Korean J Hepatobiliary Pancreat Surg.
2016 Aug;20(3):137-143. 10.14701/kjhbps.2016.20.3.137.
Surgical treatment of mucin-producing cholangiocarcinoma arising from intraductal papillary neoplasm of the intrahepatic bile duct: a report of 2 cases
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. shwang@amc.seoul.kr
- 2Department of Internal Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 3Department of General Surgery, Mongolian National University of Medical Science Hospital, Ulaanbaatar, Mongolia.
- KMID: 2351302
- DOI: http://doi.org/10.14701/kjhbps.2016.20.3.137
Abstract
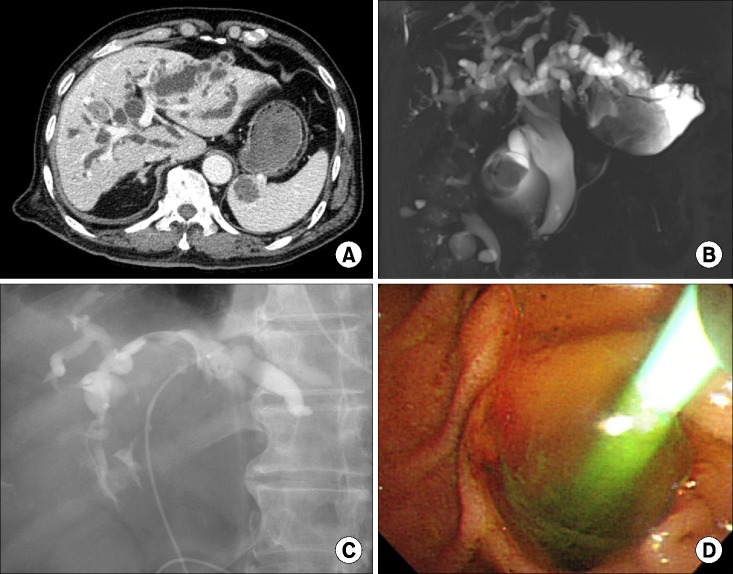
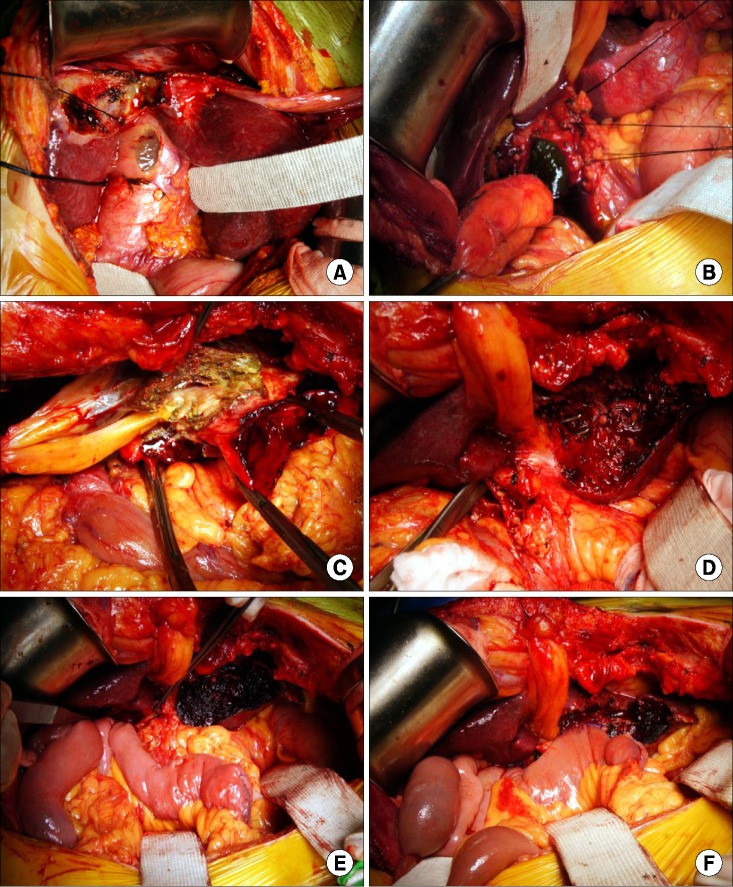
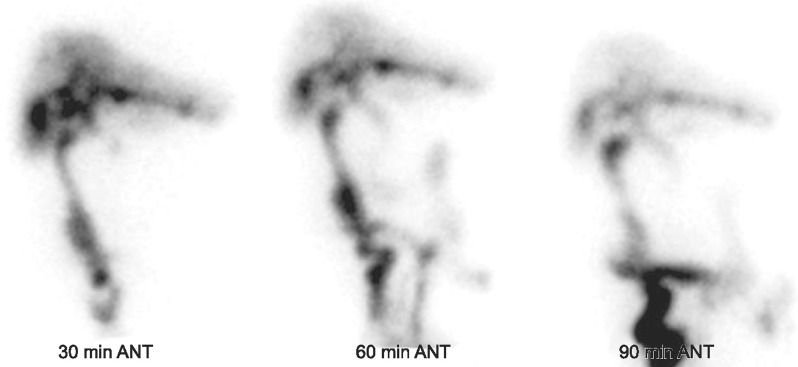
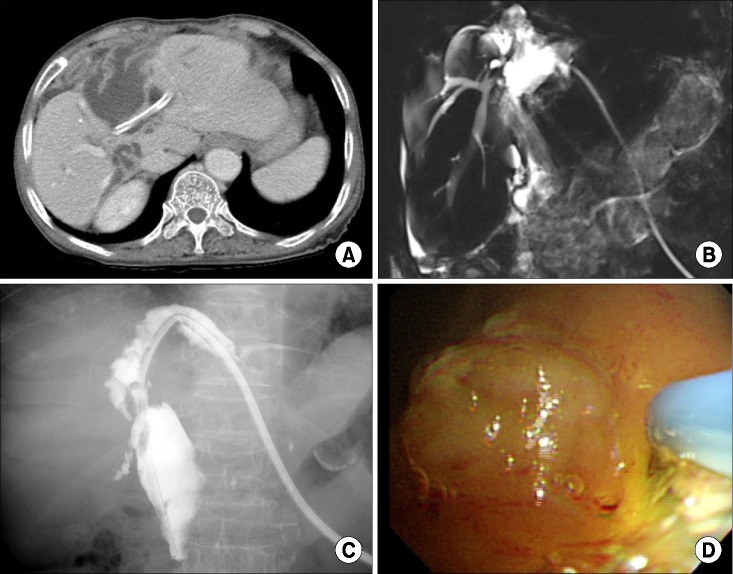
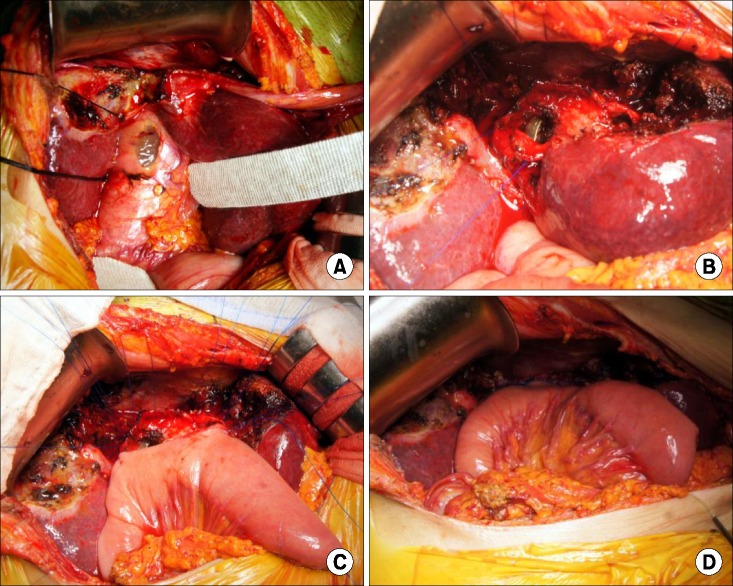
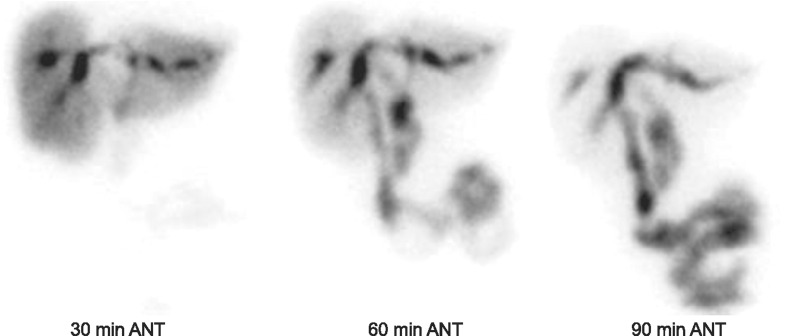
- Intraductal papillary neoplasms of the bile duct (IPNB) leads to malignant transformation and mucin production. Herein, we presented two cases of mucin-producing IPNB with obstructive jaundice who underwent resection of the intrahepatic lesions and bypass hepaticojejunostomy. The first case was a 69 year-old male patient with 5-year follow up for gallstone disease. Imaging studies showed mucin-secreting IPNB mainly in the hepatic segment III bile duct (B3) and multiple intrahepatic duct stones for which, segment III resection, intrahepatic stone removal, end-to-side choledochojejunostomy and B3 hepaticojejunostomy were conducted. The second case was a 74 year-old female patient with 11-year follow up for gallstone disease. Imaging studies showed mucin-producing IPNB with dilatation of the segment IV duct (B4) and mural nodules for which, segment IV resection, partial resection of the diaphragm and central hepaticojejunostomy were conducted. Both patients recovered uneventfully from surgery. These cases highlight that in patients with IPNB, abundant production of highly viscous mucin inducing obstructive jaundice may be associated with malignant transformation.
Keyword
MeSH Terms
Figure
Reference
-
1. Kim WJ, Hwang S, Lee YJ, Kim KH, Park KM, Ahn CS, et al. Clinicopathological features and long-term outcomes of intraductal papillary neoplasms of the intrahepatic bile duct. J Gastrointest Surg. 2016; 20:1368–1375. PMID: 26873016.
Article2. Nakanuma Y, Sato Y, Harada K, Sasaki M, Xu J, Ikeda H. Pathological classification of intrahepatic cholangiocarcinoma based on a new concept. World J Hepatol. 2010; 2:419–427. PMID: 21191517.
Article3. Itatsu K, Zen Y, Ohira S, Ishikawa A, Sato Y, Harada K, et al. Immunohistochemical analysis of the progression of flat and papillary preneoplastic lesions in intrahepatic cholangiocarcinogenesis in hepatolithiasis. Liver Int. 2007; 27:1174–1184. PMID: 17919228.
Article4. Nakanuma Y. A novel approach to biliary tract pathology based on similarities to pancreatic counterparts: is the biliary tract an incomplete pancreas? Pathol Int. 2010; 60:419–429. PMID: 20518896.
Article5. Lee SS, Kim MH, Lee SK, Jang SJ, Song MH, Kim KP, et al. Clinicopathologic review of 58 patients with biliary papillomatosis. Cancer. 2004; 100:783–793. PMID: 14770435.
Article6. Rocha FG, Lee H, Katabi N, DeMatteo RP, Fong Y, D'Angelica MI, et al. Intraductal papillary neoplasm of the bile duct: a biliary equivalent to intraductal papillary mucinous neoplasm of the pancreas? Hepatology. 2012; 56:1352–1360. PMID: 22504729.
Article7. Furukawa T, Klöppel G, Volkan Adsay N, Albores-Saavedra J, Fukushima N, Horii A, et al. Classification of types of intraductal papillary-mucinous neoplasm of the pancreas: a consensus study. Virchows Arch. 2005; 447:794–799. PMID: 16088402.
Article8. Ohtsuka M, Shimizu H, Kato A, Yoshitomi H, Furukawa K, Tsuyuguchi T, et al. Intraductal papillary neoplasms of the bile duct. Int J Hepatol. 2014; 2014:459091. PMID: 24949206.
Article9. Yeh TS, Tseng JH, Chiu CT, Liu NJ, Chen TC, Jan YY, et al. Cholangiographic spectrum of intraductal papillary mucinous neoplasm of the bile ducts. Ann Surg. 2006; 244:248–253. PMID: 16858187.
Article10. Wu SD, Lu CD, Lu CJ, Huang J, Zhou J. Mucin-producing intrahepatic biliary papillomatosis. Surg Today. 2010; 40:845–850. PMID: 20740348.
Article11. Yang J, Wang W, Yan L. The clinicopathological features of intraductal papillary neoplasms of the bile duct in a Chinese population. Dig Liver Dis. 2012; 44:251–256. PMID: 21930444.
Article12. Naito Y, Kusano H, Nakashima O, Sadashima E, Hattori S, Taira T, et al. Intraductal neoplasm of the intrahepatic bile duct: clinicopathological study of 24 cases. World J Gastroenterol. 2012; 18:3673–3680. PMID: 22851859.
Article13. Kloek JJ, van der Gaag NA, Erdogan D, Rauws EA, Busch OR, Gouma DJ, et al. A comparative study of intraductal papillary neoplasia of the biliary tract and pancreas. Hum Pathol. 2011; 42:824–832. PMID: 21292296.
Article14. Zen Y, Fujii T, Itatsu K, Nakamura K, Minato H, Kasashima S, et al. Biliary papillary tumors share pathological features with intraductal papillary mucinous neoplasm of the pancreas. Hepatology. 2006; 44:1333–1343. PMID: 17058219.
Article15. Wu SD, Lu CD, Lu CJ, Huang J, Zhou J. Mucin-producing intrahepatic biliary papillomatosis. Surg Today. 2010; 40:845–850. PMID: 20740348.
Article16. Ohtsuka M, Kimura F, Shimizu H, Yoshidome H, Kato A, Yoshitomi H, et al. Similarities and differences between intraductal papillary tumors of the bile duct with and without macroscopically visible mucin secretion. Am J Surg Pathol. 2011; 35:512–521. PMID: 21412069.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intrahepatic and extrahepatic intraductal papillary neoplasms of bile duct
- Photodynamic Therapy Followed by Left Hepatectomy Used to Treat an Intraductal Papillary Mucinous Neoplasm of the Bile Duct
- Intraductal Papillary Mucinous Neoplasm of the Bile Ducts
- Intrahepatic cholangiocarcinoma presenting as liver Abscess: Report of Two Cases
- Extrahepatic Bile Duct Duplication with Intraductal Papillary Neoplasm: A Case Report