J Korean Fract Soc.
2016 Oct;29(4):265-269. 10.12671/jkfs.2016.29.4.265.
Percutaneous Drainage and Sclerotherapy for Delayed Lumbar Morel-Lavalee Lesion: Two Case Reports
- Affiliations
-
- 1Department of Plastic Surgery, Hanil General Hospital, Seoul, Korea.
- 2Department of Orthopedic Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 3Department of Plastic and Reconstructive Surgery, School of Medicine, Kangwon National University, Chuncheon, Korea. ps@kangwon.ac.kr
- KMID: 2355432
- DOI: http://doi.org/10.12671/jkfs.2016.29.4.265
Abstract
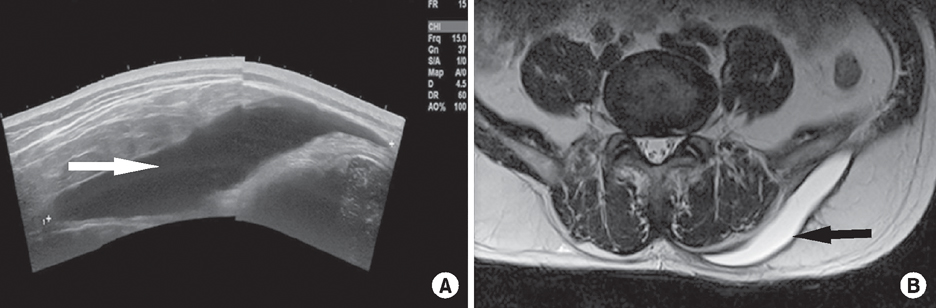
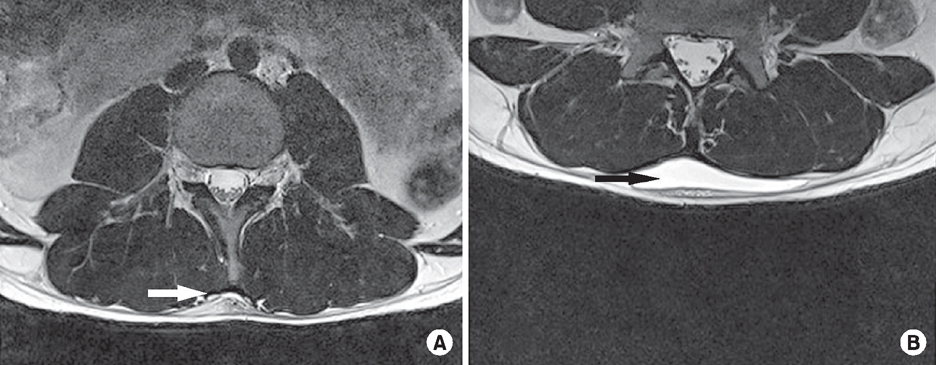
- Closed internal degloving is a significant soft-tissue injury associated with a trauma that results in a tear of the subcutaneous tissue away from the underlying fascia. Although the diagnosis of Morel-Lavallee lesion (MLL) is routinely based on clinical and radiological examinations, in one-third of the cases, there is a possibility that clinicians may fail to diagnose MLL due to its inconsistent clinical manifestations. Additionally, it often involves initial skin bruising due to underlying soft-tissue injury. We present two cases of delayed MLL without a fracture treated using percutaneous drainage and sclerotherapy. Our cases demonstrated successful treatment with a minimally invasive percutaneous approach. The potential advantage of using a percutaneous technique is to preserve the subdermal arterial plexus, which is the only remaining blood supply to the skin in the area of the lesion. Maintaining this blood supply may result in healthier skin at the time of any open procedure.
Keyword
Figure
Reference
-
1. Hak DJ, Olson SA, Matta JM. Diagnosis and management of closed internal degloving injuries associated with pelvic and acetabular fractures: the Morel-Lavallee lesion. J Trauma. 1997; 42:1046–1051.
Article2. Shen C, Peng JP, Chen XD. Efficacy of treatment in peri-pelvic Morel-Lavallee lesion: a systematic review of the literature. Arch Orthop Trauma Surg. 2013; 133:635–640.
Article3. Kottmeier SA, Wilson SC, Born CT, Hanks GA, Iannacone WM, DeLong WG. Surgical management of soft tissue lesions associated with pelvic ring injury. Clin Orthop Relat Res. 1996; (329):46–53.
Article4. Hudson DA, Knottenbelt JD, Krige JE. Closed degloving injuries: results following conservative surgery. Plast Reconstr Surg. 1992; 89:853–855.5. Mukherjee K, Perrin SM, Hughes PM. Morel-Lavallee lesion in an adolescent with ultrasound and MRI correlation. Skeletal Radiol. 2007; 36:Suppl 1. S43–S45.
Article6. Letts RM. Degloving injuries in children. J Pediatr Orthop. 1986; 6:193–197.
Article7. Moran DE, Napier NA, Kavanagh EC. Lumbar Morel-Lavallée effusion. Spine J. 2012; 12:1165–1166.
Article8. Tseng S, Tornetta P 3rd. Percutaneous management of Morel-Lavallee lesions. J Bone Joint Surg Am. 2006; 88:92–96.
Article9. Bansal A, Bhatia N, Singh A, Singh AK. Doxycycline sclerodesis as a treatment option for persistent Morel-Lavallée lesions. Injury. 2013; 44:66–69.
Article10. Anakwenze OA, Trivedi V, Goodman AM, Ganley TJ. Concealed degloving injury (the Morel-Lavallée lesion) in childhood sports: a case report. J Bone Joint Surg Am. 2011; 93:e148.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sclerotherapy Using Abnobaviscum for the Extensive Recurrent Chronic Morel-Lavallée Lesions - A Case Report -
- Limited Incisional Drainage and Negative-Pressure Wound Therapy in an Acute Morel-Lavallée Lesion
- Extensive Multiple Morel-Lavallée Lesions: A Case Report
- Morel-Lavallee Lesion: A Case Report
- Rare complication of skin necrosis after endoscopic debridement and cutaneo-fascial suture for a massive Morel-Lavallée lesion in Korea: a case report