Korean J Crit Care Med.
2016 May;31(2):140-145. 10.4266/kjccm.2016.31.2.140.
Lethal Hyperammonemia due to Ornithine Transcarbamylase Deficiency in a Patient with Severe Septic Shock
- Affiliations
-
- 1Division of Pulmonology, Department of Internal Medicine, Severance Hospital, Institute of Chest Diseases, Yonsei University College of Medicine, Seoul, Korea. pms70@yuhs.ac
- KMID: 2350922
- DOI: http://doi.org/10.4266/kjccm.2016.31.2.140
Abstract
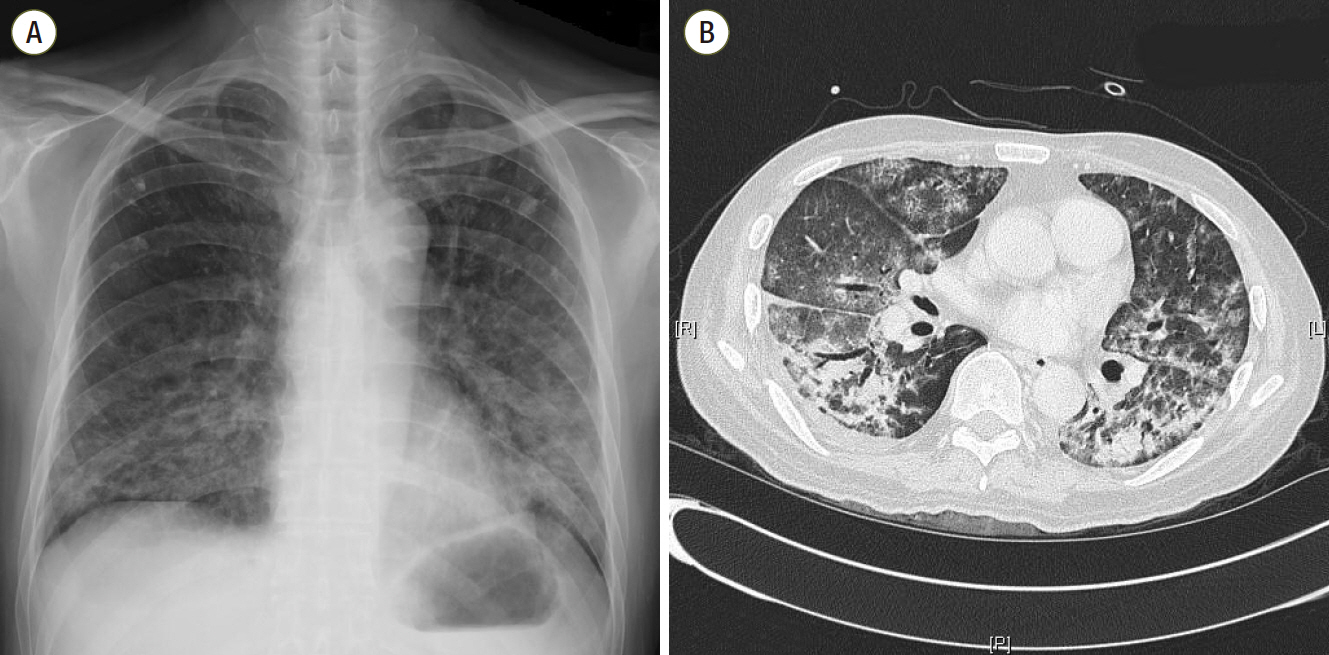
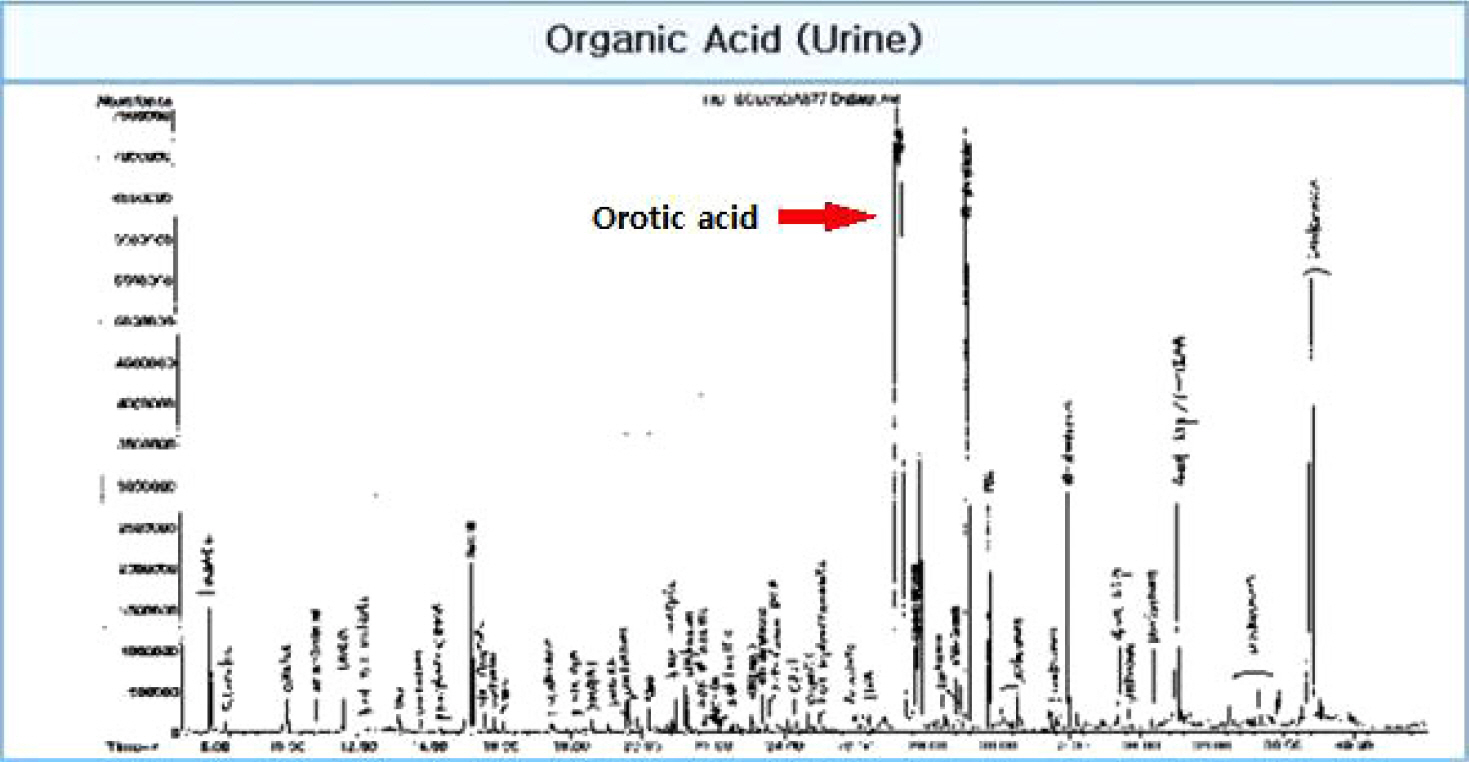
- Severe hyperammonemia can occur as a result of inherited or acquired liver enzyme defects in the urea cycle, among which ornithine transcarbamylase deficiency (OTCD) is the most common form. We report a very rare case of a 45-year-old Korean male who was admitted to the intensive care unit (ICU) due to severe septic shock with acute respiratory failure caused by Pneumocystis jiroveci pneumonia. During his ICU stay with ventilator care, the patient suffered from marked hyperammonemia (>1,700 µg/dL) with abrupt mental change leading to life-threatening cerebral edema. Despite every effort including continuous renal replacement therapy and use of a molecular adsorbent recirculating system (extracorporeal liver support-albumin dialysis) to lower his serum ammonia level, the patient was not recovered. The lethal hyperammonemia in the patient was later proven to be a manifestation of acquired liver enzyme defect known as OTCD, which is triggered by serious catabolic conditions, such as severe septic shock with acute respiratory failure.
Keyword
MeSH Terms
-
Ammonia
Brain Edema
Humans
Hyperammonemia*
Intensive Care Units
Liver
Male
Middle Aged
Ornithine Carbamoyltransferase Deficiency Disease*
Ornithine Carbamoyltransferase*
Ornithine*
Pneumocystis jirovecii
Pneumonia
Renal Replacement Therapy
Respiratory Insufficiency
Shock, Septic*
Urea
Ventilators, Mechanical
Ammonia
Ornithine
Ornithine Carbamoyltransferase
Urea
Figure
Reference
-
References
1. Gropman AL, Summar M, Leonard JV. Neurological implications of urea cycle disorders. J Inherit Metab Dis. 2007; 30:865–79.
Article2. Shawcross D, Jalan R. The pathophysiologic basis of hepatic encephalopathy: central role for ammonia and inflammation. Cell Mol Life Sci. 2005; 62:2295–304.
Article3. Vaquero J, Chung C, Cahill ME, Blei AT. Pathogenesis of hepatic encephalopathy in acute liver failure. Semin Liver Dis. 2003; 23:259–69.
Article4. Clay AS, Hainline BE. Hyperammonemia in the ICU. Chest. 2007; 132:1368–78.
Article5. Bachmann C. Inherited hyperammonemia. Physicians Guide to the Laboratory Diagnosis of Metabolic Diseases. 2nd ed. In : Blau N, Duran M, Blaskovics ME, Gibson KM, editors. Berlin: Springer;2003. p. 261–76.6. Brusilow SW, Horwich AL. Urea cycle enzymes. The Metabolic and Molecular and Bases of Inherited Disease, 4 volume. 8th ed. In : Scriver CR, Beaudet AL, Valle D, Sly WS, Childs B, Kinzler KW, editors. New York: McGraw-Hill;2000. p. 1909–61.7. Yamaguchi S, Brailey LL, Morizono H, Bale AE, Tuchman M. Mutations and polymorphisms in the human ornithine transcarbamylase (OTC) gene. Hum Mutat. 2006; 27:626–32.
Article8. Arranz JA, Riudor E, Marco-Marín C, Rubio V. Estimation of the total number of disease-causing mutations in ornithine transcarbamylase (OTC) deficiency. Value of the OTC structure in predicting a mutation pathogenic potential. J Inherit Metab Dis. 2007; 30:217–26.
Article9. Wakiya T, Sanada Y, Mizuta K, Umehara M, Urahasi T, Egami S, et al. Living donor liver transplantation for ornithine transcarbamylase deficiency. Pediatr Transplant. 2011; 15:390–5.
Article10. Yorifuji T, Muroi J, Uematsu A, Tanaka K, Kiwaki K, Endo F, et al. X-inactivation pattern in the liver of a manifesting female with ornithine transcarbamylase (OTC) deficiency. Clin Genet. 1998; 54:349–53.
Article11. Gordon N. Ornithine transcarbamylase deficiency: a urea cycle defect. Eur J Paediatr Neurol. 2003; 7:115–21.
Article12. Häberle J, Boddaert N, Burlina A, Chakrapani A, Dixon M, Huemer M, et al. Suggested guidelines for the diagnosis and management of urea cycle disorders. Orphanet J Rare Dis. 2012; 7:32.
Article13. Chiu A, Tam S, Au WY, Chan SC, Liu CL, Fan ST. MARS treatment for a patient presenting with acquired hepatic glutamine synthetase deficiency after orthotopic liver transplantation. Liver Transpl. 2005; 11:353–5.
Article14. Busuttil AA, Goss JA, Seu P, Dulkanchainun TS, Yanni GS, McDiarmid SV, et al. The role of orthotopic liver transplantation in the treatment of ornithine transcarbamylase deficiency. Liver Transpl Surg. 1998; 4:350–4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acute treatment of hyperammonemia by continuous renal replacement therapy in a newborn patient with ornithine transcarbamylase deficiency
- CT and MR Imaging in 3 Patients with Hyperammonemia Due to Ornithine Transcarbamylase Deficiency
- A Case of Ornithine Transcarbamylase Deficiency Successfully Treated with Protein Restriction and Living Related Liver Transplantation
- A Case of Ornithine Transcarbamylase (OTC) Deficiency
- A Case of Molecular Diagnosis of Ornithine Transcarbamylase Deficiency