Perinatology.
2016 Sep;27(3):181-184. 10.14734/PN.2016.27.3.181.
Polyhydramnios as a Clue for the Diagnosis of Congenital Myotonic Dystrophy
- Affiliations
-
- 1Division of Neonatology, Department of Pediatrics, Gil Medical Center, Gachon University, Incheon, Korea. sondw@gilhospital.com
- 2Department of Obstetrics and Gynecology, Gil Medical Center, Gachon University, Incheon, Korea.
- KMID: 2355578
- DOI: http://doi.org/10.14734/PN.2016.27.3.181
Abstract
- In 40-50% of all polyhydramnios cases, no apparent cause can be identified and are classified as idiopathic. More than ten percent of babies with idiopathic polyhydramnios revealed certain anomalies after a course of clinical suffering. Congenital myotonic dystrophy (CMD) is one of them. Myotonic dystrophy is the most common form of neuromuscular disorder in adults. CMD is an autosomal dominantly inherited disease, inherited mostly from the mother. Severely affected CMD infants exhibit very critical respiratory failure, and the prognosis is unfavorable in up to 30% of cases. Polyhydramnios coexists with almost all CMD fetuses. A provisional diagnosis of CMD in a pregnancy complicated with polyhydramnios and maternal grip myotonia before birth may be helpful to the neonatology team for planning a thorough and prepared care for newborn patients. We report two cases to inform neonatologists as well as obstetricians that a provisional diagnosis of CMD can be made in a pregnancy complicated with polyhydramnios in a mother with grip myotonia or myotonic dystrophy.
MeSH Terms
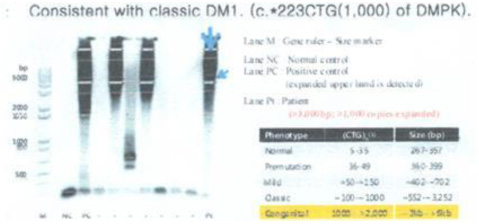
Figure
Reference
-
1. Boito S, Crovetto F, Ischia B, Crippa BL, Fabietti I, Bedeschi MF, et al. Prenatal ultrasound factors and genetic disorders in pregnancies complicated by polyhydramnios. Prenat Diagn. 2016; 36:726–730.
Article2. Magann EF, Chauhan SP, Doherty DA, Lutgendorf MA, Magann MI, Morrison JC. A review of idiopathic hydramnios and pregnancy outcomes. Obstet Gynecol Surv. 2007; 62:795–802.
Article3. Webb D, Muir I, Faulkner J, Johnson G. Myotonia dystrophica: obstetric complications. Am J Obstet Gynecol. 1978; 132:265–270.
Article4. Khan ZA, Khan SA. Myotonic dystrophy and pregnancy. J Pak Med Assoc. 2009; 59:717–719.5. Ashizawa T, Dubel JR, Dunne PW, Dunne CJ, Fu YH, Pizzuti A, et al. Anticipation in myotonic dystrophy. II. Complex relationships between clinical findings and structure of the GCT repeat. Neurology. 1992; 42:1877–1883.
Article6. Vanacore N, Rastelli E, Antonini G, Bianchi ML, Botta A, Bucci E, et al. An Age-Standardized Prevalence Estimate and a Sex and Age Distribution of Myotonic Dystrophy Types 1 and 2 in the Rome Province, Italy. Neuroepidemiology. 2016; 46:191–197.
Article7. Prendergast P, Magalhaes S, Campbell C. Congenital myotonic dystrophy in a national registry. Paediatr Child Health. 2010; 15:514–518.
Article8. Esplin MS, Hallam S, Farrington PF, Nelson L, Byrne J, Ward K. Myotonic dystrophy is a significant cause of idiopathic polyhydramnios. Am J Obstet Gynecol. 1998; 179:974–977.
Article9. Turner C, Hilton-Jones D. The myotonic dystrophies: diagnosis and management. J Neurol Neurosurg Psychiatry. 2010; 81:358–367.
Article10. Dufour P, Berard J, Vinatier D, Savary JB, Dubreucq S, Monnier JC, et al. Myotonic dystrophy and pregnancy. A report of two cases and a review of the literature. Eur J Obstet Gynecol Reprod Biol. 1997; 72:159–164.
Article11. Textbook of neonatal resuscitation. 7th ed. Elk Grove Village: American Academy of Pediatrics;2016.12. Vanier TM. Dystrophia myotonica in childhood. Br Med J. 1960; 2:1284–1288.
Article13. Hageman AT, Gabreels FJ, Liem KD, Renkawek K, Boon JM. Congenital myotonic dystrophy; a report on thirteen cases and a review of the literature. J Neurol Sci. 1993; 115:95–101.
Article14. Rudnik-Schoneborn S, Zerres K. Outcome in pregnancies complicated by myotonic dystrophy: a study of 31 patients and review of the literature. Eur J Obstet Gynecol Reprod Biol. 2004; 114:44–53.15. Geifman-Holtzman O, Fay K. Prenatal diagnosis of congenital myotonic dystrophy and counseling of the pregnant mother: case report and literature review. Am J Med Genet. 1998; 78:250–253.
Article16. Zaki M, Boyd PA, Impey L, Roberts A, Chamberlain P. Congenital myotonic dystrophy: prenatal ultrasound findings and pregnancy outcome. Ultrasound Obstet Gynecol. 2007; 29:284–288.
Article17. Mashiach R, Rimon E, Achiron R. Tent-shaped mouth as a presenting symptom of congenital myotonic dystrophy. Ultrasound Obstet Gynecol. 2002; 20:312–313.
Article18. Zeesman S, Carson N, Whelan DT. Paternal transmission of the congenital form of myotonic dystrophy type 1: a new case and review of the literature. Am J Med Genet. 2002; 107:222–226.
Article19. Richer LP, Shevell MI, Miller SP. Diagnostic profile of neonatal hypotonia: an 11-year study. Pediatr Neurol. 2001; 25:32–37.
Article20. Kim ES, Jung KE, Kim SD, Kim EK, Chae JH, Kim HS, et al. Diagnostic classification and clinical aspects of floppy infants in the neonatal and pediatric intensive care units. Korean J Pediatr. 2006; 49:1158–1166.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Recurrent Hydramnios in Association with Congenital Myotonic Dystrophy
- A Case of Congenital Myotonic Dystrophy
- A Floppy Baby with Congenital Myotonic Dystrophy Complicated with Huge Subgaleal Hematoma Occurring in Non-instrumental Vaginal Delivery
- A case of congenital myotonic dystrophy: Molecular diagnosis and clinical study
- Clinical characteristics of pregnancies complicated by congenital myotonic dystrophy