiocarcinoma in hepatolithiasis. Cancer. 1991; 68:2217–2223. PMID: 1655206.34. Sun WB, Han BL, Cai JX. The surgical treatment of isolated left-sided hepatolithiasis: a 22-year experience. Surgery. 2000; 127:493–497. PMID: 10819056.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Management of Hepatolithiasis
- Analysis of Surgical Treatments for Hepatolithiasis According to the Site of Biliary stenosis
- A Study of Factors Related to Recurrent Stones after Surgical Treatment of Hepatolithiasis
- Analysis on the Clinical Significance of Biliary Exploration through the Left Hepatic Duct Opening during Left Hepatectomy for the Patients with Hepatolithiasis
- New Surgical Technique for Bilateral Hepatolithiasis