Korean Circ J.
2016 Nov;46(6):798-803. 10.4070/kcj.2016.46.6.798.
Is SYNTAX Score Predictive of Atrial Fibrillation after On-Pump Coronary Artery Bypass Graft Surgery?
- Affiliations
-
- 1Department of Cardiology, Near East University, Nicosia, Cyprus. drcerit@hotmail.com
- 2Department of Cardiovascular Surgery, Near East University, Nicosia, Cyprus.
- 3Department of Biostatistics, Near East University, Nicosia, Cyprus.
- 4Department of Cardiology, Afyon State Hospital, Afyon, Turkey.
- KMID: 2355455
- DOI: http://doi.org/10.4070/kcj.2016.46.6.798
Abstract
- BACKGROUND AND OBJECTIVES
The relationship of synergy between percutaneous coronary intervention with taxus and cardiac surgery (SYNTAX) score and development of atrial fibrillation (AF) after coronary artery bypass surgery (CABG) has not been studied. Therefore, we assessed the relationship between the SYNTAX score and development of AF after CABG (POAF).
SUBJECTS AND METHODS
The medical records of consecutive patients, who underwent CABG surgery from January 2013 to September 2015, were retrospectively reviewed for the development of AF in the postoperative period. SYNTAX score, clinical and echocardiographic parameters were evaluated. The independent variables for the development of POAF were defined and their predictive values were measured.
RESULTS
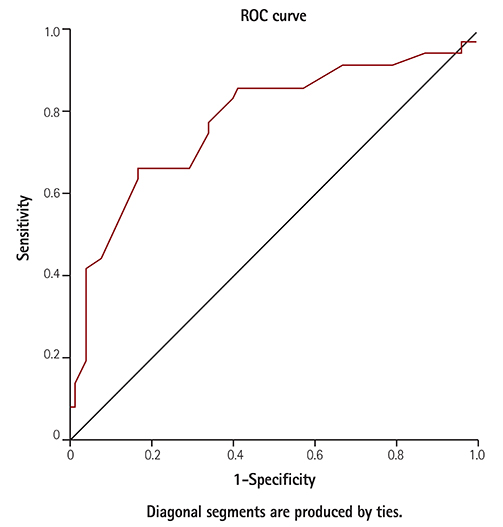
The study group consisted of 106 patients, of which 36 (34%) developed POAF. Age, hypertension, stroke, chronic obstructive pulmonary disease (COPD), heart failure (HF), diabetes mellitus (DM), left atrial diameter, neutrophil/lymphocyte ratio, platelet large cell ratio, creatinine, blood urea nitrogen and SYNTAX score were identified as important variables for the development of POAF. However, in logistic regression analysis COPD (OR=19.313, 95% CI=2.416-154.407, p=0.005), HF (OR=28.362, 95% CI=2.034-395.515, p=0.013), SYNTAX score (OR=0.863, 95% CI=0.757-0.983, p=0.026), and DM (OR=20.770, 95% CI=3.791-113.799, p<0.001) appeared as independent variables predicting the development of POAF. In receiver operation characteristic analysis, SYNTAX score (≥22.25) (AUC=0.777, 95% CI=0.676-0.877, p<0.001) was one of the strongest predictors for the development of POAF.
CONCLUSION
The SYNTAX score level was independently associated with the development of AF after CABG.
MeSH Terms
-
Atrial Fibrillation*
Blood Platelets
Blood Urea Nitrogen
Coronary Artery Bypass*
Coronary Artery Disease
Coronary Vessels*
Creatinine
Diabetes Mellitus
Echocardiography
Heart Failure
Humans
Hypertension
Logistic Models
Medical Records
Percutaneous Coronary Intervention
Postoperative Period
Pulmonary Disease, Chronic Obstructive
Retrospective Studies
Stroke
Taxus
Thoracic Surgery
Creatinine
Figure
Reference
-
1. Blommaert D, Gonzalez M, Mucumbitsi J, et al. Effective prevention of atrial fibrillation by continuous atrial overdrive pacing after coronary artery bypass surgery. J Am Coll Cardiol. 2000; 35:1411–1415.2. Amar D, Shi W, Hogue CW Jr, et al. Clinical prediction rule for atrial fibrillation after coronary artery bypass grafting. J Am Coll Cardiol. 2004; 44:1248–1253.3. American heart association heart disease and stroke statistics update at-A-glance. Circulation. 2007; 115:e69–e171.4. Lip GY, Beevers DG. ABC of atrial fibrillation. History, epidemiology, and importance of atrial fibrillation. BMJ. 1995; 311:1361–1363.5. Kralev S, Schneider K, Lang S, Süselbeck T, Borggrefe M. Incidence and severity of coronary artery disease in patients with atrial fibrillation undergoing first-time coronary angiography. PLoS One. 2011; 6:e24964.6. Van Gelder IC, Groenveld HF, Crijns HJ, et al. Race II Investigators. Lenient versus strict rate control in patients with atrial fibrillation. N Engl J Med. 2010; 362:1363–1373.7. Crijns HJ, Van Gelder IC, Van Gilst WH, Hillege H, Gosselink AM, Lie KI. Serial antiarrhythmic drug treatment to maintain sinus rhythm after electrical cardioversion for chronic atrial fibrillation or atrial flutter. Am J Cardiol. 1991; 68:335–341.8. AFFIRM Investigators. Atrial Fibrillation Follow-up Investigation of Rhythm Management. Baseline characteristics of patients with atrial fibrillation: the AFFIRM study. Am Heart J. 2002; 143:991–1001.9. Sianos G, Morel MA, Kappetein AP, et al. The SYNTAX score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention. 2005; 1:219–227.10. Aksakal E, Tanboğa IH, Kurt M. Predictors of coronary lesions complexity in patients with stable coronary artery disease. Angiology. 2013; 64:304–309.11. Ucar H, Gur M, Borekci A, et al. Relationship between extent and complexity of coronary artery disease and different left ventricular geometric patterns in patients with coronary artery disease and hypertension. Anatol J Cardiol. 2015; 15:789–794.12. Benjamin EJ, Wolf PA, D'Agostino RB, Silbershatz H, Kannel WB, Levy D. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation. 1998; 98:946–952.13. Banach M, Rysz J, Drozdz JA, et al. Risk factors of atrial fibrillation following coronary artery bypass grafting: a preliminary report. Circ J. 2006; 70:438–441.14. Sidney S, Sorel M, Quesenberry CP Jr, DeLuise C, Lanes S, Eisner MD. COPD and incident cardiovascular disease hospitalizations and mortality: Kaiser Permanente Medical Care Program. Chest. 2005; 128:2068–2075.15. Caglar IM, Dasli T, Turhan Caglar FN, Teber MK, Ugurlucan M, Ozmen G. Evaluation of atrial conduction features with tissue Doppler imaging in patients with chronic obstructive pulmonary disease. Clin Res Cardiol. 2012; 101:599–606.16. Benjamin EJ, Levy D, Vaziri SM, D'Agostino RB, Belanger AJ, Wolf PA. Independent risk factors for atrial fibrillation in a population-based cohort: The Framingham heart study. JAMA. 1994; 271:840–844.17. Middlekauff HR, Stevenson WG, Stevenson LW. Prognostic significance of atrial fibrillation in advanced heart failure: A study of 390 patients. Circulation. 1991; 84:40–48.18. Huxley RR, Filion KB, Konety S, Alonso A. Meta-analysis of cohort and case-control studies of type 2 diabetes mellitus and risk of atrial fibrillation. Am J Cardiol. 2011; 108:56–62.19. Schoen T, Pradhan AD, Albert CM, Conen D. Type 2 diabetes mellitus and risk of incident atrial fibrillation in women. J Am Coll Cardiol. 2012; 60:1421–1428.20. Rechciński T, Jasińska A, Foryś J, et al. Prognostic value of platelet indices after acute myocardial infarction treated with primary percutaneous coronary intervention. Cardiol J. 2013; 20:491–498.21. Shao Q, Chen K, Rha SW, Lim HE, Li G, Liu T. Usefulness of Neutrophil/Lymphocyte Ratio as a Predictor of Atrial Fibrillation: A Meta-analysis. Arch Med Res. 2015; 46:199–206.22. Kwon CH, Kim J, Kim MS, et al. Impact of Impaired Renal Function on the Incidence of Atrial Fibrillation following Radiofrequency Ablation of Cavotricuspid Isthmus-Dependent Atrial Flutter. Korean Circ J. 2015; 45:473–478.23. Valgimigli M, Serruys PW, Tsuchida K, et al. Cyphering the complexity of coronary artery disease using the SYNTAX score to predict clinical outcome in patients with three-vessel lumen obstruction undergoing percutaneous coronary intervention. Am J Cardiol. 2007; 99:1072–1081.24. Fukui T, Uchimuro T, Takanashi S. EuroSCORE II with SYNTAX score to assess risks of coronary artery bypass grafting outcomes. Eur J Cardiothorac Surg. 2015; 47:66–71.25. Møller CH, Penninga L, Wetterslev J, Steinbrüchel DA, Gluud C. Off-pump versus on-pump coronary artery bypass grafting for ischaemic heart disease. Cochrane Database Syst Rev. 2012; (3):CD007224.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Risk Factors of Atrial Fibrillation after Coronary Artery Bypass Grafting
- Use of Preoperative Transthoracic Echocardiography to Predict the Prognosis after Off-Pump Coronary Artery Bypass Grafting
- Air embolism during off-pump coronary artery bypass graft surgery: A case report
- Intra-aortic Balloon Pump Therapy for Hemodynamic Instability during Off-pump Coronary Artery Bypass Surgery
- Wrapping of an Ascending Aortic Aneurysm with the Multiple Boot-Straps Technique in a Patient Undergoing Off-Pump Coronary Artery Bypass Grafting