Lab Med Online.
2016 Oct;6(4):221-227. 10.3343/lmo.2016.6.4.221.
Association of Homocysteine Levels with Subclinical Coronary Atherosclerosis in Asymptomatic Subjects
- Affiliations
-
- 1Department of Laboratory Medicine and Health Promotion Research Institute, Korea Association of Health Promotion, Seoul, Korea. cellonah@hanmail.net
- 2Korea Association of Health Promotion, Seoul, Korea.
- 3Department of Radiology, Korea Association of Health Promotion, Seoul, Korea.
- KMID: 2353423
- DOI: http://doi.org/10.3343/lmo.2016.6.4.221
Abstract
- BACKGROUND
Progression of atherosclerotic plaques is known to be correlated with elevated circulating homocysteine (Hcy). However, whether the level of Hcy is related with coronary atherosclerosis in the subclinical state is unclear. Therefore, we performed this study to investigate the relationship between blood Hcy levels and subclinical atherosclerosis in asymptomatic self-referred subjects.
METHODS
We retrospectively enrolled 2,968 self-referred asymptomatic subjects (1,374 men, 1,594 women) who had undergone both coronary CT angiography (CCTA) and coronary artery calcium scoring. The relationships between atherosclerosis, Hcy, and other clinical factors were assessed.
RESULTS
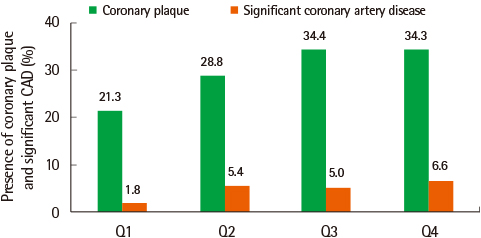
Higher levels of Hcy were related with age, male gender, body mass index (BMI), waist circumference, blood pressure, high density lipoprotein (HDL), triglyceride, blood glucose, HbA1c, hsCRP, and coronary artery calcium score (CACS). Coronary plaque was more frequently found in higher Hcy quartile groups (21.3%, 28.8%, 34.4%, and 34.3%, P<0.001). Significant coronary artery stenosis (stenosis>50%) was also more frequent in higher Hcy quartile groups (1.8%, 5.4%, 5.0%, and 6.6%, P<0.001). The factors associated with CACS included age, male gender, levels of HbA1c, Hcy and hsCRP. Logistic regression analysis adjusted for gender and confounding factors showed that the third- and fourth-quartile Hcy groups had higher odds ratios [odd ratio (OR) 3.980 (1.723-9.194), P=0.001, 7.355 (3.291-16.439), P<0.001, respectively] for high CACS (CACS >400) than the first quartile group.
CONCLUSIONS
Blood Hcy levels were associated with an increased risk of the presence and extent of subclinical atherosclerosis in asymptomatic subjects.
Keyword
MeSH Terms
-
Angiography
Atherosclerosis
Blood Glucose
Body Mass Index
Calcium
Coronary Artery Disease*
Coronary Stenosis
Coronary Vessels
Homocysteine*
Humans
Hypertension
Lipoproteins
Logistic Models
Male
Odds Ratio
Plaque, Atherosclerotic
Retrospective Studies
Triglycerides
Waist Circumference
Blood Glucose
Calcium
Homocysteine
Lipoproteins
Figure
Reference
-
1. Choi EK, Choi SI, Rivera JJ, Nasir K, Chang SA, Chun EJ, et al. Coronary computed tomography angiography as a screening tool for the detection of occult coronary artery disease in asymptomatic individuals. J Am Coll Cardiol. 2008; 52:357–365.
Article2. Myerburg RJ, Interian A Jr, Mitrani RM, Kessler KM, Castellanos A. Frequency of sudden cardiac death and profiles of risk. Am J Cardiol. 1997; 80:10–9F.
Article3. Schaffer A, Verdoia M, Cassetti E, Marino P, Suryapranata H, De Luca G, et al. Relationship between homocysteine and coronary artery disease. Results from a large prospective cohort study. Thromb Res. 2014; 134:288–293.
Article4. Klerk M, Verhoef P, Clarke R, Blom HJ, Kok FJ, Schouten EG. MTHFR 677C-->T polymorphism and risk of coronay heart disease: a meta-analysis. JAMA. 2002; 288:2023–2031.
Article5. Rasouli ML, Nasir K, Blumenthal RS, Park R, Aziz DC, Budoff MJ. Plasma homocysteine predicts progression of atherosclerosis. Atherosclerosis. 2005; 181:159–165.
Article6. Kullo IJ, Bielak LF, Bailey KR, Sheedy PF II, Peyser PA, Li G, et al. Association of plasma homocysteine with coronary artery calcification in different categories of coronary heart disease risk. Mayo Clin Proc. 2006; 81:177–182.
Article7. Taylor AJ, Feuerstein I, Wong H, Barko W, Brazaitis M, O'Malley PG. Do conventional risk factors predict subclinical coronary artery disease? Results from the Prospective Army Coronary Calcium Project. Am Heart J. 2001; 141:463–468.
Article8. Hunt ME, O'Malley PG, Vernalis MN, Feuerstein IM, Taylor AJ. C-reactive protein is not associated with the presence or extent of calcified subclinical atherosclerosis. Am Heart J. 2001; 141:206–210.
Article9. Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990; 15:827–832.
Article10. Austen WG, Edwards JE, Frye RL, Gensini GG, Gott VL, Griffith LS. A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation. 1975; 51:4 Suppl. 5–40.
Article11. Lin T, Liu JC, Chang LY, Shen CW. Association of C-reactive protein and homocysteine with subclinical coronary plaque subtype and stenosis using low-dose MDCT coronary angiography. Atherosclerosis. 2010; 21:501–506.
Article12. Nasir K. Role of nonenhanced multidetector CT coronary artery calcium testing in asymptomatic and symptomatic individuals. Radiology. 2012; 264:637–649.
Article13. Kunita E, Yamamoto H, Kitagawa T, Ohashi N, Oka T, Utsunomiya H, et al. Prognostic value of coronary artery calcium and epicardial adipose tissue assessed by non-contrast cardiac computed tomography. Atherosclerosis. 2014; 233:447–453.
Article14. Stuhlinger MC, Tsao PS, Her JH, Kimoto M, Balint RF, Cooke JP. Homocysteine impairs the nitric oxide synthase pathway: role of asymmetric dimethylarginine. Circulation. 2001; 104:2569–2575.15. Ungvari Z, Csiszar A, Edwards JG, Kaminski PM, Wolin MS, Kaley G, et al. Increased superoxide production in coronary arteries in hyperhomocysteinemia: role of tumor necrosis factor-alpha, NAD(P)H oxidase, and inducible nitric oxide synthase. Arterioscler Thromb Vasc Biol. 2003; 23:418–424.
Article16. Jin L, Caldwell RB, Li-Masters T, Caldwell RW. Homocysteine induces endothelial dysfunction via inhibition of arginine transport. J Physiol Pharmacol. 2007; 58:191–206.17. Bienvenu T, Ankri A, Chadefaux B, Montalescot G, Kamoun P. Elevated total plasma homocysteine, a risk factor for thrombosis. Relation to coagulation and fibrinolytic parameters. Thromb Res. 1993; 70:123–129.
Article18. Woo KS, Chook P, Lolin YI, Cheung AS, Chan LT, Sun YY, et al. Hyper-homocyst(e)inemia is a risk factor for arterial endothelial dysfunction in humans. Circulation. 1997; 96:2542–2544.
Article19. Kullo IJ, Li G, Bielak LF, Bailey KR, Sheedy PF 2nd, Peyser PA, et al. Association of plasma homocysteine with coronary artery calcification in different categories of coronary heart disease risk. Mayo Clin Proc. 2006; 81:177–182.
Article20. Grundy SM, Pasternak R, Greenland P, Smith S Jr, Fuster V. Assessment of cardiovascular risk by use of multiple-risk-factor assessment equations: a statement for healthcare professionals from the American Heart Association and the American College of Cariology. Circulation. 1999; 100:1481–1492.
Article21. Graham IM, Daly LE, Refsum HM, Robinson K, Brattstrom LE, Ueland PM, et al. Plasma homocysteine as a risk factor for vascular disease. The European Concerted Action Project. JAMA. 1997; 277:1775–1781.
Article22. Selhub J, Jacques PF, Bostom AG, D'Agostino RB, Wilson PW, Belanger AJ. Association between plasma homocysteine concentrations and extracranial carotid-artery stenosis. N Engl J Med. 1995; 332:286–291.
Article23. Van den, Stehouwer CD, Bierdrager E, Rauwerda JA. Plasma homocysteine and severity of atherosclerosis in young patients with lower-limb atherosclerotic disease. Arterioscler Thromb Vasc Biol. 1996; 16:165–171.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Association of Blood Homocysteine levels with Subclinical Atherosclerosis in Impaired Fasting Glucose
- Homocysteine and Atherosclerosis
- Common Mutation of Methylenetetrahydrofolate Reductass and Homocysteine in Patients with Coronary Artery Disease
- Plasma Homocysteine, Folate and Vitamin B12 Concentrations in Coronary Artery Disease
- Pathogenesis of Coronary Atherosclerosis