Yonsei Med J.
2015 Jan;56(1):154-158. 10.3349/ymj.2015.56.1.154.
Effect of the Starting Point of Half-Pin Insertion on the Insertional Torque of the Pin at the Tibia
- Affiliations
-
- 1Department of Orthopaedic Surgery, Arthroscopy and Joint Research Institute, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. min1201@hanmail.net
- KMID: 2352801
- DOI: http://doi.org/10.3349/ymj.2015.56.1.154
Abstract
- PURPOSE
The authors have observed a failure to achieve secure fixation in elderly patients when inserting a half-pin at the anteromedial surface of the tibia. The purpose of this study was to compare two methods for inserting a half-pin at tibia diaphysis in elderly patients.
MATERIALS AND METHODS
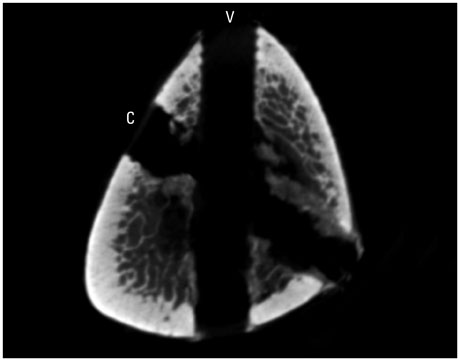
Twenty cadaveric tibias were divided into Group C or V. A half-pin was inserted into the tibias of Group C via the conventional method, from the anteromedial surface to the interosseous border of the tibia diaphysis, and into the tibias of Group V via the vertical method, from the anterior border to the posterior surface at the same level. The maximum insertion torque was measured during the bicortical insertion with a torque driver. The thickness of the cortex was measured by micro-computed tomography. The relationship between the thickness of the cortex engaged and the insertion torque was investigated.
RESULTS
The maximum insertion torque and the thickness of the cortex were significantly higher in Group V than Group C. Both groups exhibited a statistically significant linear correlation between torque and thickness by Spearman's rank correlation analysis.
CONCLUSION
Half-pins inserted by the vertical method achieved purchase of more cortex than those inserted by the conventional method. Considering that cortical thickness and insertion torque in Group V were significantly greater than those in Group C, we suggest that the vertical method of half-pin insertion may be an alternative to the conventional method in elderly patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Giannoudis PV, Schneider E. Principles of fixation of osteoporotic fractures. J Bone Joint Surg Br. 2006; 88:1272–1278.
Article2. Donaldson FE, Pankaj P, Simpson AH. Bone properties affect loosening of half-pin external fixators at the pin-bone interface. Injury. 2012; 43:1764–1770.
Article3. Hyldahl C, Pearson S, Tepic S, Perren SM. Induction and prevention of pin loosening in external fixation: an in vivo study on sheep tibiae. J Orthop Trauma. 1991; 5:485–492.4. Donaldson FE, Pankaj P, Simpson AH. Investigation of factors affecting loosening of Ilizarov ring-wire external fixator systems at the bone-wire interface. J Orthop Res. 2012; 30:726–732.
Article5. Parameswaran AD, Roberts CS, Seligson D, Voor M. Pin tract infection with contemporary external fixation: how much of a problem? J Orthop Trauma. 2003; 17:503–507.
Article6. Koval KJ, Meek R, Schemitsch E, Liporace F, Strauss E, Zuckerman JD. An AOA critical issue. Geriatric trauma: young ideas. J Bone Joint Surg Am. 2003; 85-A:1380–1388.7. Seebeck J, Goldhahn J, Morlock MM, Schneider E. Mechanical behavior of screws in normal and osteoporotic bone. Osteoporos Int. 2005; 16:Suppl 2. S107–S111.
Article8. Ziran BH, Smith WR, Anglen JO, Tornetta P 3rd. External fixation: how to make it work. J Bone Joint Surg Am. 2007; 89:1620–1632.9. Hoang-Kim A, Scott J, Micera G, Orsini R, Moroni A. Functional assessment in patients with osteoporotic wrist fractures treated with external fixation: a review of randomized trials. Arch Orthop Trauma Surg. 2009; 129:105–111.
Article10. Russo CR, Lauretani F, Seeman E, Bartali B, Bandinelli S, Di Iorio A, et al. Structural adaptations to bone loss in aging men and women. Bone. 2006; 38:112–118.
Article11. Currey JD. Changes in the impact energy absorption of bone with age. J Biomech. 1979; 12:459–469.
Article12. Donaldson FE, Pankaj P, Cooper DM, Thomas CD, Clement JG, Simpson AH. Relating age and micro-architecture with apparent-level elastic constants: a micro-finite element study of female cortical bone from the anterior femoral midshaft. Proc Inst Mech Eng H. 2011; 225:585–596.
Article13. Wikenheiser MA, Markel MD, Lewallen DG, Chao EY. Thermal response and torque resistance of five cortical half-pins under simulated insertion technique. J Orthop Res. 1995; 13:615–619.
Article14. Hutchinson DT, Bachus KN, Higgenbotham T. External fixation of the distal radius: to predrill or not to predrill. J Hand Surg Am. 2000; 25:1064–1068.
Article15. Oliphant BW, Kim H, Osgood GM, Golden RD, Hawks MA, Hsieh AH, et al. Predrilling does not improve the pullout strength of external fixator pins: a biomechanical study. J Orthop Trauma. 2013; 27:e25–e30.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Biomechanics of Hybrid External Fixator: The Effect of Periarticular Half Pin on Frame Stiffness
- Removal torque of bicortically stabilized RBM(resorbable blast media) pin implants in rabbit tibia
- Bilateral Subtrochanteric fracture After Pin Removal in Slipped Capital Femoral Epiphysis: A Case Report
- Comparison of histologic observation and insertional and removal torque values between titanium grade 2 and 4 microimplants
- Screw Insertional Torque Measurement in Spine Surgery: Correlation With Bone Mineral Density and Hounsfield Unit