J Korean Orthop Assoc.
2016 Oct;51(5):357-364. 10.4055/jkoa.2016.51.5.357.
The Effect of Lumbar Spinal Stenosis on Results of Treatment in Peripheral Arterial Disease
- Affiliations
-
- 1Department of Orthopedic Surgery, Presbyterian Medical Center, Jeonju, Korea. docby@hanmali.net
- 2Department of General Surgery, Presbyterian Medical Center, Jeonju, Korea.
- KMID: 2355499
- DOI: http://doi.org/10.4055/jkoa.2016.51.5.357
Abstract
- PURPOSE
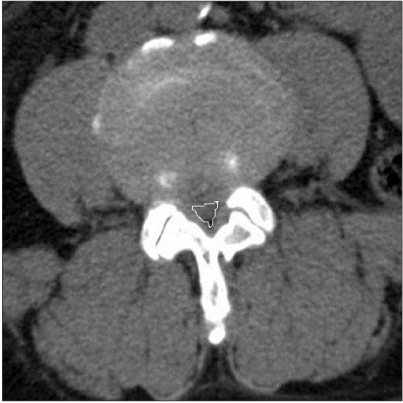
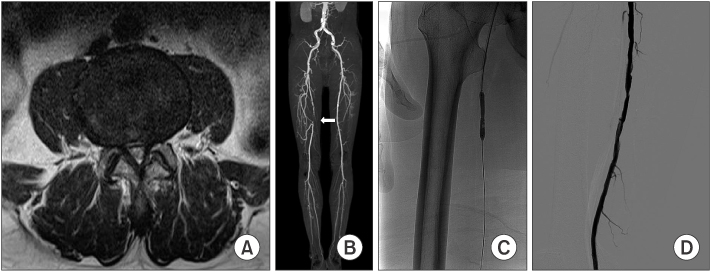
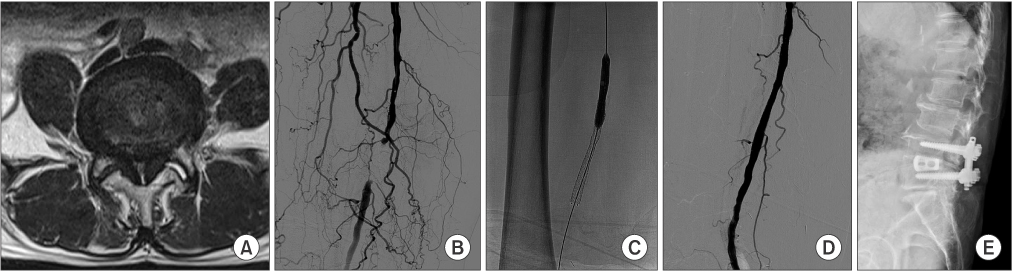
The purpose of this study was to evaluate the result of percutaneous transluminal angioplasty (PTA) in patients with concurrent lumbar spinal stenosis (LSS) and peripheral arterial disease (PAD).
MATERIALS AND METHODS
Patients who underwent PTA for intermittent claudication were evaluated retrospectively. Twenty-two patients with severe LSS were included in group A and 23 patients with no or mild LSS in group B. The symptomatic improvement after PTA was comparatively evaluated.
RESULTS
Visual analogue scale (VAS) and Walking Impairment Questionnaire (WIQ) scores showed significant improvement after PTA in both groups (p<0.001, <0.001). However, according to VAS, WIQ and modified MacNab scores, results of group A were less satisfactory (p<0.001, <0.001, p=0.03). Only 2 patients underwent additional spine surgery.
CONCLUSION
In results of PTA, the PAD associated LSS group showed less improvement than the PAD only group, but most patients showed symptomatic improvement with conservative treatment.
Keyword
MeSH Terms
Figure
Reference
-
1. Watters WC 3rd, Baisden J, Gilbert TJ, et al. North American Spine Society. Degenerative lumbar spinal stenosis: an evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis. Spine J. 2008; 8:305–310.
Article2. Dodge LD, Bohlman HH, Rhodes RS. Concurrent lumbar spinal stenosis and peripheral vascular disease. A report of nine patients. Clin Orthop Relat Res. 1988; (230):141–148.3. Uesugi K, Sekiguchi M, Kikuchi S, et al. Lumbar spinal stenosis associated with peripheral arterial disease: a prospective multicenter observational study. J Orthop Sci. 2012; 17:673–681.
Article4. Han MH, Lee DH, Park KS, et al. Risk factors and incidence for peripheral arterial disease in patients with typical lumbar spinal stenosis. Korean J Spine. 2014; 11:183–187.
Article5. Toribatake Y, Sawamura E, Kano N, Kitagawa K, Saito Y. The frequency and differential diagnosis of peripheral arterial occlusive disease in intermittent claudicants in orthopaedics. Orthop Surg Traumatol. 2002; 45:665–674.6. Konno S, Hayashino Y, Fukuhara S, et al. Development of a clinical diagnosis support tool to identify patients with lumbar spinal stenosis. Eur Spine J. 2007; 16:1951–1957.
Article7. Lee GY, Lee JW, Choi HS, Oh KJ, Kang HS. A new grading system of lumbar central canal stenosis on MRI: an easy and reliable method. Skeletal Radiol. 2011; 40:1033–1039.
Article8. Schonstrom NS, Bolender NF, Spengler DM. The pathomorphology of spinal stenosis as seen on CT scans of the lumbar spine. Spine (Phila Pa 1976). 1985; 10:806–811.
Article9. Regensteiner JG, Steiner JF, Panzer RJ, Hiatt WR. Evaluation of walking impairment by questionnaire in patients with peripheral arterial disease. J Vasc Med Biol. 1990; 2:142–152.10. Verbiest H. A radicular syndrome from developmental narrowing of the lumbar vertebral canal. J Bone Joint Surg Br. 1954; 36-B:230–237.
Article11. Hawkes CH, Roberts GM. Neurogenic and vascular claudication. J Neurol Sci. 1978; 38:337–345.
Article12. Ouriel K. Peripheral arterial disease. Lancet. 2001; 358:1257–1264.
Article13. Faglia E, Dalla Paola L, Clerici G, et al. Peripheral angioplasty as the first-choice revascularization procedure in diabetic patients with critical limb ischemia: prospective study of 993 consecutive patients hospitalized and followed between 1999 and 2003. Eur J Vasc Endovasc Surg. 2005; 29:620–627.
Article14. Park SW, Kim JS, Yun IJ, et al. Clinical outcomes of endovascular treatments for critical limb ischemia with chronic total occlusive lesions limited to below-the-knee arteries. Acta Radiol. 2013; 54:785–789.
Article15. Belli AM, Cumberland DC, Knox AM, Procter AE, Welsh CL. The complication rate of percutaneous peripheral balloon angioplasty. Clin Radiol. 1990; 41:380–383.
Article16. Minar E, Ahmadi A, Koppensteiner R, et al. Comparison of effects of high-dose and low-dose aspirin on restenosis after femoropopliteal percutaneous transluminal angioplasty. Circulation. 1995; 91:2167–2173.
Article17. Cabana F, Pointillart V, Vital J, Sénégas J. Postoperative compressive spinal epidural hematomas. 15 cases and a review of the literature. Rev Chir Orthop Reparatrice Appar Mot. 2000; 86:335–345.18. Scavarda D, Peruzzi P, Bazin A, et al. Postoperative spinal extradural hematomas. 14 cases. Neurochirurgie. 1997; 43:220–227.19. Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Associations for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (writing committee to develop guidelines for the management of patients with peripheral arterial disease): summary of recommendations. J Vasc Interv Radiol. 2006; 17:1383–1397.20. Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG;. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J Vasc Surg. 2007; 45:Suppl S. S5–S67.
Article21. Imagama S, Matsuyama Y, Sakai Y, et al. An arterial pulse examination is not sufficient for diagnosis of peripheral arterial disease in lumbar spinal canal stenosis: a prospective multicenter study. Spine (Phila Pa 1976). 2011; 36:1204–1210.22. Jeon CH, Han SH, Chung NS, Hyun HS. The validity of ankle-brachial index for the differential diagnosis of peripheral arterial disease and lumbar spinal stenosis in patients with atypical claudication. Eur Spine J. 2012; 21:1165–1170.
Article23. de Graaf I, Prak A, Bierma-Zeinstra S, Thomas S, Peul W, Koes B. Diagnosis of lumbar spinal stenosis: a systematic review of the accuracy of diagnostic tests. Spine (Phila Pa 1976). 2006; 31:1168–1176.24. Beattie PF, Meyers SP, Stratford P, Millard RW, Hollenberg GM. Associations between patient report of symptoms and anatomic impairment visible on lumbar magnetic resonance imaging. Spine (Phila Pa 1976). 2000; 25:819–828.
Article25. Wiesel SW, Tsourmas N, Feffer HL, Citrin CM, Patronas N. A study of computer-assisted tomography. I. The incidence of positive CAT scans in an asymptomatic group of patients. Spine (Phila Pa 1976). 1984; 9:549–551.26. Haig AJ, Tong HC, Yamakawa KS, et al. The sensitivity and specificity of electrodiagnostic testing for the clinical syndrome of lumbar spinal stenosis. Spine (Phila Pa 1976). 2005; 30:2667–2676.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Characteristics and Rehabilitative Therapeutic Effect on Peripheral Arterial Disease Combined with Lumbar Spinal Stenosis
- A Case of Coexisting Cervical and Lumbar Spinal Stenosis
- Prevalence and Risk Factors of Peripheral Arterial Disease in Patients with Lumbar Spinal Stenosis and Intermittent Claudication: CT Angiography Study
- A case of William's syndrome associated peripheral pulmonary arterial stenosis
- Y-Angle Stenosis of Lumbar Spine: New Concept of Lumbar Stenosis