Korean J Neurotrauma.
2016 Oct;12(2):61-66. 10.13004/kjnt.2016.12.2.61.
The Effect of Preoperative Antiplatelet Therapy on Hemorrhagic Complications after Decompressive Craniectomy in Patients with Traumatic Brain Injury
- Affiliations
-
- 1Department of Neurosurgery, Dongguk University Ilsan Hospital, Goyang, Korea. ktcho21@naver.com
- KMID: 2356774
- DOI: http://doi.org/10.13004/kjnt.2016.12.2.61
Abstract
OBJECTIVE
Traditionally, it is generally recommended that antiplatelet agent should be discontinued before surgery. However, decompressive craniectomy (DC) in patients with traumatic brain injury (TBI) is performed emergently in most cases. Therefore, DC cannot be delayed to the time when the effect of antiplatelet agent on bleeding tendency dissipates. In this study, we evaluated the effect of preinjury antiplatelet therapy on hemorrhagic complications after emergent DC in patients with TBI.
METHODS
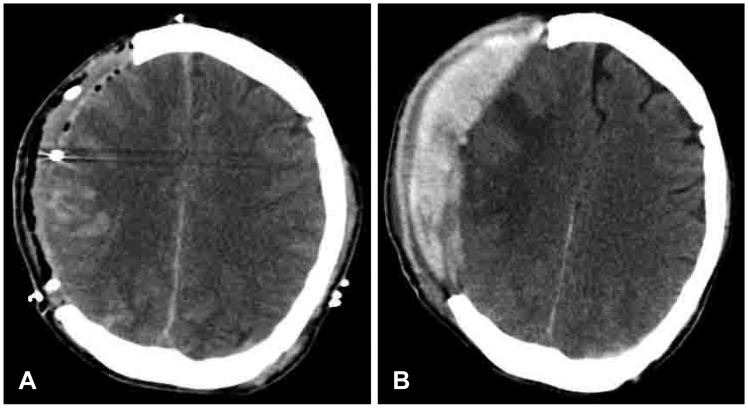
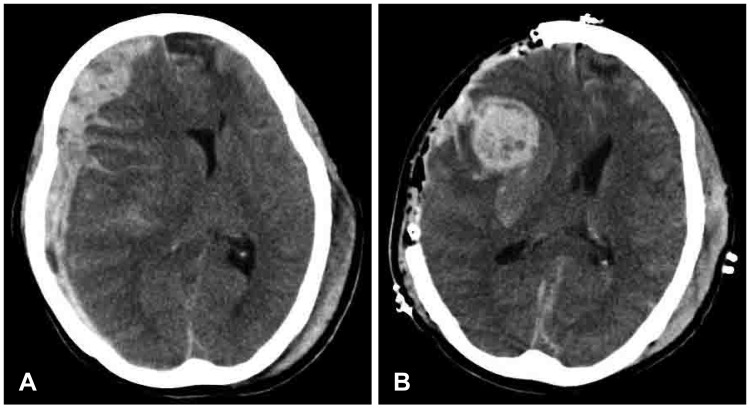
We retrospectively investigated patients with TBI who underwent emergent DC between 2006 and 2015. The patients were separated into two groups according to the use of preinjury antiplatelet agent: group 1 (patients taking antiplatelet agent) and group 2 (patients not taking antiplatelet agent). The rate of hemorrhagic complications (postoperative epidural or subdural hemorrhage, newly developed, or progression of preexisting contusion or intracerebral hemorrhage within the field of DC) and the rate of reoperation within 7 days after DC were compared between two groups.
RESULTS
During the study period, DC was performed in 90 patients. Of them, 19 patients were taking antiplatelet agent before TBI. The rate of hemorrhagic complications was 52.6% (10/19) in group 1 and 46.5% (33/71) in group 2 (p=0.633). The rate of reoperation was 36.8% (7/19) in group 1 and 36.6% (26/71) in group 2 (p=0.986). No statistical difference was found between two groups.
CONCLUSION
Preinjury antiplatelet therapy did not influence the rate of hemorrhagic complications and reoperation after DC. Emergent DC in patients with TBI should not be delayed because of preinjury antiplatelet therapy.
Keyword
MeSH Terms
Figure
Reference
-
1. Akhavan-Sigari R, Rohde V, Abili M. Continuation of medically necessary platelet aggregation inhibitors - acetylsalicylic acid and clopidogrel - during surgery for spinal degenerative disorders: Results in 100 patients. Surg Neurol Int. 2014; 5:S376–S379. PMID: 25289165.
Article2. Ban SP, Son YJ, Yang HJ, Chung YS, Lee SH, Han DH. Analysis of complications following decompressive craniectomy for traumatic brain injury. J Korean Neurosurg Soc. 2010; 48:244–250. PMID: 21082053.
Article3. Batchelor JS, Grayson A. A meta-analysis to determine the effect of preinjury antiplatelet agents on mortality in patients with blunt head trauma. Br J Neurosurg. 2013; 27:12–18. PMID: 22900511.
Article4. Bor-Seng-Shu E, Figueiredo EG, Amorim RL, Teixeira MJ, Valbuza JS, de Oliveira MM, et al. Decompressive craniectomy: a meta-analysis of influences on intracranial pressure and cerebral perfusion pressure in the treatment of traumatic brain injury. J Neurosurg. 2012; 117:589–596. PMID: 22794321.
Article5. Boyd CR, Tolson MA, Copes WS. Evaluating trauma care: the TRISS method. Trauma Score and the Injury Severity Score. J Trauma. 1987; 27:370–378. PMID: 3106646.6. Cull JD, Sakai LM, Sabir I, Johnson B, Tully A, Nagy K, et al. Outcomes in traumatic brain injury for patients presenting on antiplatelet therapy. Am Surg. 2015; 81:128–132. PMID: 25642873.
Article7. Devereaux PJ, Mrkobrada M, Sessler DI, Leslie K, Alonso-Coello P, Kurz A, et al. Aspirin in patients undergoing noncardiac surgery. N Engl J Med. 2014; 370:1494–1503. PMID: 24679062.8. Fleisher LA, Fleischmann KE, Auerbach AD, Barnason SA, Beckman JA, Bozkurt B, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014; 130:2215–2245. PMID: 25085962.
Article9. Joo MS, Ahn BM, Kim HJ, Mun HS, Kang MK, Choi SH, et al. Evaluation of feasible timing of elective noncardiac procedure after antiplatelet discontinuation in patients treated with antiplatelet agents. J Investig Med. 2014; 62:808–812.
Article10. Joseph B, Pandit V, Aziz H, Kulvatunyou N, Hashmi A, Tang A, et al. Clinical outcomes in traumatic brain injury patients on preinjury clopidogrel: a prospective analysis. J Trauma Acute Care Surg. 2014; 76:817–820. PMID: 24553554.11. Korinth MC, Gilsbach JM, Weinzierl MR. Low-dose aspirin before spinal surgery: results of a survey among neurosurgeons in Germany. Eur Spine J. 2007; 16:365–372. PMID: 16953446.
Article12. Ogawa Y, Tominaga T. Sellar and parasellar tumor removal without discontinuing antithrombotic therapy. J Neurosurg. 2015; 123:794–798. PMID: 25699416.
Article13. Palmer JD, Sparrow OC, Iannotti F. Postoperative hematoma: a 5-year survey and identification of avoidable risk factors. Neurosurgery. 1994; 35:1061–1064. discussion 1064-1065. PMID: 7885549.14. Park JH, Park JE, Kim SH, Lim YC, You NK, Ahn YH, et al. Outcomes of Ultra-Early Decompressive Craniectomy after Severe Traumatic Brain Injury-Treatment Outcomes after Severe TBI. Korean J Neurotrauma. 2014; 10:112–118. PMID: 27169044.
Article15. Rahman M, Donnangelo LL, Neal D, Mogali K, Decker M, Ahmed MM. Effects of Perioperative Acetyl Salicylic Acid on Clinical Outcomes in Patients Undergoing Craniotomy for Brain Tumor. World Neurosurg. 2015; 84:41–47. PMID: 25727304.
Article16. Rouine-Rapp K, McDermott MW. Perioperative management of a neurosurgical patient with a meningioma and recent coronary artery stent. J Clin Anesth. 2013; 25:228–231. PMID: 23688961.
Article17. Schuss P, Borger V, Vatter H, Singer OC, Seifert V, Guresir E. Antiplatelet therapy, but not intravenous thrombolytic therapy, is associated with postoperative bleeding complications after decompressive craniectomy for stroke. J Neurol. 2013; 260:2149–2155. PMID: 23712799.
Article18. Stiver SI. Complications of decompressive craniectomy for traumatic brain injury. Neurosurg Focus. 2009; 26:E7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Decompressive Craniectomy in Traumatic Brain Injury: A Review Article
- The relationship between the serum lactate level and in-hospital mortality after decompressive craniectomy in traumatic brain Injury
- Analysis of Complications Following Decompressive Craniectomy for Traumatic Brain Injury
- Paradoxical Herniation after Decompressive Craniectomy for Acute Subdural Hematoma
- Post-Traumatic Cerebral Infarction Following Low-Energy Penetrating Craniocerebral Injury Caused by a Nail