Investig Magn Reson Imaging.
2016 Sep;20(3):185-190. 10.13104/imri.2016.20.3.185.
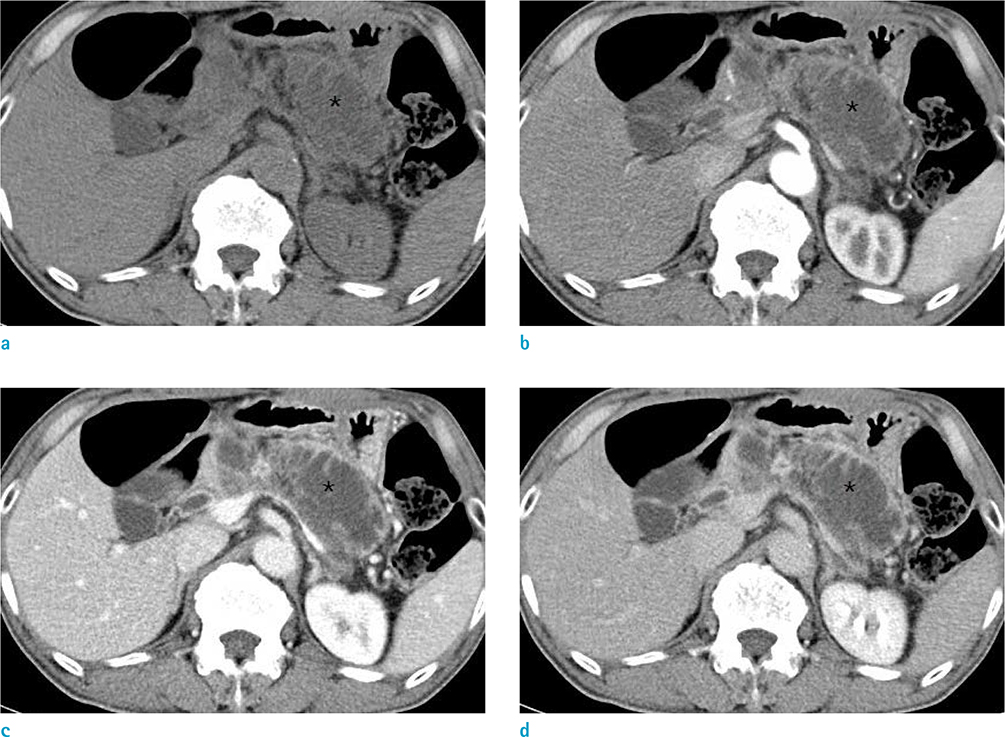
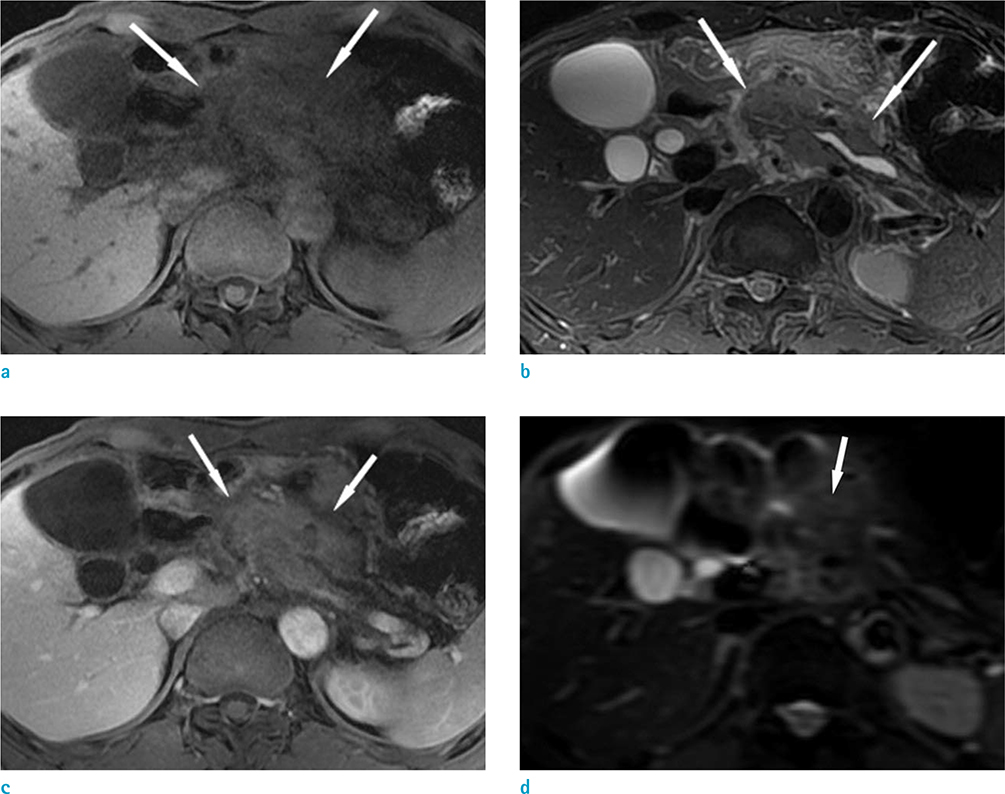
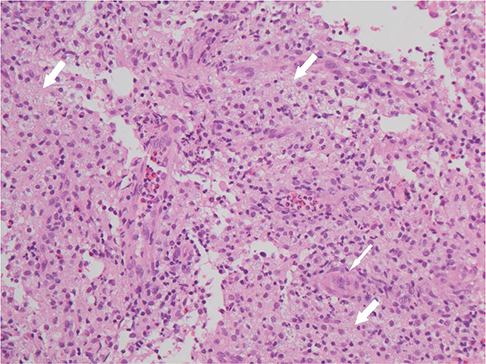
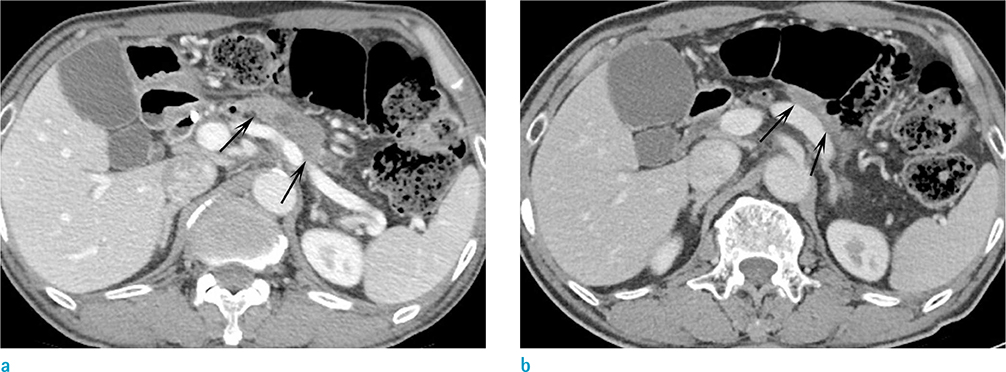
Xanthogranulomatous Pancreatitis Mimicking a Pancreatic Cancer on CT and MRI: a Case Report and Literature Review
- Affiliations
-
- 1Department of Radiology, Kyungpook National University Hospital, Kyungpook National University, School of Medicine, Daegu, Korea.
- 2Department of Radiology, Kyungpook National University Medical Center, Kyungpook National University School of Medicine, Daegu, Korea. shcho2405@gmail.com
- 3Department of Pathology, Kyungpook National University Medical Center, Kyungpook National University School of Medicine, Daegu, Korea.
- 4Department of Internal Medicine, Kyungpook National University Medical Center, Kyungpook National University School of Medicine, Daegu, Korea.
- KMID: 2354800
- DOI: http://doi.org/10.13104/imri.2016.20.3.185
Abstract
- Xanthogranulomatous inflammation is a rare benign condition involving various organs. However, its pancreas involvement is very rare. To the best of our knowledge, only 17 cases have been described in the literature. Interestingly, all reported 17 cases due to various causes underwent surgical resection. Here, we present a case of xanthogranulomatous pancreatitis in a 63-year-old man. He presented with epigastric pain and solid mass mimicking ductal adenocarcinoma in the body and tail of pancreas on magnetic resonance imaging. The patient was diagnosed as xanthogranulomatous pancreatitis via endoscopic ultrasound-guided fine needle aspiration. After that, he was followed up and monitored without any surgical treatment. Here, we show imaging findings and serial image changes of xanthogranulomatous pancreatitis for this case.
Keyword
MeSH Terms
Figure
Reference
-
1. Kim HS, Joo M, Chang SH, et al. Xanthogranulomatous pancreatitis presents as a solid tumor mass: a case report. J Korean Med Sci. 2011; 26:583–586.2. Houston JP, Collins MC, Cameron I, Reed MW, Parsons MA, Roberts KM. Xanthogranulomatous cholecystitis. Br J Surg. 1994; 81:1030–1032.3. Ueno T, Hamanaka Y, Nishihara K, et al. Xanthogranulomatous change appearing in the pancreas cyst wall. Pancreas. 1993; 8:649–651.4. Kamitani T, Nishimiya M, Takahashi N, Shida Y, Hasuo K, Koizuka H. Xanthogranulomatous pancreatitis associated with intraductal papillary mucinous tumor. AJR Am J Roentgenol. 2005; 185:704–707.5. Iyer VK, Aggarwal S, Mathur M. Xanthogranulomatous pancreatitis: mass lesion of the pancreas simulating pancreatic carcinoma--a report of two cases. Indian J Pathol Microbiol. 2004; 47:36–38.6. Kim YN, Park SY, Kim YK, Moon WS. Xanthogranulomatous pancreatitis combined with intraductal papillary mucinous carcinoma in situ. J Korean Med Sci. 2010; 25:1814–1817.7. Okabayashi T, Nishimori I, Kobayashi M, et al. Xanthogranulomatous pancreatic abscess secondary to acute pancreatitis: two case reports. Hepatogastroenterology. 2007; 54:1648–1651.8. Shima Y, Saisaka Y, Furukita Y, et al. Resected xanthogranulomatous pancreatitis. J Hepatobiliary Pancreat Surg. 2008; 15:240–242.9. Uguz A, Yakan S, Gurcu B, Yilmaz F, Ilter T, Coker A. Xanthogranulomatous pancreatitis treated by duodenum-preserving pancreatic head resection. Hepatobiliary Pancreat Dis Int. 2010; 9:216–218.10. Ikeura T, Takaoka M, Shimatani M, et al. Xanthogranulomatous inflammation of the peripancreatic region mimicking pancreatic cystic neoplasm. Intern Med. 2009; 48:1881–1884.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Xanthogranulomatous pancreatitis mimicking potentially malignant pancreatic neoplasm: report of a case
- Xanthogranulomatous Pancreatitis Mimicking Pancreatic Cancer
- Focal type autoimmune pancreatitis mimicking pancreatic cancer
- A Case of Pancreatic Head Carcinoma Mimicking Chronic Pancreatitis
- A case of lymphoplasmacytic sclerosing pancreatitis presenting as an obstructive jaundice