Brain Tumor Res Treat.
2016 Oct;4(2):111-115. 10.14791/btrt.2016.4.2.111.
Neurological Change after Gamma Knife Radiosurgery for Brain Metastases Involving the Motor Cortex
- Affiliations
-
- 1Department of Neurosurgery, Gamma Knife Center, Ajou University School of Medicine, Suwon, Korea. nsksh@ajou.ac.kr
- 2Department of Neurosurgery, Winjin Green Hospital, Seoul, Korea.
- KMID: 2356979
- DOI: http://doi.org/10.14791/btrt.2016.4.2.111
Abstract
- BACKGROUND
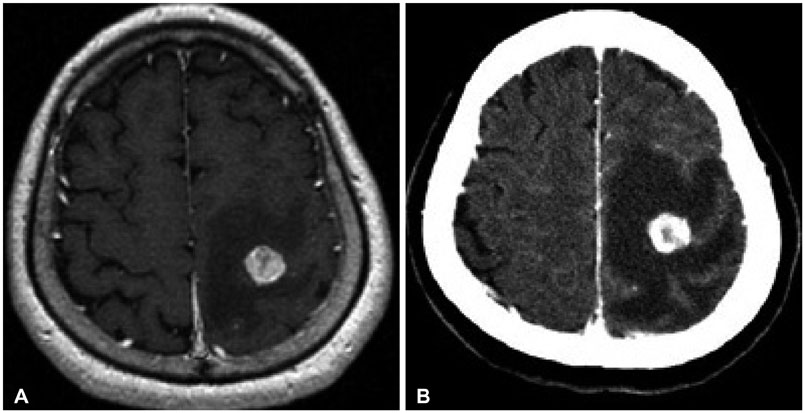
Although Gamma Knife radiosurgery (GKRS) can provide beneficial therapeutic effects for patients with brain metastases, lesions involving the eloquent areas carry a higher risk of neurologic deterioration after treatment, compared to those located in the non-eloquent areas. We aimed to investigate neurological change of the patients with brain metastases involving the motor cortex (MC) and the relevant factors related to neurological deterioration after GKRS.
METHODS
We retrospectively reviewed clinical, radiological and dosimetry data of 51 patients who underwent GKRS for 60 brain metastases involving the MC. Prior to GKRS, motor deficits existed in 26 patients (50.9%). The mean target volume was 3.2 cc (range 0.001-14.1) at the time of GKRS, and the mean prescription dose was 18.6 Gy (range 12-24 Gy).
RESULTS
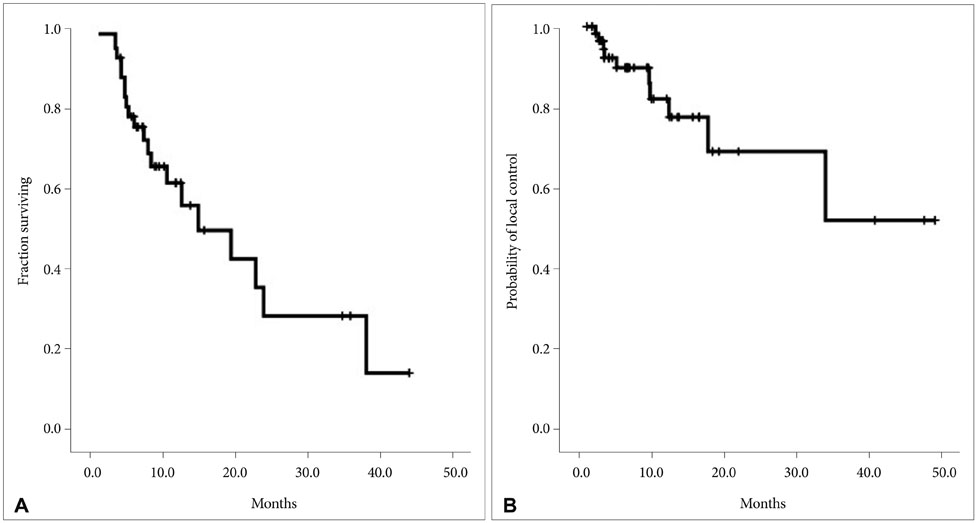
The actuarial median survival time from GKRS was 19.2±5.0 months. The calculated local tumor control rates at 6 and 12 months after GKRS were 89.7% and 77.4%, respectively. During the median clinical follow-up duration of 12.3±2.6 months (range 1-54 months), 18 patients (35.3%) experienced new or worsened neurologic deficits with a median onset time of 2.5±0.5 months (range 0.3-9.7 months) after GKRS. Among various factors, prescription dose (>20 Gy) was a significant factor for the new or worsened neurologic deficits in univariate (p=0.027) and multivariate (p=0.034) analysis. The managements of 18 patients were steroid medication (n=10), boost radiation therapy (n=5), and surgery (n=3), and neurological improvement was achieved in 9 (50.0%).
CONCLUSION
In our series, prescription dose (>20 Gy) was significantly related to neurological deterioration after GKRS for brain metastases involving the MC. Therefore, we suggest that careful dose adjustment would be required for lesions involving the MC to avoid neurological deterioration requiring additional treatment in the patients with limited life expectancy.
MeSH Terms
Figure
Reference
-
1. Hasegawa T, Kondziolka D, Flickinger JC, Germanwala A, Lunsford LD. Brain metastases treated with radiosurgery alone: an alternative to whole brain radiotherapy? Neurosurgery. 2003; 52:1318–1326. discussion 1326.
Article2. Joseph J, Adler JR, Cox RS, Hancock SL. Linear accelerator-based stereotaxic radiosurgery for brain metastases:the influence of number of lesions on survival. J Clin Oncol. 1996; 14:1085–1092.
Article3. Kondziolka D, Martin JJ, Flickinger JC, et al. Long-term survivors after gamma knife radiosurgery for brain metastases. Cancer. 2005; 104:2784–2791.
Article4. Kano H, Iyer A, Kondziolka D, Niranjan A, Flickinger JC, Lunsford LD. Outcome predictors of gamma knife radiosurgery for renal cell carcinoma metastases. Neurosurgery. 2011; 69:1232–1239.
Article5. Auchter RM, Lamond JP, Alexander E, et al. A multiinstitutional outcome and prognostic factor analysis of radiosurgery for resectable single brain metastasis. Int J Radiat Oncol Biol Phys. 1996; 35:27–35.
Article6. Davidson L, Zada G, Yu C, et al. Delayed toxicity from gamma knife radiosurgery to lesions in and adjacent to the brainstem. J Clin Neurosci. 2009; 16:1139–1147.
Article7. Dea N, Borduas M, Kenny B, Fortin D, Mathieu D. Safety and efficacy of Gamma Knife surgery for brain metastases in eloquent locations. J Neurosurg. 2010; 113:Suppl. 79–83.
Article8. Gaspar LE, Scott C, Murray K, Curran W. Validation of the RTOG recursive partitioning analysis (RPA) classification for brain metastases. Int J Radiat Oncol Biol Phys. 2000; 47:1001–1006.
Article9. Henson JW, Ulmer S, Harris GJ. Brain tumor imaging in clinical trials. AJNR Am J Neuroradiol. 2008; 29:419–424.
Article10. Molenaar R, Wiggenraad R, Verbeek-de Kanter A, Walchenbach R, Vecht C. Relationship between volume, dose and local control in stereotactic radiosurgery of brain metastasis. Br J Neurosurg. 2009; 23:170–178.
Article11. Petrovich Z, Yu C, Giannotta SL, O'Day S, Apuzzo ML. Survival and pattern of failure in brain metastasis treated with stereotactic gamma knife radiosurgery. J Neurosurg. 2002; 97:5 Suppl. 499–506.
Article12. Patchell RA, Tibbs PA, Walsh JW, et al. A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med. 1990; 322:494–500.
Article13. Mintz AH, Kestle J, Rathbone MP, et al. A randomized trial to assess the efficacy of surgery in addition to radiotherapy in patients with a single cerebral metastasis. Cancer. 1996; 78:1470–1476.
Article14. DeAngelis LM, Mandell LR, Thaler HT, et al. The role of postoperative radiotherapy after resection of single brain metastases. Neurosurgery. 1989; 24:798–805.
Article15. Gerosa M, Nicolato A, Foroni R, et al. Gamma knife radiosurgery for brain metastases: a primary therapeutic option. J Neurosurg. 2002; 97:5 Suppl. 515–524.
Article16. Gerosa M, Nicolato A, Foroni R. The role of gamma knife radiosurgery in the treatment of primary and metastatic brain tumors. Curr Opin Oncol. 2003; 15:188–196.
Article17. Mathieu D, Kondziolka D, Flickinger JC, et al. Tumor bed radiosurgery after resection of cerebral metastases. Neurosurgery. 2008; 62:817–823. discussion 823-4.
Article18. Luther N, Kondziolka D, Kano H, Mousavi SH, Flickinger JC, Lunsford LD. Motor function after stereotactic radiosurgery for brain metastases in the region of the motor cortex. J Neurosurg. 2013; 119:683–688.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Analysis of Gamma Knife Radiosurgery for Brain Metastases
- How to use Leksell GammaPlan
- Normal pressure hydrocephalus after gamma knife radiosurgery in a patient with vestibular schwannoma
- Letters to the Editor: Gamma Knife Radiosurgery for Brain Metastases in Patients Harboring Four or More Lesions : Survival and Prognostic Factors
- Gamma Knife Radiosurgery for Single & Multiple brain Metastasis