J Cardiovasc Ultrasound.
2016 Sep;24(3):201-207. 10.4250/jcu.2016.24.3.201.
Impact of Valvuloarterial Impedance on Concentric Remodeling in Aortic Stenosis and Its Regression after Valve Replacement
- Affiliations
-
- 1Cardiac Imaging Center, Asan Medical Center Heart Institute, University of Ulsan College of Medicine, Seoul, Korea. jksong@amc.seoul.kr
- 2Division of Cardiology, Department of Internal Medicine, Gyeongsang National University School of Medicine, Cardiovascular Center, Gyeongsang National University Changwon Hospital, Changwon, Korea.
- 3Division of Cardiology, Department of Internal Medicine, Busan Paik Hospital, Inje University College of Medicinen, Busan, Korea.
- 4Division of Cardiology, Department of Internal Medicine, Chungnam National University Hospital, Daejeon, Korea.
- KMID: 2353097
- DOI: http://doi.org/10.4250/jcu.2016.24.3.201
Abstract
- BACKGROUND
Left ventricle (LV) in patients with aortic stenosis (AS) faces a double hemodynamic load incorporating both valvular stenosis and reduced systemic arterial compliance (SAC). This study aimed to evaluate the impact of global LV afterload on LV hypertrophy (LVH) before and after aortic valve replacement (AVR).
METHODS
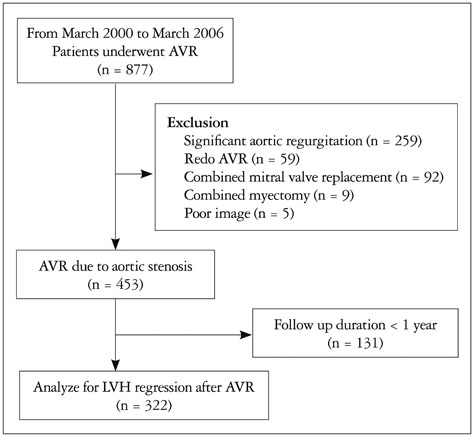
The study cohort included 453 patients (247 males; mean age, 64 ± 11 years) who underwent AVR. Pre- and post-AVR echocardiographic examinations were retrospectively analyzed including an index of valvuloarterial impedance (Z(VA)) and LV mass index/LV end-diastolic volume index (LVMI/LVEDVI) as a parameter of LVH.
RESULTS
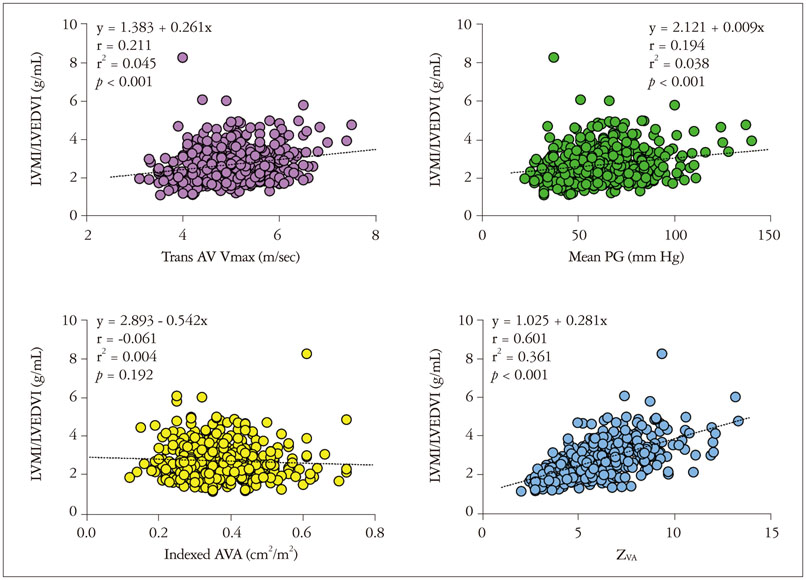
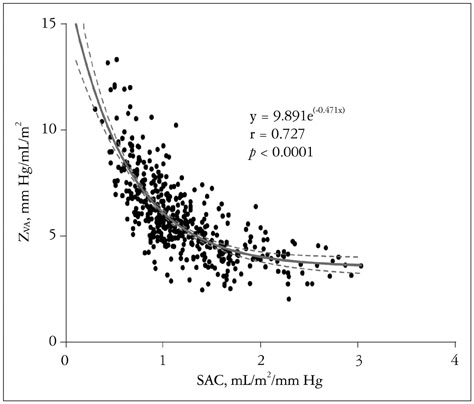
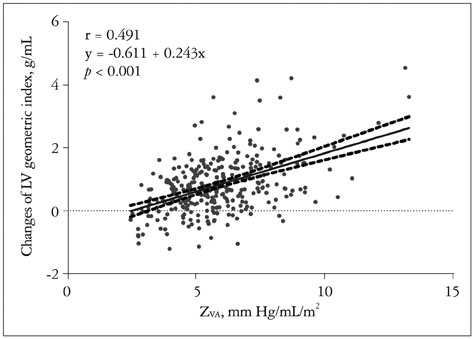
Pre-AVR LVMI/LVEDVI was 2.7 ± 0.9 g/mL with an aortic valve area (AVA) of 0.6 ± 0.2 cm². Z(VA) was 5.9 ± 1.9 mm Hg/mL/m² and showed a stronger correlation (β = 0.601, p < 0.001) with pre-AVR LVMI/LVEDVI than indexed AVA (β = 0.061, p = 0.19), transvalvular peak velocity (β = 0.211, p < 0.001). During a median follow-up of 3.5 years, patients had a 18.8 ± 10.4% decrease in the LV geometry index with a decrease in SAC from 1.20 ± 0.48 to 1.00 ± 0.38 mL/m²/mm Hg (p < 0.001). Pre-AVR LV ejection fraction (r = 0.284, p < 0.001) and Z(VA) (r = 0.523, p < 0.001) were independent factors associated with LVH regression in 322 patients with follow-up duration >1 year after AVR.
CONCLUSION
Z(VA) is a major determinant of concentric remodeling in AS before AVR and LVH regression after AVR, which should be incorporated in routine evaluation of AS.
MeSH Terms
Figure
Cited by 1 articles
-
Multimodality Imaging for the Assessment of Severe Aortic Stenosis
Sung-Ji Park, Marc R. Dweck
J Cardiovasc Imaging. 2019;27(4):235-246. doi: 10.4250/jcvi.2019.27.e48.
Reference
-
1. Briand M, Dumesnil JG, Kadem L, Tongue AG, Rieu R, Garcia D, Pibarot P. Reduced systemic arterial compliance impacts significantly on left ventricular afterload and function in aortic stenosis: implications for diagnosis and treatment. J Am Coll Cardiol. 2005; 46:291–298.2. Hachicha Z, Dumesnil JG, Bogaty P, Pibarot P. Paradoxical low-flow, low-gradient severe aortic stenosis despite preserved ejection fraction is associated with higher afterload and reduced survival. Circulation. 2007; 115:2856–2864.3. Hachicha Z, Dumesnil JG, Pibarot P. Usefulness of the valvuloarterial impedance to predict adverse outcome in asymptomatic aortic stenosis. J Am Coll Cardiol. 2009; 54:1003–1011.4. Cramariuc D, Cioffi G, Rieck AE, Devereux RB, Staal EM, Ray S, Wachtell K, Gerdts E. Low-flow aortic stenosis in asymptomatic patients: valvular-arterial impedance and systolic function from the SEAS Substudy. JACC Cardiovasc Imaging. 2009; 2:390–399.5. Weisz SH, Magne J, Dulgheru R, Caso P, Piérard LA, Lancellotti P. Carotid artery and aortic stiffness evaluation in aortic stenosis. J Am Soc Echocardiogr. 2014; 27:385–392.6. Rashedi N, Otto CM. Aortic stenosis: changing disease concepts. J Cardiovasc Ultrasound. 2015; 23:59–69.7. Baumgartner H, Otto CM. Aortic stenosis severity: do we need a new concept? J Am Coll Cardiol. 2009; 54:1012–1013.8. Lancellotti P, Donal E, Magne J, O'Connor K, Moonen ML, Cosyns B, Pierard LA. Impact of global left ventricular afterload on left ventricular function in asymptomatic severe aortic stenosis: a two-dimensional speckle-tracking study. Eur J Echocardiogr. 2010; 11:537–543.9. Zito C, Salvia J, Cusmà-Piccione M, Antonini-Canterin F, Lentini S, Oreto G, Di Bella G, Montericcio V, Carerj S. Prognostic significance of valvuloarterial impedance and left ventricular longitudinal function in asymptomatic severe aortic stenosis involving three-cuspid valves. Am J Cardiol. 2011; 108:1463–1469.10. Giannini C, Petronio AS, De Carlo M, Guarracino F, Benedetti G, Delle Donne MG, Dini FL, Marzilli M, Di Bello V. The incremental value of valvuloarterial impedance in evaluating the results of transcatheter aortic valve implantation in symptomatic aortic stenosis. J Am Soc Echocardiogr. 2012; 25:444–453.11. Samarendra P. Usefulness of valvuloarterial impedance to predict adverse outcomes in patients with asymptomatic aortic stenosis. J Am Coll Cardiol. 2010; 55:1164–1165.12. Levy F, Luc Monin J, Rusinaru D, Petit-Eisenmann H, Lelguen C, Chauvel C, Adams C, Metz D, Leleu F, Gueret P, Tribouilloy C. Valvuloarterial impedance does not improve risk stratification in low-ejection fraction, low-gradient aortic stenosis: results from a multicentre study. Eur J Echocardiogr. 2011; 12:358–363.13. Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ. Chamber Quantification Writing Group. American Society of Echocardiography's Guidelines and Standards Committee. European Association of Echocardiography. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005; 18:1440–1463.14. Seo JS, Jang MK, Lee EY, Yun SC, Kim DH, Song JM, Kang DH, Song JK. Evaluation of left ventricular diastolic function after valve replacement in aortic stenosis using exercise Doppler echocardiography. Circ J. 2012; 76:2792–2798.15. Kupari M, Turto H, Lommi J. Left ventricular hypertrophy in aortic valve stenosis: preventive or promotive of systolic dysfunction and heart failure? Eur Heart J. 2005; 26:1790–1796.16. Beach JM, Mihaljevic T, Rajeswaran J, Marwick T, Edwards ST, Nowicki ER, Thomas J, Svensson LG, Griffin B, Gillinov AM, Blackstone EH. Ventricular hypertrophy and left atrial dilatation persist and are associated with reduced survival after valve replacement for aortic stenosis. J Thorac Cardiovasc Surg. 2014; 147:362–369.e8.17. Pagé A, Dumesnil JG, Clavel MA, Chan KL, Teo KK, Tam JW, Mathieu P, Després JP, Pibarot P. ASTRONOMER Investigators. Metabolic syndrome is associated with more pronounced impairment of left ventricle geometry and function in patients with calcific aortic stenosis: a substudy of the ASTRONOMER (Aortic Stenosis Progression Observation Measuring Effects of Rosuvastatin). J Am Coll Cardiol. 2010; 55:1867–1874.18. Dellgren G, Eriksson MJ, Blange I, Brodin LA, Rådegran K, Sylvén C. Angiotensin-converting enzyme gene polymorphism influences degree of left ventricular hypertrophy and its regression in patients undergoing operation for aortic stenosis. Am J Cardiol. 1999; 84:909–913.19. Orlowska-Baranowska E, Placha G, Gaciong Z, Baranowski R, Zakrzewski D, Michalek P, Hoffman P, Rawczynska-Englert I. Influence of ACE I/D genotypes on left ventricular hypertrophy in aortic stenosis: gender-related differences. J Heart Valve Dis. 2004; 13:574–581.20. Chang SA, Kim HK, Sohn DW. Impact of afterload on the assessment of severity of aortic stenosis. J Cardiovasc Ultrasound. 2012; 20:79–84.21. Lund O, Erlandsen M, Dørup I, Emmertsen K, Flø C, Jensen FT. Predictable changes in left ventricular mass and function during ten years after valve replacement for aortic stenosis. J Heart Valve Dis. 2004; 13:357–368.22. Lund O, Emmertsen K, Dørup I, Jensen FT, Flø C. Regression of left ventricular hypertrophy during 10 years after valve replacement for aortic stenosis is related to the preoperative risk profile. Eur Heart J. 2003; 24:1437–1446.23. Hein S, Arnon E, Kostin S, Schönburg M, Elsässer A, Polyakova V, Bauer EP, Klövekorn WP, Schaper J. Progression from compensated hypertrophy to failure in the pressure-overloaded human heart: structural deterioration and compensatory mechanisms. Circulation. 2003; 107:984–991.24. Krayenbuehl HP, Hess OM, Monrad ES, Schneider J, Mall G, Turina M. Left ventricular myocardial structure in aortic valve disease before, intermediate, and late after aortic valve replacement. Circulation. 1989; 79:744–755.25. Weidemann F, Herrmann S, Störk S, Niemann M, Frantz S, Lange V, Beer M, Gattenlöhner S, Voelker W, Ertl G, Strotmann JM. Impact of myocardial fibrosis in patients with symptomatic severe aortic stenosis. Circulation. 2009; 120:577–584.26. Azevedo CF, Nigri M, Higuchi ML, Pomerantzeff PM, Spina GS, Sampaio RO, Tarasoutchi F, Grinberg M, Rochitte CE. Prognostic significance of myocardial fibrosis quantification by histopathology and magnetic resonance imaging in patients with severe aortic valve disease. J Am Coll Cardiol. 2010; 56:278–287.27. Park J, Chang HJ, Choi JH, Yang PS, Lee SE, Heo R, Shin S, Cho IJ, Kim YJ, Shim CY, Hong GR, Chung N. Late gadolinium enhancement in cardiac MRI in patients with severe aortic stenosis and preserved left ventricular systolic function is related to attenuated improvement of left ventricular geometry and filling pressure after aortic valve replacement. Korean Circ J. 2014; 44:312–319.28. Gaudino M, Alessandrini F, Glieca F, Luciani N, Cellini C, Pragliola C, Morelli M, Canosa C, Nasso G, Possati G. Survival after aortic valve replacement for aortic stenosis: does left ventricular mass regression have a clinical correlate? Eur Heart J. 2005; 26:51–57.29. Tsang W, Veronesi F, Sugeng L, Weinert L, Takeuchi M, Jeevanandam V, Lang RM. Mitral valve dynamics in severe aortic stenosis before and after aortic valve replacement. J Am Soc Echocardiogr. 2013; 26:606–614.30. Dahl JS, Videbaek L, Poulsen MK, Pellikka PA, Veien K, Andersen LI, Haghfelt T, Møller JE. Effect of candesartan treatment on left ventricular remodeling after aortic valve replacement for aortic stenosis. Am J Cardiol. 2010; 106:713–719.31. Palmieri V, Dahlöf B, DeQuattro V, Sharpe N, Bella JN, de Simone G, Paranicas M, Fishman D, Devereux RB. Reliability of echocardiographic assessment of left ventricular structure and function: the PRESERVE study. Prospective Randomized Study Evaluating Regression of Ventricular Enlargement. J Am Coll Cardiol. 1999; 34:1625–1632.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Expanding transcatheter aortic valve replacement into uncharted indications
- Right Coronary Artery Ostial Stenosis after Re-do Aortic Valve Replacement
- Aortic Stenosis and Transcatheter Aortic Valve Implantation: Current Status and Future Directions in Korea
- Valve-Sparing Root Replacement: Aortic Root Remodeling with External Subvalvular Ring Annuloplasty
- A Study of Pure Aortic Valvular Stenosis in Adult