J Korean Med Sci.
2016 Dec;31(12):1963-1968. 10.3346/jkms.2016.31.12.1963.
Analysis of Malpractice Claims Associated with Surgical Site Infection in the Field of Plastic Surgery
- Affiliations
-
- 1Department of Plastic Surgery, Ewha Womans University Mokdong Hospital, Seoul, Korea. monkeyhong@hanmail.net
- KMID: 2355626
- DOI: http://doi.org/10.3346/jkms.2016.31.12.1963
Abstract
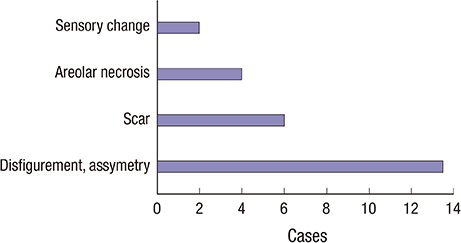
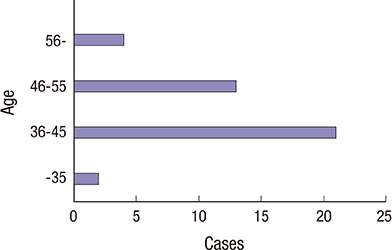
- Postoperative infections are rare after plastic surgery; however, when present, they can affect the aesthetic outcome. Currently, many malpractice lawsuits are associated with surgical site infection. The present study aimed to analyze malpractice claims associated with surgical site infection in the field of plastic surgery through a review of Korean precedents. We analyzed the type of procedure, associated complications, and legal judgment in these cases. Most claimants were women, and claims were most often related to breast surgery. The common complications related to surgical site infection were deformity, scar, and asymmetry. Among the 40 cases, 34 were won by the plaintiff, and the mean claim settlement was 2,832,654 KRW (USD 2,636.6). The reasons for these judgements were as follows: 1) immediate bacterial culture tests were not performed and appropriate antibiotics were not used; 2) patients were not transferred to a high-level hospital or the infection control department was not consulted; 3) surgical site infection control measures were not appropriate; and 4) surgical procedures were performed without preoperative explanation about surgical site infection. The number of claims owing to surgical site infection after surgery is increasing. Infection handling was one of the key factors that influenced the judgement, and preoperative explanation about the possibility of infection is important. The findings will help surgeons achieve high patient satisfaction and reduce liability concerns.
MeSH Terms
Figure
Cited by 2 articles
-
Analysis of Judicial Precedents Cases Regarding Skin Cancer from 1997 to 2017 in Republic of Korea
Su Hwan Shin, Won Lee, So Yoon Kim, Gwanghyun Jo, Je-Ho Mun, Soo Ick Cho
Ann Dermatol. 2019;31(3):300-306. doi: 10.5021/ad.2019.31.3.300.Analysis of closed medical litigation in urology
Su Hwan Shin, So Yoon Kim, Seung Gyeong Jang, Won Lee
Investig Clin Urol. 2017;58(5):317-323. doi: 10.4111/icu.2017.58.5.317.
Reference
-
1. Bratzler DW, Houck PM; Surgical Infection Prevention Guideline Writers Workgroup. Antimicrobial prophylaxis for surgery: an advisory statement from the National Surgical Infection Prevention Project. Am J Surg. 2005; 189:395–404.2. Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG. CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infect Control Hosp Epidemiol. 1992; 13:606–608.3. Emori TG, Gaynes RP. An overview of nosocomial infections, including the role of the microbiology laboratory. Clin Microbiol Rev. 1993; 6:428–442.4. Bratzler DW, Dellinger EP, Olsen KM, Perl TM, Auwaerter PG, Bolon MK, Fish DN, Napolitano LM, Sawyer RG, Slain D, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Surg Infect (Larchmt). 2013; 14:73–156.5. Lyden JR, Dellinger EP. Surgical site infections. Hosp Med Clin. 2016; 5:319–333.6. Cheadle WG. Risk factors for surgical site infection. Surg Infect (Larchmt). 2006; 7:Suppl 1. S7–11.7. Ahmadi AH, Cohen BE, Shayani P. A prospective study of antibiotic efficacy in preventing infection in reduction mammaplasty. Plast Reconstr Surg. 2005; 116:126–131.8. Peled IJ, Dvir G, Berger J, Ramon I, Ullmann Y, Nachlieli T. Prophylactic antibiotics in aesthetic and reconstructive surgery. Aesthetic Plast Surg. 2000; 24:299–302.9. LeRoy JL Jr, Rees TD, Nolan WB 3rd. Infections requiring hospital readmission following face lift surgery: incidence, treatment, and sequelae. Plast Reconstr Surg. 1994; 93:533–536.10. Meyers AD. Prophylactic antibiotics in nasal surgery. Arch Otolaryngol Head Neck Surg. 1990; 116:1125–1126.11. Choi JH. Legal aspects on nosocomial infection. Korean J Med. 2009; 76:Suppl 2. S286–9.12. Kompatscher P, von Planta A, Spicher I, Seifert B, Vetter S, Minder J, Beer GM. Comparison of the incidence and predicted risk of early surgical site infections after breast reduction. Aesthetic Plast Surg. 2003; 27:308–314.13. Tejirian T, DiFronzo LA, Haigh PI. Antibiotic prophylaxis for preventing wound infection after breast surgery: a systematic review and metaanalysis. J Am Coll Surg. 2006; 203:729–734.14. Mioton LM, Jordan SW, Hanwright PJ, Bilimoria KY, Kim JY. The relationship between preoperative wound classification and postoperative infection: a multi-institutional analysis of 15,289 patients. Arch Plast Surg. 2013; 40:522–529.15. Thomassin JM, Bardot J, Radulesco T. Rhinoplasty: medicolegal issues. Ann Chir Plast Esthet. 2014; 59:592–595.16. Reisman NR. Medicolegal issues in breast reduction. Clin Plast Surg. 2016; 43:441–444.17. White AA, Pichert JW, Bledsoe SH, Irwin C, Entman SS. Cause and effect analysis of closed claims in obstetrics and gynecology. Obstet Gynecol. 2005; 105:1031–1038.18. Ward CJ. Analysis of 500 obstetric and gynecologic malpractice claims: causes and prevention. Am J Obstet Gynecol. 1991; 165:298–304.19. Gravante G, Caruso R, Araco A, Cervelli V. Infections after plastic procedures: incidences, etiologies, risk factors, and antibiotic prophylaxis. Aesthetic Plast Surg. 2008; 32:243–251.20. Gorney M. Avoiding litigation in breast modification. Plast Reconstr Surg. 2011; 127:2113–2115.21. Lee JH. Where is your real face? News article [Internet]. accessed on 20 June 2016. Available at http://premium.chosun.com/site/data/html_dir/2014/08/16/2014081600184.html.22. Recht A, Come SE, Henderson IC, Gelman RS, Silver B, Hayes DF, Shulman LN, Harris JR. The sequencing of chemotherapy and radiation therapy after conservative surgery for early-stage breast cancer. N Engl J Med. 1996; 334:1356–1361.23. Bratzler DW, Dellinger EP, Olsen KM, Perl TM, Auwaerter PG, Bolon MK, Fish DN, Napolitano LM, Sawyer RG, Slain D, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health Syst Pharm. 2013; 70:195–283.24. Pittet B, Montandon D, Pittet D. Infection in breast implants. Lancet Infect Dis. 2005; 5:94–106.25. Gabriel SE, Woods JE, O’Fallon WM, Beard CM, Kurland LT, Melton LJ 3rd. Complications leading to surgery after breast implantation. N Engl J Med. 1997; 336:677–682.26. International Society of Aesthetic Plastic Surgery (US). ISAPS international survey on esthetic/cosmetic: procedures performed in 2014 [Internet]. accessed on 24 July 2016. Available at http://www.isaps.org/Media/Default/global-statistics/2015%20ISAPS%20Results.pdf.27. Tablan OC, Anderson LJ, Besser R, Bridges C, Hajjeh R. CDC; Healthcare Infection Control Practices Advisory Committee. Guidelines for preventing health-care--associated pneumonia, 2003: recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee. MMWR Recomm Rep. 2004; 53:1–36.28. Mojon P. Oral health and respiratory infection. J Can Dent Assoc. 2002; 68:340–345.29. Kluytmans JA, Wertheim HF. Nasal carriage of Staphylococcus aureus and prevention of nosocomial infections. Infection. 2005; 33:3–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Strategies to Reduce the Risk of Medical Malpractice Claims against Hospitalists
- Medico-Legal Consideration of Hemopneumothorax : Closing Claim Study
- Medical Malpractice Claims on Emergency Medical Facilities: Medicolegal Consideration Based on Judicial Precedents
- The Legal Doctrine on 'Limitation of Liability' in the Precedent Analysis on Plastic Surgery Medical Malpractice Lawsuits
- A Systematic Content Analysis of the Closed Nursing Malpractice Claims Related to Patients’ Safety