Ann Rehabil Med.
2016 Aug;40(4):734-740. 10.5535/arm.2016.40.4.734.
Progressive Bilateral Facial Palsy as a Manifestation of Granulomatosis With Polyangiitis: A Case Report
- Affiliations
-
- 1Department of Rehabilitation Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea. drlee71@naver.com
- KMID: 2356660
- DOI: http://doi.org/10.5535/arm.2016.40.4.734
Abstract
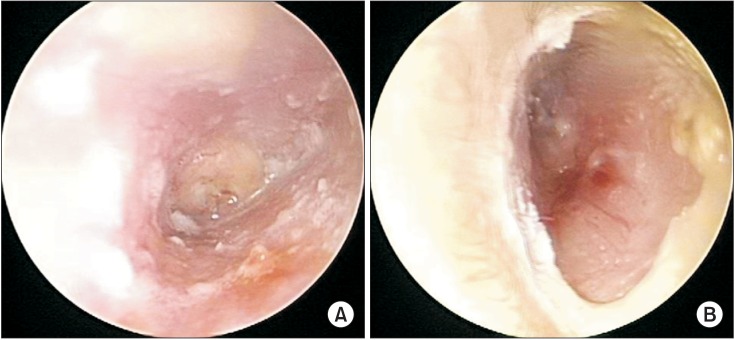
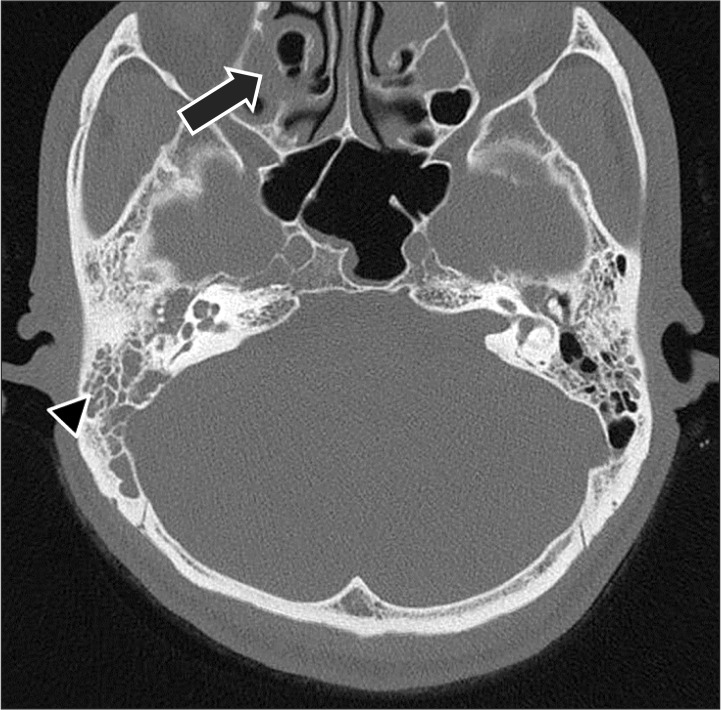
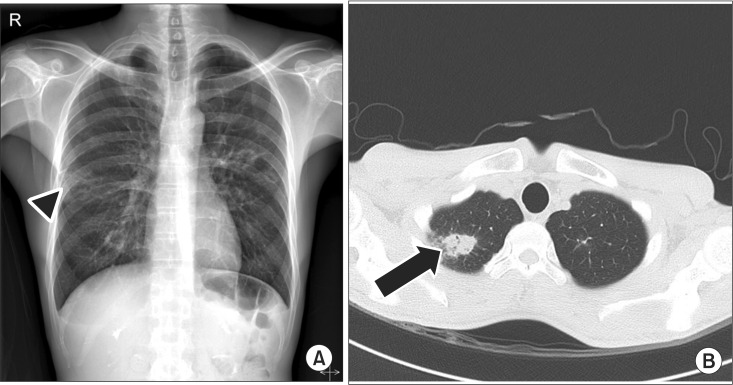
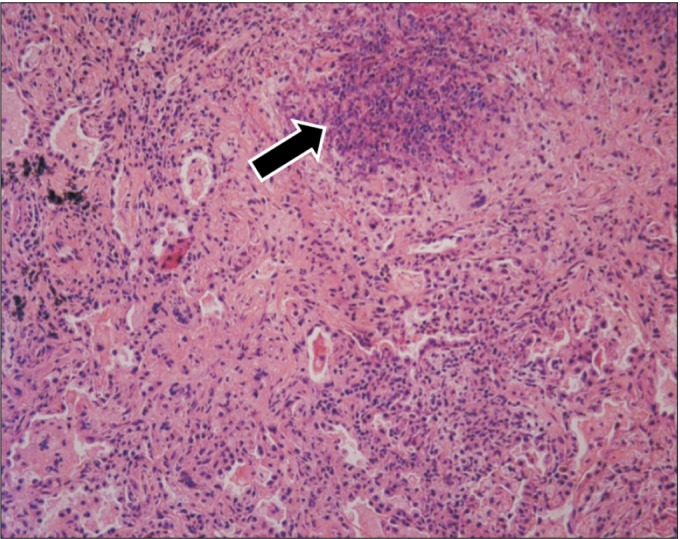
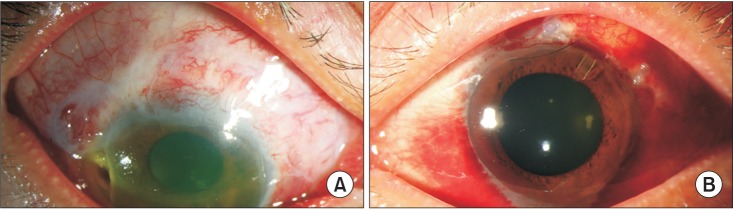
- Bilateral facial palsy, which is usually combined with other diseases, occurs infrequently. It may imply a life-threatening condition. Therefore, the differential diagnosis of bilateral facial palsy is important. However, the etiology is variable, which makes diagnosis challenging. We report a rare case of progressive bilateral facial palsy as a manifestation of granulomatosis with polyangiitis (GPA). A 40-year-old male with otitis media and right facial palsy was referred for electroneurography (ENoG), which showed a 7.7% ENoG. Left facial palsy occurred after 2 weeks, and multiple cavitary opacities were noted on chest images. GPA was diagnosed by lung biopsy. His symptoms deteriorated and mononeuropathy multiplex developed. The possibility of systemic disease, such as GPA, should be considered in patients presenting with bilateral facial palsy, the differential diagnosis of which is summarized in this report.
MeSH Terms
Figure
Reference
-
1. Oosterveer DM, Benit CP, de Schryver EL. Differential diagnosis of recurrent or bilateral peripheral facial palsy. J Laryngol Otol. 2012; 126:833–836. PMID: 22804856.
Article2. Pothiawala S, Lateef F. Bilateral facial nerve palsy: a diagnostic dilemma. Case Rep Emerg Med. 2012; 2012:458371. PMID: 23326715.
Article3. Jain V, Deshmukh A, Gollomp S. Bilateral facial paralysis: case presentation and discussion of differential diagnosis. J Gen Intern Med. 2006; 21:C7–C10. PMID: 16808763.
Article4. May M, Klein SR. Differential diagnosis of facial nerve palsy. Otolaryngol Clin North Am. 1991; 24:613–645. PMID: 1762779.
Article5. Lee MG, Cho YH. Lyme disease. J Korean Med Assoc. 2004; 47:1063–1069.
Article6. Maranhao AS, Chen VG, Rossini BA, Testa JR, Penido Nde O. Mastoiditis and facial paralysis as initial manifestations of Wegener's Granulomatosis. Braz J Otorhinolaryngol. 2012; 78:80–86. PMID: 22499374.7. Hoffman GS, Kerr GS, Leavitt RY, Hallahan CW, Lebovics RS, Travis WD, et al. Wegener granulomatosis: an analysis of 158 patients. Ann Intern Med. 1992; 116:488–498. PMID: 1739240.
Article8. Takagi D, Nakamaru Y, Maguchi S, Furuta Y, Fukuda S. Otologic manifestations of Wegener's granulomatosis. Laryngoscope. 2002; 112:1684–1690. PMID: 12352687.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Wegener's Granulomatosis Presenting as Bilateral Otalgia with Facial Palsy: A Case Report
- Refractory Granulomatosis with Polyangiitis Presenting as Facial Paralysis and Bilateral Sudden Deafness
- A Case of Unilateral Otologic Symptoms as Initial Manifestations of Granulomatosis With Polyangiitis
- A Case of Bilateral Bell's Palsy with Uncontrolled Diabetes Mellitus
- Facial Palsy as a Presenting Symptom of Wegener's Granulomatosis