Allergy Asthma Respir Dis.
2016 Nov;4(6):453-457. 10.4168/aard.2016.4.6.453.
Intrathoracic hemangioendothelioma presenting as refractory unilateral pleural effusion and thrombocytopenia
- Affiliations
-
- 1Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea. dongins0@snu.ac.kr
- 2Department of Pathology, Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Radiology, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2361262
- DOI: http://doi.org/10.4168/aard.2016.4.6.453
Abstract
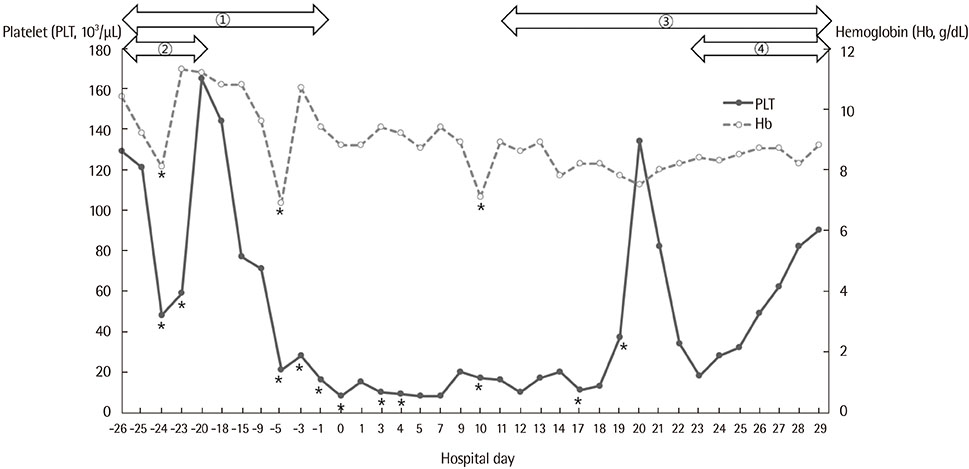
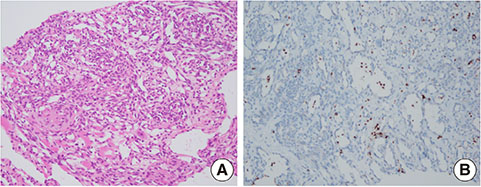
- A variety of diseases are associated with the development of unilateral pleural effusion. Although unilateral pleural effusion is common, refractory unilateral pleural effusion is rare. It is important to make an accurate diagnosis using proper diagnostic tools. Thrombocytopenia is one of the rare conditions occurring from various diseases such as severe infection or autoimmune diseases. It can be life-threatening if accurate diagnosis and treatment are delayed and be a clue to accurate diagnosis in differential diagnosis from refractory pleural effusion. Kasabach-Merrit syndrome (KMS) is often accompanied by extensive vascular tumors and characterized by consumptive coagulopathy with profound thrombocytopenia. It is also important to have a high index of suspicion for the diagnosis. We report a case of KMS in a 2-month-old female infant with a vascular tumor on her left intrathoracic cage, who had presented refractory unilateral pleural effusion and thrombocytopenia. Initially, the patient was diagnosed as having complications of severe infection, and a chest tube was inserted for aggressive treatment. However, her unilateral pleural effusion persisted, and thrombocytopenia and hypofibrinogenemia were refractory. Chest imaging revealed an infiltrating large vascular tumor involving the cardiac border, diaphragm, and chest wall. The patient's unilateral pleural effusion was misidentified as an infectious condition at the initial stage. As a result of the ultrasonography-guided biopsy, it was revealed to be Kaposiform hemangioendothelioma. The patient was cured after treatment for KMS.
MeSH Terms
Figure
Reference
-
1. Hooper C, Lee YC, Maskell N;. Investigation of a unilateral pleural effusion in adults: British Thoracic Society Pleural Disease Guideline 2010. Thorax. 2010; 65:Suppl 2. ii4–ii17.
Article2. Buckley MF, James JW, Brown DE, Whyte GS, Dean MG, Chesterman CN, et al. A novel approach to the assessment of variations in the human platelet count. Thromb Haemost. 2000; 83:480–484.
Article3. Sato T. Differential diagnosis of pleural effusions. Jpn Med Assoc J. 2006; 49:315–319.4. McGrath EE, Anderson PB. Diagnosis of pleural effusion: a systematic approach. Am J Crit Care. 2011; 20:119–127.
Article5. Broderick SR. Hemothorax: Etiology, diagnosis, and management. Thorac Surg Clin. 2013; 23:89–96.6. Varsano S, Edelstein E, Gendel B, Smorzik J. Bilateral and unilateral spontaneous massive hemothorax as a presenting manifestation of rare tumors. Respiration. 2003; 70:214–218.
Article7. Kumar S, Verma SK, Singh R, Prasad R. Hemorrhagic pleural effusion secondary to sarcoidosis: a brief review. Ann Thorac Med. 2009; 4:27–31.
Article8. Nanaware S, Gothi D, Joshi JM. Hemorrhagic pleural effusion due to pleural hemangioma. J Assoc Physicians India. 2003; 51:623–625.9. Croteau SE, Liang MG, Kozakewich HP, Alomari AI, Fishman SJ, Mulliken JB, et al. Kaposiform hemangioendothelioma: atypical features and risks of Kasabach-Merritt phenomenon in 107 referrals. J Pediatr. 2013; 162:142–147.
Article10. San Miguel FL, Spurbeck W, Budding C, Horton J. Kaposiform hemangioendothelioma: a rare cause of spontaneous hemothorax in infancy. Review of the literature. J Pediatr Surg. 2008; 43:e37–e41.
Article11. DeFatta RJ, Verret DJ, Adelson RT, Gomez A, Myers LL. Kaposiform hemangioendothelioma: case report and literature review. Laryngoscope. 2005; 115:1789–1792.
Article12. Lee JW, Jung HL, Shim JW, Kim DS, Shim JY, Park MS, et al. A case of Kasabach-Merritt Syndrome successfully treated with Interferon-alpha 2b and propranolol. Clin Pediatr Hematol Oncol. 2015; 22:161–166.
Article13. Hall GW. Kasabach-Merritt syndrome: pathogenesis and management. Br J Haematol. 2001; 112:851–862.
Article14. Fernández Y, Bernabeu-Wittel M, García-Morillo JS. Kaposiform hemangioendothelioma. Eur J Intern Med. 2009; 20:106–113.
Article15. Kelly M. Kasabach-Merritt phenomenon. Pediatr Clin North Am. 2010; 57:1085–1089.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Composite Epithelioid Hemangioendothelioma in Pleural Effusion Mimicking Metastatic Adenocarcinoma: Cytologic and Immunocytochemical Findings
- Refractory Pleural Effusion in Systemic Lupus Erythematosus Treated by Pleurectomy
- Congenital Chylothorax Diagnosed by in Utero Thoracentesis
- The clinical evaluation of pleural biopsy in the intrathoracic lesion with pleural effusion
- A Case of Mediastinal Teratoma Complicated by Spontaneous Rupture into Pleural Cavity