J Korean Soc Radiol.
2016 Nov;75(5):354-362. 10.3348/jksr.2016.75.5.354.
Evaluation of Dual-Input Perfusion in Lung Cancer Using a 320-Detector CT: Its Correlation with Tumor Size, Location, and Presence of Metastasis
- Affiliations
-
- 1Department of Radiology, Dong-A University College of Medicine, Busan, Korea. gnlee@dau.ac.kr
- 2Department of Radiology, Dongnam Institute of Radiological & Medical Sciences, Busan, Korea.
- 3Department of Pathology, Dong-A University College of Medicine, Busan, Korea.
- 4Department of Internal Medicine, Dong-A University College of Medicine, Busan, Korea.
- KMID: 2355989
- DOI: http://doi.org/10.3348/jksr.2016.75.5.354
Abstract
- PURPOSE
The purposes of our study were to assess the dual blood supply of lung cancer using a computed tomography (CT) perfusion technique, and to analyze the correlations between dual perfusion and various characteristics of lung cancer.
MATERIALS AND METHODS
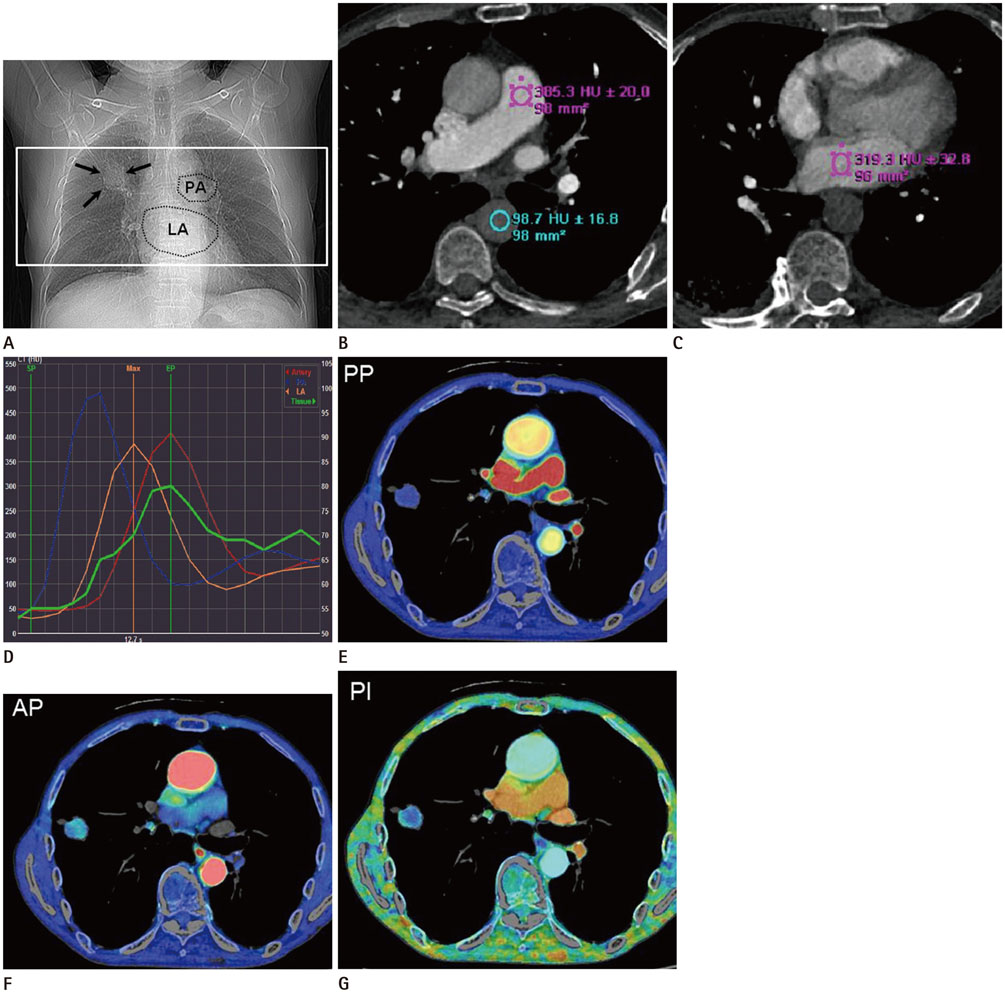
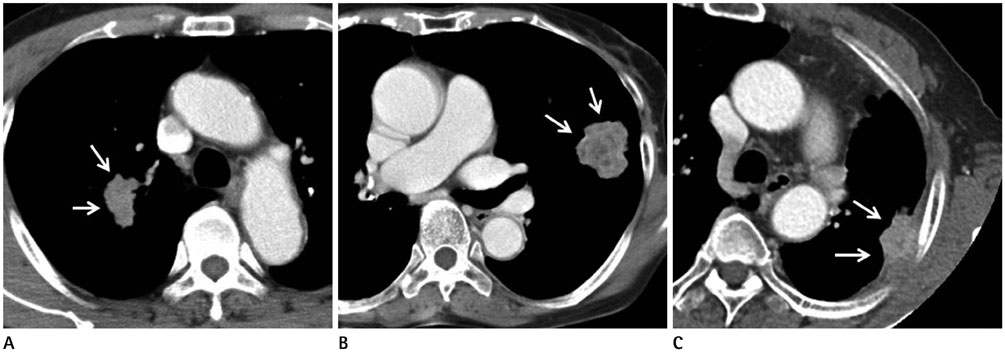
Thirty-five consecutive patients with lung tumors highly suggestive of malignancy were included in this study. All subjects underwent a dual-input dynamic perfusion volume scan using a 320-detector-row CT before CT-guided biopsy. The pulmonary trunk and the descending thoracic aorta were selected for the arterial input functions. From the CT data, pulmonary arterial perfusion (PP), aortic perfusion (AP), and the perfusion index [PI = PP / (PP + AP)] were calculated using the dual-input maximum-slope method. We statistically analyzed the relationship of the perfusion data with tumor locations (central, peripheral, and abutting the pleural lesions), tumor volumes, and the presence of lymph node metastasis or distant metastasis.
RESULTS
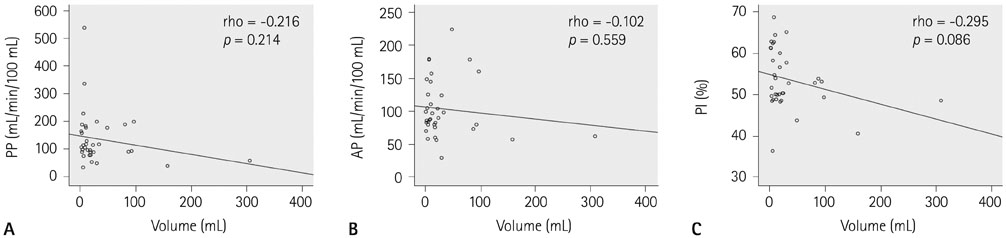
All subjects were pathologically diagnosed with primary lung cancers via CT-guided aspiration biopsy. The overall mean PI was 53.7 ± 7.2%. The PI showed a significant difference according to the tumor location (central, 49.2 ± 3.3%; peripheral, 56.2 ± 6.7%; abutting the pleural lesions, 48.9 ± 7.6%, p = 0.047). In contrast, no significant difference was detected in tumor size or the presence of metastasis (p > 0.05).
CONCLUSION
We found that the proportion of dual perfusion in lung cancer was significantly dependent on the location of the tumor, while tumor size or the presence of metastasis was not distinctly associated with dual perfusion.
MeSH Terms
Figure
Reference
-
1. Ogilvie RW, Blanding JD jr, Wood ML, Knisely WH. The arterial supply to experimental metastatic VX2 and XY tumors in rabbit lungs. Cancer Res. 1964; 24:1418–1431.2. Milne EN. Circulation of primary and metastatic pulmonary neoplasms. A postmortem microarteriographic study. Am J Roentgenol Radium Ther Nucl Med. 1967; 100:603–619.3. Kiessling F, Boese J, Corvinus C, Ederle JR, Zuna I, Schoenberg SO, et al. Perfusion CT in patients with advanced bronchial carcinomas: a novel chance for characterization and treatment monitoring? Eur Radiol. 2004; 14:1226–1233.4. Li Y, Yang ZG, Chen TW, Deng YP, Yu JQ, Li ZL. Whole tumour perfusion of peripheral lung carcinoma: evaluation with first-pass CT perfusion imaging at 64-detector row CT. Clin Radiol. 2008; 63:629–635.5. Ohno Y, Koyama H, Matsumoto K, Onishi Y, Takenaka D, Fujisawa Y, et al. Differentiation of malignant and benign pulmonary nodules with quantitative first-pass 320-detector row perfusion CT versus FDG PET/CT. Radiology. 2011; 258:599–609.6. Tacelli N, Remy-Jardin M, Copin MC, Scherpereel A, Mensier E, Jaillard S, et al. Assessment of non-small cell lung cancer perfusion: pathologic-CT correlation in 15 patients. Radiology. 2010; 257:863–871.7. Yuan X, Zhang J, Ao G, Quan C, Tian Y, Li H. Lung cancer perfusion: can we measure pulmonary and bronchial circulation simultaneously? Eur Radiol. 2012; 22:1665–1671.8. Yuan X, Zhang J, Quan C, Cao J, Ao G, Tian Y, et al. Differentiation of malignant and benign pulmonary nodules with first-pass dual-input perfusion CT. Eur Radiol. 2013; 23:2469–2474.9. Christner JA, Kofler JM, McCollough CH. Estimating effective dose for CT using dose-length product compared with using organ doses: consequences of adopting International Commission on Radiological Protection publication 103 or dual-energy scanning. AJR Am J Roentgenol. 2010; 194:881–889.10. McCullagh A, Rosenthal M, Wanner A, Hurtado A, Padley S, Bush A. The bronchial circulation--worth a closer look: a review of the relationship between the bronchial vasculature and airway inflammation. Pediatr Pulmonol. 2010; 45:1–13.11. Park HS, Kim YI, Kim HY, Zo JI, Lee JH, Lee JS. Bronchial artery and systemic artery embolization in the management of primary lung cancer patients with hemoptysis. Cardiovasc Intervent Radiol. 2007; 30:638–643.12. Miles KA, Hayball MP, Dixon AK. Functional images of hepatic perfusion obtained with dynamic CT. Radiology. 1993; 188:405–411.13. Blomley MJ, Coulden R, Dawson P, Kormano M, Donlan P, Bufkin C, et al. Liver perfusion studied with ultrafast CT. J Comput Assist Tomogr. 1995; 19:424–433.14. Tsushima Y, Funabasama S, Aoki J, Sanada S, Endo K. Quantitative perfusion map of malignant liver tumors, created from dynamic computed tomography data. Acad Radiol. 2004; 11:215–223.15. Nakano S, Gibo J, Fukushima Y, Kaira K, Sunaga N, Taketomi-Takahashi A, et al. Perfusion evaluation of lung cancer: assessment using dual-input perfusion computed tomography. J Thorac Imaging. 2013; 28:253–262.16. Yamazaki K, Abe S, Takekawa H, Sukoh N, Watanabe N, Ogura S, et al. Tumor angiogenesis in human lung adenocarcinoma. Cancer. 1994; 74:2245–2250.17. Yano T, Tanikawa S, Fujie T, Masutani M, Horie T. Vascular endothelial growth factor expression and neovascularisation in non-small cell lung cancer. Eur J Cancer. 2000; 36:601–609.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparative Analysis of Lung Perfusion Scan and SPECT/CT for the Evaluation of Functional Lung Capacity
- Mediastinal and Hilar Lymphadenopathy: Cross-Referenced Anatomy on Axial and Coronal Images Displayed by Using Multi-detector row CT
- Advanced Gastric Cancer and Perfusion Imaging Using a Multidetector Row Computed Tomography: Correlation with Prognostic Determinants
- CT evaluation of cavitary lung lesions: focused of lung cancer, tuberculosis and abscess
- CT Findings of Atypical Carcinoid Tumor of the Lung