Ann Rehabil Med.
2016 Aug;40(4):575-582. 10.5535/arm.2016.40.4.575.
Phantom Study of a New Laser-Etched Needle for Improving Visibility During Ultrasonography-Guided Lumbar Medial Branch Access With Novices
- Affiliations
-
- 1Topteam Rehabilitation Clinic, Gwangju, Korea.
- 2Department of Hospital Biomedical Engineering, Dongshin University, Gwangju, Korea.
- 3Department of Rehabilitation Medicine, Chosun University Hospital, Gwangju, Korea. hayaaaa@hanmail.net
- KMID: 2356642
- DOI: http://doi.org/10.5535/arm.2016.40.4.575
Abstract
OBJECTIVE
To compare the visibility and procedural parameters between a standard spinal needle and a new laser-etched needle (LEN) in real-time ultrasonography guided lumbar medial branch access in a phantom of the lumbosacral spine.
METHODS
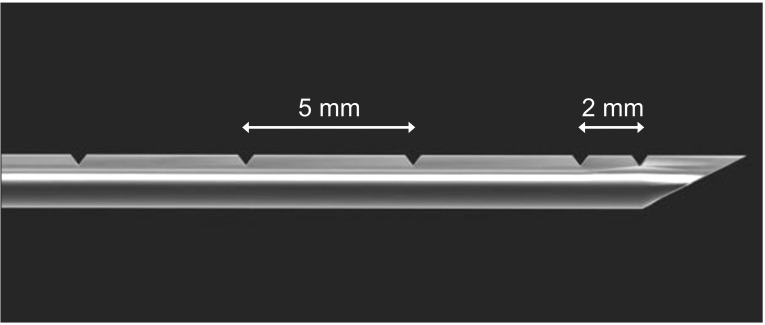
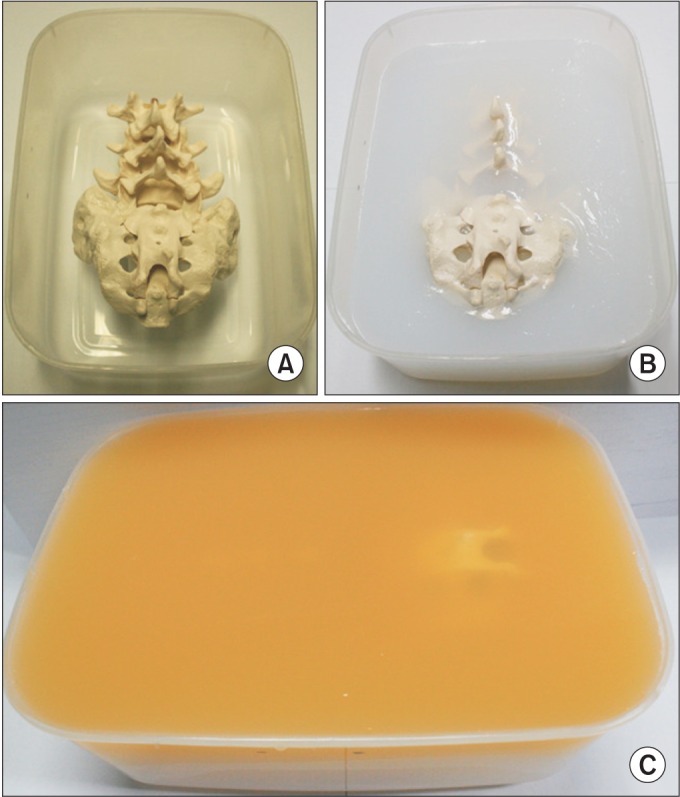
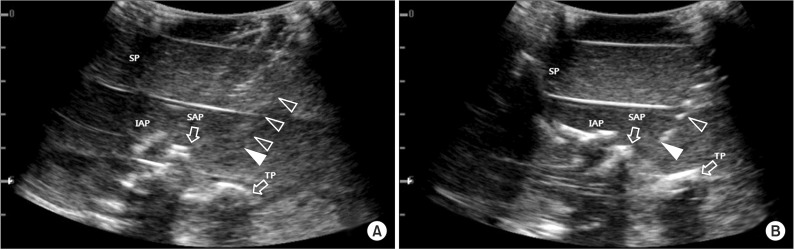
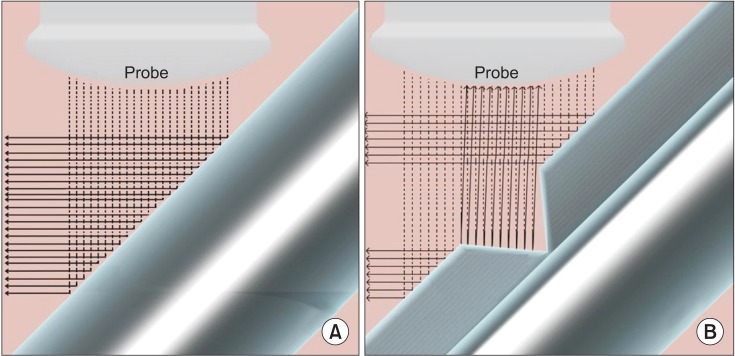
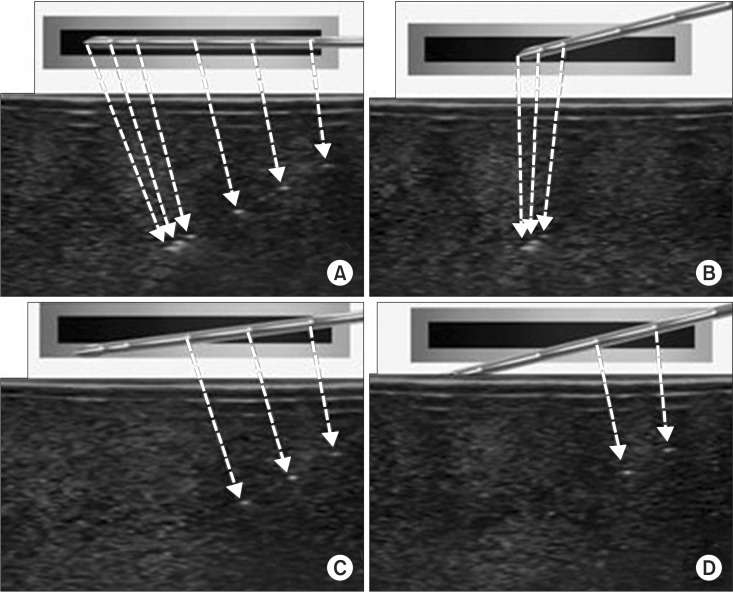
We conducted a prospective single-blinded observational study at a rehabilitation medicine center. A new model of LEN was manufactured with a standard 22-gauge spinal needle and a laser etching machine. Thirty-two inexperienced polyclinic medical students performed ultrasonography-guided lumbar medial branch access using both a standard spinal needle and a LEN with scanning protocol. The outcomes included needle visibility score, needle elapsed time, first-pass success rate, and number of needle sticks.
RESULTS
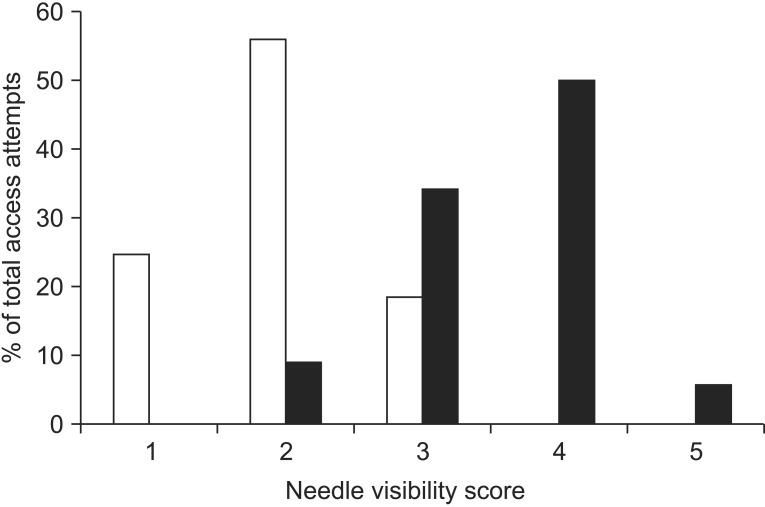
The LEN received significantly better visibility scores and shorter needle elapsed time compared to the standard spinal needle. First-pass success rate and the number of needle sticks were not significantly different between needles.
CONCLUSION
A new LEN is expected to offer better visibility and enable inexperienced users to perform an ultrasonography-guided lumbar medial branch block more quickly. However, further study of variables may be necessary for clinical application.
MeSH Terms
Figure
Reference
-
1. Greher M, Scharbert G, Kamolz LP, Beck H, Gustorff B, Kirchmair L, et al. Ultrasound-guided lumbar facet nerve block: a sonoanatomic study of a new methodologic approach. Anesthesiology. 2004; 100:1242–1248. PMID: 15114223.2. Saal JS. General principles of diagnostic testing as related to painful lumbar spine disorders: a critical appraisal of current diagnostic techniques. Spine (Phila Pa 1976). 2002; 27:2538–2545. PMID: 12435989.3. Ha DH, Shim DM, Kim TK, Kim YM, Choi SS. Comparison of ultrasonography- and fluoroscopy-guided facet joint block in the lumbar spine. Asian Spine J. 2010; 4:15–22. PMID: 20622950.
Article4. Kaplan M, Dreyfuss P, Halbrook B, Bogduk N. The ability of lumbar medial branch blocks to anesthetize the zygapophysial joint: a physiologic challenge. Spine (Phila Pa 1976). 1998; 23:1847–1852. PMID: 9762741.5. Chin KJ, Perlas A, Chan VW, Brull R. Needle visualization in ultrasound-guided regional anesthesia: challenges and solutions. Reg Anesth Pain Med. 2008; 33:532–544. PMID: 19258968.
Article6. Crum T, Adhikari S, Lander L, Blaivas M. Do echo-enhanced needles make a difference in sonographically guided vascular access? J Ultrasound Med. 2014; 33:623–628. PMID: 24658941.
Article7. Kilicaslan A, Topal A, Tavlan A, Erol A, Otelcioglu S. Differences in tip visibility and nerve block parameters between two echogenic needles during a simulation study with inexperienced anesthesia trainees. J Anesth. 2014; 28:460–462. PMID: 24127134.
Article8. Marks R, Semple AJ. Spinal anaesthesia after facet joint injection. Anaesthesia. 1988; 43:65–66. PMID: 3344957.
Article9. Sites BD, Spence BC, Gallagher JD, Wiley CW, Bertrand ML, Blike GT. Characterizing novice behavior associated with learning ultrasound-guided peripheral regional anesthesia. Reg Anesth Pain Med. 2007; 32:107–115. PMID: 17350520.
Article10. Gottlieb RH, Robinette WB, Rubens DJ, Hartley DF, Fultz PJ, Violante MR. Coating agent permits improved visualization of biopsy needles during sonography. AJR Am J Roentgenol. 1998; 171:1301–1302. PMID: 9798867.
Article11. Culp WC, McCowan TC, Goertzen TC, Habbe TG, Hummel MM, LeVeen RF, et al. Relative ultrasonographic echogenicity of standard, dimpled, and polymeric-coated needles. J Vasc Interv Radiol. 2000; 11:351–358. PMID: 10735431.
Article12. Barr RG. Improved needle visualization with electronic beam steering: proof of concept. Ultrasound Q. 2012; 28:59–64. PMID: 22634767.13. Hocking G, Mitchell CH. Optimizing the safety and practice of ultrasound-guided regional anesthesia: the role of echogenic technology. Curr Opin Anaesthesiol. 2012; 25:603–609. PMID: 22825047.14. Edgcombe H, Hocking G. Sonographic identification of needle tip by specialists and novices: a blinded comparison of 5 regional block needles in fresh human cadavers. Reg Anesth Pain Med. 2010; 35:207–211. PMID: 20301826.15. Uppal V, Sondekoppam RV, Ganapathy S. Effect of beam steering on the visibility of echogenic and non-echogenic needles: a laboratory study. Can J Anaesth. 2014; 61:909–915. PMID: 25053210.
Article16. Bellingham GA, Peng PW. A low-cost ultrasound phantom of the lumbosacral spine. Reg Anesth Pain Med. 2010; 35:290–293. PMID: 20921841.
Article17. Kendall JL, Faragher JP. Ultrasound-guided central venous access: a homemade phantom for simulation. CJEM. 2007; 9:371–373. PMID: 17935654.
Article18. Greher M, Kirchmair L, Enna B, Kovacs P, Gustorff B, Kapral S, et al. Ultrasound-guided lumbar facet nerve block: accuracy of a new technique confirmed by computed tomography. Anesthesiology. 2004; 101:1195–1200. PMID: 15505456.19. Guo S, Schwab A, McLeod G, Corner G, Cochran S, Eisma R, et al. Echogenic regional anaesthesia needles: a comparison study in Thiel cadavers. Ultrasound Med Biol. 2012; 38:702–707. PMID: 22390992.
Article20. Rauch S, Kasuya Y, Turan A, Neamtu A, Vinayakan A, Sessler DI. Ultrasound-guided lumbar medial branch block in obese patients: a fluoroscopically confirmed clinical feasibility study. Reg Anesth Pain Med. 2009; 34:340–342. PMID: 19585701.21. Miura M, Takeyama K, Suzuki T. Visibility of ultrasound-guided echogenic needle and its potential in clinical delivery of regional anesthesia. Tokai J Exp Clin Med. 2014; 39:80–86. PMID: 25027252.22. Sviggum HP, Ahn K, Dilger JA, Smith HM. Needle echogenicity in sonographically guided regional anesthesia: blinded comparison of 4 enhanced needles and validation of visual criteria for evaluation. J Ultrasound Med. 2013; 32:143–148. PMID: 23269719.23. Gofeld M, Krashin DL, Ahn S. Needle echogenicity in ultrasound-guided lumbar spine injections: a cadaveric study. Pain Physician. 2013; 16:E725–E730. PMID: 24284853.24. Deam RK, Kluger R, Barrington MJ, McCutcheon CA. Investigation of a new echogenic needle for use with ultrasound peripheral nerve blocks. Anaesth Intensive Care. 2007; 35:582–586. PMID: 18020079.
Article25. Maecken T, Zenz M, Grau T. Ultrasound characteristics of needles for regional anesthesia. Reg Anesth Pain Med. 2007; 32:440–447. PMID: 17961844.
Article26. Schafhalter-Zoppoth I, McCulloch CE, Gray AT. Ultrasound visibility of needles used for regional nerve block: an in vitro study. Reg Anesth Pain Med. 2004; 29:480–488. PMID: 15372394.27. Nichols K, Wright LB, Spencer T, Culp WC. Changes in ultrasonographic echogenicity and visibility of needles with changes in angles of insonation. J Vasc Interv Radiol. 2003; 14:1553–1557. PMID: 14654490.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasound Phantoms to Protect Patients from Novices
- Burn Wound along the Guide Needle Trajectory as a Complication of Radiofrequency Neurotomy of the Lumbar Medial Branch: A case report
- Transverse Process and Needles of Medial Branch Block to Facet Joint as Landmarks for Ultrasound-Guided Selective Nerve Root Block
- Measuring Needle Angle and Depth for Lumbar Medial Branch Block Using Ultrasonography: An Evaluation of Efficiency Compared with Magnetic Resonance Imaging
- Comparison of Lidocaine and Bupivacaine in Lumbar Medial Branch Block