Quality of care in inflammatory bowel disease in Asia: the results of a multinational web-based survey in the 2nd Asian Organization of Crohn's and Colitis (AOCC) meeting in Seoul
- Affiliations
-
- 1Department of Internal Medicine, Ewha University College of Medicine, Seoul, Korea.
- 2Department of Internal Medicine, St. Vincent's Hospital, The Catholic University College of Medicine, Seoul, Korea. drmaloman@catholic.ac.kr
- 3Department of Internal Medicine, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 4Department of Internal Medicine, Guri Hospital, Hanyang University College of Medicine, Guri, Korea.
- 5Department of Internal Medicine, Ulsan University College of Medicine, Seoul, Korea.
- KMID: 2354966
- DOI: http://doi.org/10.5217/ir.2016.14.3.240
Abstract
- BACKGROUND/AIMS
The quality of care in inflammatory bowel disease (IBD) has not been systematically estimated. The aim of this study was to investigate the current status of quality of IBD care in Asian countries.
METHODS
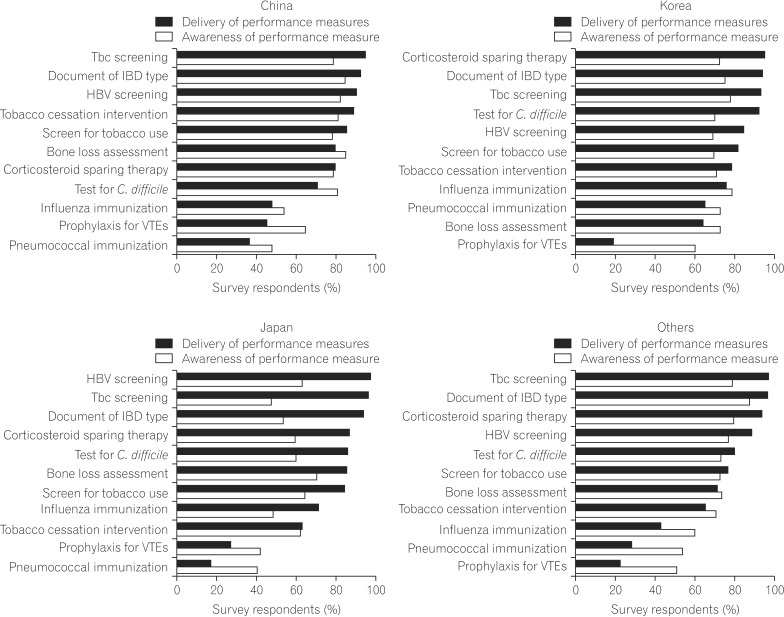
A questionnaire-based survey was conducted between March 2014 and May 2014. The questionnaire was adopted from "An adult inflammatory bowel disease physician performance measure set" developed by the American Gastroenterological Association. If the respondent executed the performance measure in more than 70% of patients, the measure was regarded as well performed.
RESULTS
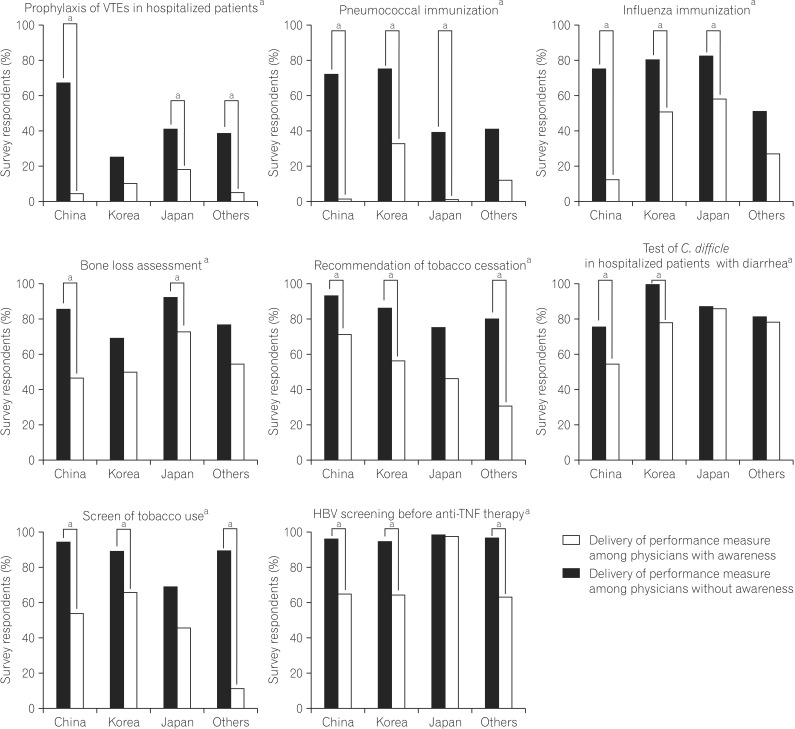
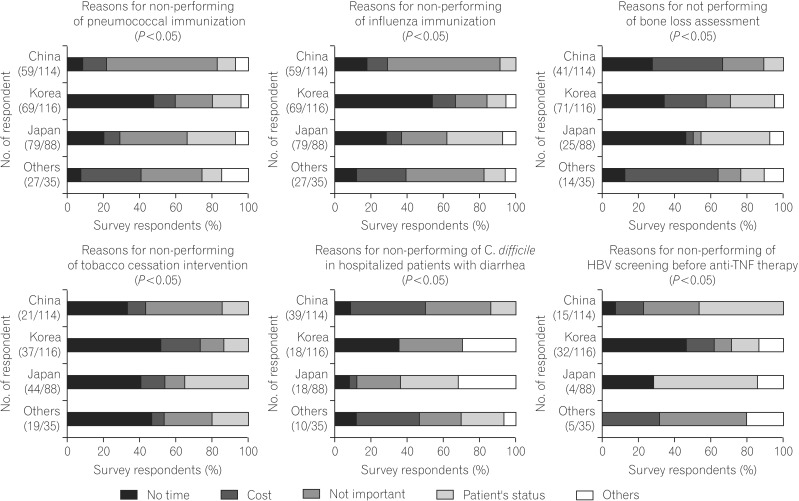
A total of 353 medical doctors from Asia completed the survey (116 from Korea, 114 from China, 88 from Japan, 17 from Taiwan, 8 from Hong-Kong, 4 from India, 3 from Singapore, and 1 each from the Philippines, Malaysia and Indonesia). The delivery of performance measures, however, varied among countries. The documentation of IBD and tuberculosis screening before anti-tumor necrosis factor therapy were consistently performed well, while pneumococcal immunization and prophylaxis of venous thromboembolisms in hospitalized patients were performed less frequently in all countries. Physician awareness was positively associated with the delivery of performance measures. Variations were also noted in reasons for non-performance or low performance of quality measures, and the two primary reasons cited were consideration of the measure to be unimportant and lack of time.
CONCLUSIONS
The delivery of performance measures varies among physicians in Asian countries, and reflects variations in the quality of care among the countries. This variation should be recognized to improve the quality of care in Asian countries.
MeSH Terms
Figure
Cited by 9 articles
-
Incidence and risk factors for venous thrombosis among patients with inflammatory bowel disease in China: a multicenter retrospective study
Jing Liu, Xiang Gao, Ye Chen, Qiao Mei, Liangru Zhu, Jiaming Qian, Pinjin Hu, Qian Cao
Intest Res. 2021;19(3):313-322. doi: 10.5217/ir.2020.00017.Improving the quality of care for inflammatory bowel disease
Byong Duk Ye, Simon Travis
Intest Res. 2019;17(1):45-53. doi: 10.5217/ir.2018.00113.Quality indicators in inflammatory bowel disease
Sameer K. Berry, Gil Y. Melmed
Intest Res. 2018;16(1):43-47. doi: 10.5217/ir.2018.16.1.43.Asian Organization for Crohn's and Colitis and Asia Pacific Association of Gastroenterology consensus on tuberculosis infection in patients with inflammatory bowel disease receiving anti-tumor necrosis factor treatment. Part 1: risk assessment
Dong Il Park, Tadakazu Hisamatsu, Minhu Chen, Siew Chien Ng, Choon Jin Ooi, Shu Chen Wei, Rupa Banerjee, Ida Normiha Hilmi, Yoon Tae Jeen, Dong Soo Han, Hyo Jong Kim, Zhihua Ran, Kaichun Wu, Jiaming Qian, Pin-Jin Hu, Katsuyoshi Matsuoka, Akira Andoh, Yasuo Suzuki, Kentaro Sugano, Mamoru Watanabe, Toshifumi Hibi, Amarender S. Puri, Suk-Kyun Yang
Intest Res. 2018;16(1):4-16. doi: 10.5217/ir.2018.16.1.4.Should Asian inflammatory bowel disease patients need routine thromboprophylaxis?
Meng-Tzu Weng, Chien-Chih Tung, Jau-Min Wong, Shu-Chen Wei
Intest Res. 2018;16(2):312-314. doi: 10.5217/ir.2018.16.2.312.IBD2020 global forum: results of an international patient survey on quality of care
Peter Irving, Johan Burisch, Richard Driscoll, Mats Olsson, John R Fullarton, Barry S Rodgers-Gray, Simon PL Travis
Intest Res. 2018;16(4):537-545. doi: 10.5217/ir.2018.00041.Results of the first survey for the current status of inflammatory bowel disease management in Asian countries
Ji Won Kim
Intest Res. 2016;14(3):199-201. doi: 10.5217/ir.2016.14.3.199.Infectious complications in patients with inflammatory bowel disease in Asia: the results of a multinational web-based survey in the 8th Asian Organization for Crohn’s and Colitis meeting
Yu Kyung Jun, Seong-Joon Koh, Dae Seong Myung, Sang Hyoung Park, Choon Jin Ooi, Ajit Sood, Jong Pil Im
Intest Res. 2023;21(3):353-362. doi: 10.5217/ir.2023.00013.Treatment of inflammatory bowel disease–Asian perspectives: the results of a multinational web-based survey in the 8th Asian Organization for Crohn’s and Colitis meeting
Eun Mi Song, Soo-Young Na, Sung Noh Hong, Siew Chien Ng, Tadakazu Hisamatsu, Byong Duk Ye
Intest Res. 2023;21(3):339-352. doi: 10.5217/ir.2022.00135.
Reference
-
1. Kappelman MD, Rifas-Shiman SL, Porter CQ, et al. Direct health care costs of Crohn’s disease and ulcerative colitis in US children and adults. Gastroenterology. 2008; 135:1907–1913. PMID: 18854185.
Article2. Longobardi T, Jacobs P, Bernstein CN. Utilization of health care resources by individuals with inflammatory bowel disease in the United States: a profile of time since diagnosis. Am J Gastroenterol. 2004; 99:650–655. PMID: 15089897.
Article3. Bodger K. Cost effectiveness of treatments for inflammatory bowel disease. Pharmacoeconomics. 2011; 29:387–401. PMID: 21271748.
Article4. David G, Gunnarsson C, Lofland JH. Variations in care: a retrospective database analysis of healthcare utilization patterns for patients with inflammatory bowel disease. J Med Econ. 2015; 18:137–144. PMID: 25335098.
Article5. Kappelman MD, Palmer L, Boyle BM, Rubin DT. Quality of care in inflammatory bowel disease: a review and discussion. Inflamm Bowel Dis. 2010; 16:125–133. PMID: 19572335.
Article6. Crandall WV, Boyle BM, Colletti RB, Margolis PA, Kappelman MD. Development of process and outcome measures for improvement: lessons learned in a quality improvement collaborative for pediatric inflammatory bowel disease. Inflamm Bowel Dis. 2011; 17:2184–2191. PMID: 21456033.
Article7. Melmed GY, Siegel CA. Quality improvement in inflammatory bowel disease. Gastroenterol Hepatol (N Y). 2013; 9:286–292. PMID: 23943663.8. Molodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012; 142:46–54. PMID: 22001864.
Article9. Prideaux L, Kamm MA, De Cruz PP, Chan FK, Ng SC. Inflammatory bowel disease in Asia: a systematic review. J Gastroenterol Hepatol. 2012; 27:1266–1280. PMID: 22497584.
Article10. Ahuja V, Tandon RK. Inflammatory bowel disease in the Asia-Pacific area: a comparison with developed countries and regional differences. J Dig Dis. 2010; 11:134–147. PMID: 20579217.
Article11. Feuerstein JD, Lewandowski JJ, Martinez-Vazquez M, Leffler DA, Cheifetz AS. Documented compliance with inflammatory bowel disease quality measures is poor. Dig Dis Sci. 2015; 60:339–344. PMID: 25311583.
Article12. Stille CJ, Jerant A, Bell D, Meltzer D, Elmore JG. Coordinating care across diseases, settings, and clinicians: a key role for the generalist in practice. Ann Intern Med. 2005; 142:700–708. PMID: 15838089.
Article13. Tinsley A, Naymagon S, Trindade AJ, Sachar DB, Sands BE, Ullman TA. A survey of current practice of venous thromboembolism prophylaxis in hospitalized inflammatory bowel disease patients in the United States. J Clin Gastroenterol. 2013; 47:e1–e6. PMID: 22476043.
Article14. Wasan SK, Calderwood AH, Long MD, Kappelman MD, Sandler RS, Farraye FA. Immunization rates and vaccine beliefs among patients with inflammatory bowel disease: an opportunity for improvement. Inflamm Bowel Dis. 2014; 20:246–250. PMID: 24374881.
Article15. Walsh AJ, Weltman M, Burger D, et al. Implementing guidelines on the prevention of opportunistic infections in inflammatory bowel disease. J Crohns Colitis. 2013; 7:e449–e456. PMID: 23601754.
Article16. Sam JJ, Bernstein CN, Razik R, Thanabalan R, Nguyen GC. Physicians’ perceptions of risks and practices in venous thromboembolism prophylaxis in inflammatory bowel disease. Dig Dis Sci. 2013; 58:46–52. PMID: 23053902.
Article17. Yeo DX, Junnarkar S, Balasubramaniam S, et al. Incidence of venous thromboembolism and its pharmacological prophylaxis in Asian general surgery patients: a systematic review. World J Surg. 2015; 39:150–157. PMID: 25189450.
Article18. Sonoda K, Ikeda S, Mizuta Y, Miyahara Y, Kohno S. Evaluation of venous thromboembolism and coagulation-fibrinolysis markers in Japanese patients with inflammatory bowel disease. J Gastroenterol. 2004; 39:948–954. PMID: 15549447.
Article19. Choudhry NK, Fletcher RH, Soumerai SB. Systematic review: the relationship between clinical experience and quality of health care. Ann Intern Med. 2005; 142:260–273. PMID: 15710959.
Article20. Yeung JH, Goodman KJ, Fedorak RN. Inadequate knowledge of immunization guidelines: a missed opportunity for preventing infection in immunocompromised IBD patients. Inflamm Bowel Dis. 2012; 18:34–40. PMID: 21337671.
Article21. Wagnon JH, Leiman DA, Ayers GD, Schwartz DA. Survey of gastroenterologists’ awareness and implementation of AGA guidelines on osteoporosis in inflammatory bowel disease patients: are the guidelines being used and what are the barriers to their use? Inflamm Bowel Dis. 2009; 15:1082–1089. PMID: 19137605.
Article22. Jung YS, Park JH, Kim HJ, et al. Insufficient knowledge of korean gastroenterologists regarding the vaccination of patients with inflammatory bowel disease. Gut Liver. 2014; 8:242–247. PMID: 24827619.
Article23. Gupta V, Dawood FS, Muangchana C, et al. Influenza vaccination guidelines and vaccine sales in southeast Asia: 2008-2011. PLoS One. 2012; 7:e52842. PMID: 23285200.
Article24. Mithal A, Kaur P. Osteoporosis in Asia: a call to action. Curr Osteoporos Rep. 2012; 10:245–247. PMID: 22898971.
Article25. Wasan SK, Coukos JA, Farraye FA. Vaccinating the inflammatory bowel disease patient: deficiencies in gastroenterologists knowledge. Inflamm Bowel Dis. 2011; 17:2536–2540. PMID: 21538710.
Article26. Hung IF, Tantawichien T, Tsai YH, Patil S, Zotomayor R. Regional epidemiology of invasive pneumococcal disease in Asian adults: epidemiology, disease burden, serotype distribution, and antimicrobial resistance patterns and prevention. Int J Infect Dis. 2013; 17:e364–e373. PMID: 23416209.
Article27. Mangtani P, Shah A, Roberts JA. Validation of influenza and pneumococcal vaccine status in adults based on self-report. Epidemiol Infect. 2007; 135:139–143. PMID: 16740194.
Article28. Yang J, Morris MR, Teevan J, Adamic LA, Ackerman MS. Culture matters: a survey study of social Q&A behavior. ICWSM. 2011; 11:409–416.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of inflammatory bowel disease in Asia: the results of a multinational web-based survey in the 2nd Asian Organization of Crohn's and Colitis (AOCC) meeting in Seoul
- Diagnosis of inflammatory bowel disease in Asia: the results of a multinational web-based survey in the 2nd Asian Organization for Crohn's and Colitis (AOCC) meeting in Seoul
- Diagnosis of inflammatory bowel disease–Asian perspectives: the results of a multinational web-based survey in the 8th Asian Organization for Crohn’s and Colitis meeting
- Erratum: Treatment of inflammatory bowel disease in Asia: the results of a multinational web-based survey in the 2(nd) Asian Organization for Crohn's and Colitis (AOCC) meeting in Seoul
- Treatment of inflammatory bowel disease–Asian perspectives: the results of a multinational web-based survey in the 8th Asian Organization for Crohn’s and Colitis meeting