Hip Pelvis.
2016 Sep;28(3):148-156. 10.5371/hp.2016.28.3.148.
Adjuvant Teriparatide Therapy for Surgical Treatment of Femoral Fractures; Does It Work?
- Affiliations
-
- 1Department of Orthopaedic Surgery, Seoul National University College of Medicine, Seoul, Korea. jjyos@snu.ac.kr
- 2Seoul National University Medical Research Center, Seoul, Korea.
- KMID: 2354546
- DOI: http://doi.org/10.5371/hp.2016.28.3.148
Abstract
- PURPOSE
Atypical femoral fracture (AFF), periprosthetic femoral fracture (PPFF) and femoral nonunion (FNU) are recalcitrant challenges for orthopedic surgeons. Teriparatide (TPTD) had been demonstrated to have anabolic effects on bone in various studies. We postulated that adjuvant TPTD after operation would enhance biologic stimulation for bone formation. We investigated (1) whether the adjuvant TPTD could achieve satisfactory union rate of surgically challenging cases such as displaced AFF, PPFF and FNU; (2) whether the adjuvant TPTD could promote development of abundant callus after surgical fixation; (3) whether the adjuvant TPTD had medically serious adverse effects.
MATERIALS AND METHODS
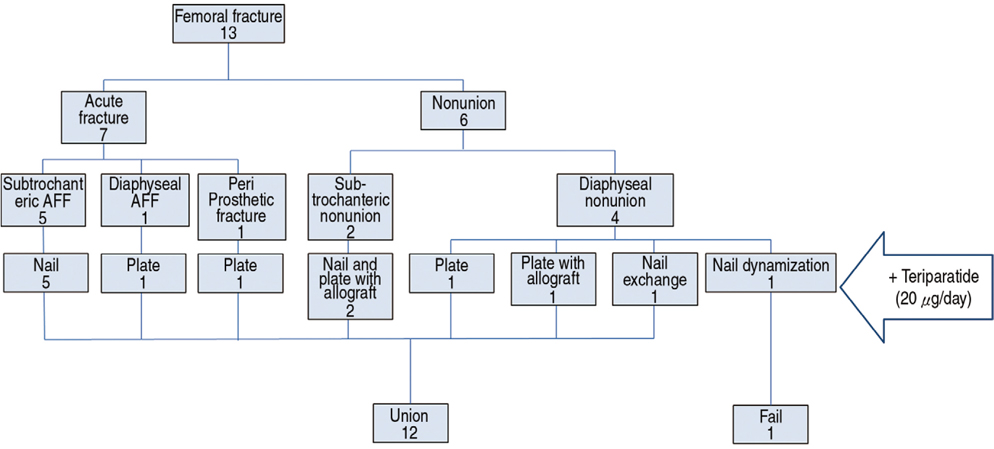
Thirteen patients who agreed to off label use of TPTD in combination of operation were included in this retrospective case series. Median patients' age was 68.7 years, and there were three male and ten female patients. Their diagnoses were nonunion in six patients and acute fracture in seven. Medical records and radiographic images were reviewed.
RESULTS
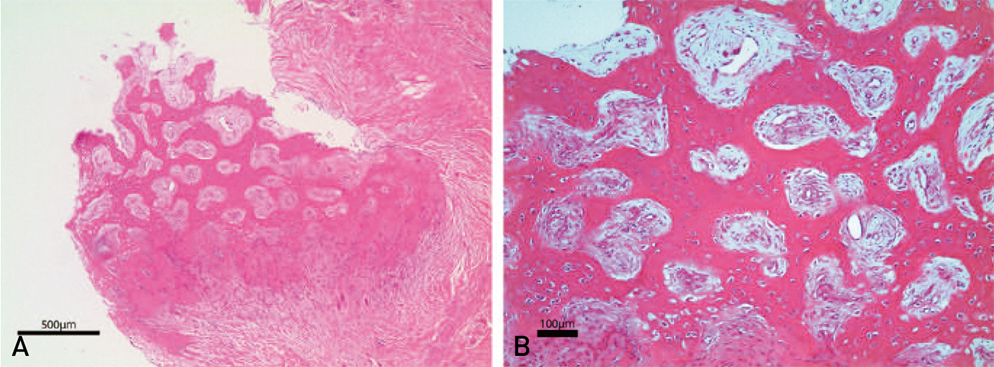
Twelve of thirteen fractures were united both clinically and radiologically within a year after adjuvant TPTD. Union completed radiologically median 5.4 months and clinically 5.7 months after the medication, respectively. Callus appeared abundantly showing median 1.4 of fracture healing response postoperatively. There was no serious adverse reaction of medication other than itching, muscle cramp, or nausea.
CONCLUSION
Even appropriate surgical treatment is a mainstay of treatment for AFF, PPFF, and FNU, the current report suggested that adjuvant TPTD combined with stable fixation results in satisfactory outcome for the challenging fractures of femur.
MeSH Terms
Figure
Reference
-
1. Kang JS, Won YY, Kim JO, et al. Atypical femoral fractures after anti-osteoporotic medication: a Korean multicenter study. Int Orthop. 2014; 38:1247–1253.
Article2. Finkemeier CG, Chapman MW. Treatment of femoral diaphyseal nonunions. Clin Orthop Relat Res. 2002; (398):223–234.
Article3. Holder N, Papp S, Gofton W, Beaulé PE. Outcomes following surgical treatment of periprosthetic femur fractures: a single centre series. Can J Surg. 2014; 57:209–213.
Article4. Weil YA, Rivkin G, Safran O, Liebergall M, Foldes AJ. The outcome of surgically treated femur fractures associated with long-term bisphosphonate use. J Trauma. 2011; 71:186–190.
Article5. Gelalis ID, Politis AN, Arnaoutoglou CM, et al. Diagnostic and treatment modalities in nonunions of the femoral shaft: a review. Injury. 2012; 43:980–988.
Article6. Saita Y, Ishijima M, Kaneko K. Atypical femoral fractures and bisphosphonate use: current evidence and clinical implications. Ther Adv Chronic Dis. 2015; 6:185–193.
Article7. Frenzel S, Vécsei V, Negrin L. Periprosthetic femoral fractures--incidence, classification problems and the proposal of a modified classification scheme. Int Orthop. 2015; 39:1909–1920.
Article8. Tashjian AH Jr, Gagel RF. Teriparatide [human PTH (1-34)]: 2.5 years of experience on the use and safety of the drug for the treatment of osteoporosis. J Bone Miner Res. 2006; 21:354–365.
Article9. Lee YK, Ha YC, Koo KH. Teriparatide, a nonsurgical solution for femoral nonunion? A report of three cases. Osteoporos Int. 2012; 23:2897–2900.
Article10. Hak DJ, Fitzpatrick D, Bishop JA, et al. Delayed union and nonunions: epidemiology, clinical issues, and financial aspects. Injury. 2014; 45:Suppl 2. S3–S7.
Article11. Shane E, Burr D, Abrahamsen B, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2014; 29:1–23.
Article12. Masri BA, Meek RM, Duncan CP. Periprosthetic fractures evaluation and treatment. Clin Orthop Relat Res. 2004; (420):80–95.
Article13. Corrales LA, Morshed S, Bhandari M, Miclau T 3rd. Variability in the assessment of fracture-healing in orthopaedic trauma studies. J Bone Joint Surg Am. 2008; 90:1862–1868.
Article14. Tower SS, Beals RK, Duwelius PJ. Resonant frequency analysis of the tibia as a measure of fracture healing. J Orthop Trauma. 1993; 7:552–557.
Article15. Heckman JD, Ryaby JP, McCabe J, Frey JJ, Kilcoyne RF. Acceleration of tibial fracture-healing by non-invasive, low-intensity pulsed ultrasound. J Bone Joint Surg Am. 1994; 76:26–34.
Article16. Spencer RF. The effect of head injury on fracture healing. A quantitative assessment. J Bone Joint Surg Br. 1987; 69:525–528.
Article17. Kanakaris NK, Lasanianos N, Calori GM, et al. Application of bone morphogenetic proteins to femoral non-unions: a 4-year multicentre experience. Injury. 2009; 40:Suppl 3. S54–S61.
Article18. Virk MS, Lieberman JR. Biologic adjuvants for fracture healing. Arthritis Res Ther. 2012; 14:225.
Article19. Carragee EJ, Hurwitz EL, Weiner BK. A critical review of recombinant human bone morphogenetic protein-2 trials in spinal surgery: emerging safety concerns and lessons learned. Spine J. 2011; 11:471–491.
Article20. Nozaka K, Miyakoshi N, Kasukawa Y, Maekawa S, Noguchi H, Shimada Y. Intermittent administration of human parathyroid hormone enhances bone formation and union at the site of cancellous bone osteotomy in normal and ovariectomized rats. Bone. 2008; 42:90–97.
Article21. Bostrom MP, Gamradt SC, Asnis P, et al. Parathyroid hormone-related protein analog RS-66271 is an effective therapy for impaired bone healing in rabbits on corticosteroid therapy. Bone. 2000; 26:437–442.
Article22. Hamann C, Picke AK, Campbell GM, et al. Effects of parathyroid hormone on bone mass, bone strength, and bone regeneration in male rats with type 2 diabetes mellitus. Endocrinology. 2014; 155:1197–1206.
Article23. Sloan AV, Martin JR, Li S, Li J. Parathyroid hormone and bisphosphonate have opposite effects on stress fracture repair. Bone. 2010; 47:235–240.
Article24. Uemura T, Okada M, Yokoi T, Shintani K, Nakamura H. Successful bone healing of nonunion after ulnar shortening osteotomy for smokers treated with teriparatide. Orthopedics. 2015; 38:e733–e737.
Article25. Tarazona-Santabalbina FJ, Aguilella-Fernández L. Bisphosphonate long-term treatment related bilateral subtrochanteric femoral fracture. Can teriparatide be useful? Aging Clin Exp Res. 2013; 25:605–609.
Article26. Miyakoshi N, Aizawa T, Sasaki S, et al. Healing of bisphosphonate-associated atypical femoral fractures in patients with osteoporosis: a comparison between treatment with and without teriparatide. J Bone Miner Metab. 2015; 33:553–559.
Article27. Qiu Z, Wei L, Liu J, et al. Effect of intermittent PTH (1-34) on posterolateral spinal fusion with iliac crest bone graft in an ovariectomized rat model. Osteoporos Int. 2013; 24:2693–2700.
Article28. Lynch JR, Taitsman LA, Barei DP, Nork SE. Femoral nonunion: risk factors and treatment options. J Am Acad Orthop Surg. 2008; 16:88–97.
Article29. Axelrad TW, Einhorn TA. Use of clinical assessment tools in the evaluation of fracture healing. Injury. 2011; 42:301–305.
Article30. Briot K, Ravaud P, Dargent-Molina P, Zylberman M, Liu-Leage S, Roux C. Persistence with teriparatide in postmenopausal osteoporosis; impact of a patient education and follow-up program: the French experience. Osteoporos Int. 2009; 20:625–630.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Atypical Femoral Fractures: What Do We Know about Them?
- Effect of Teriparatide on Healing of Atypical Femoral Fractures: A Systemic Review
- Surgical Treatment of the Atypical Femoral Fracture: Overcoming Femoral Bowing
- Effects of Teriparatide Administration on Fracture Healing after Intramedullary Nailing in Atypical Femoral Fractures
- Short-term Treatment Comparison of Teriparatide and Percutaneous Vertebroplasty in Patients with Acute Osteoporotic Vertebral Compression Fractures