Korean J Crit Care Med.
2016 May;31(2):129-133. 10.4266/kjccm.2016.31.2.129.
Primary Invasive Intestinal Aspergillosis in a Non-Severely Immunocompromised Patient
- Affiliations
-
- 1Department of Critical Care Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. dr99.park@samsung.com
- 2Division of Pulmonary and Critical Care Medicine, Department of Medicine, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2350920
- DOI: http://doi.org/10.4266/kjccm.2016.31.2.129
Abstract
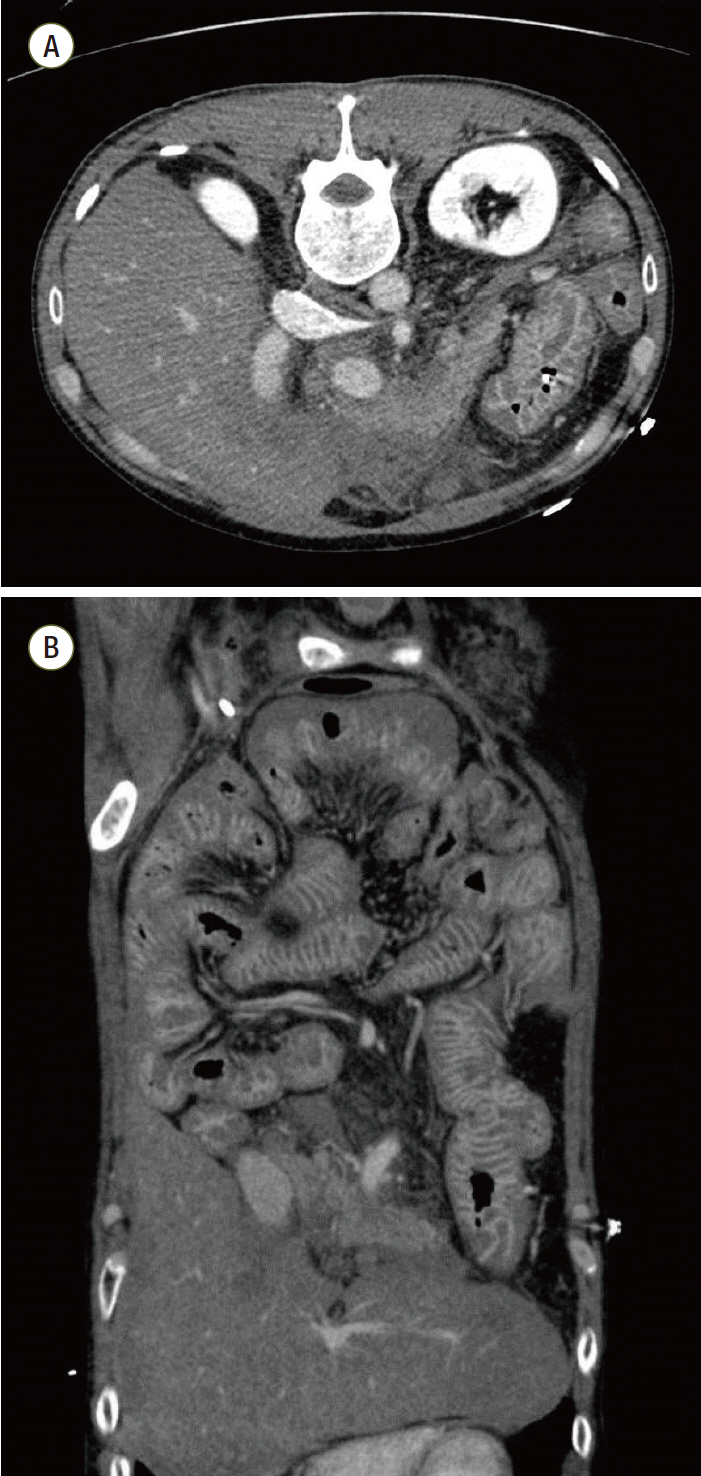
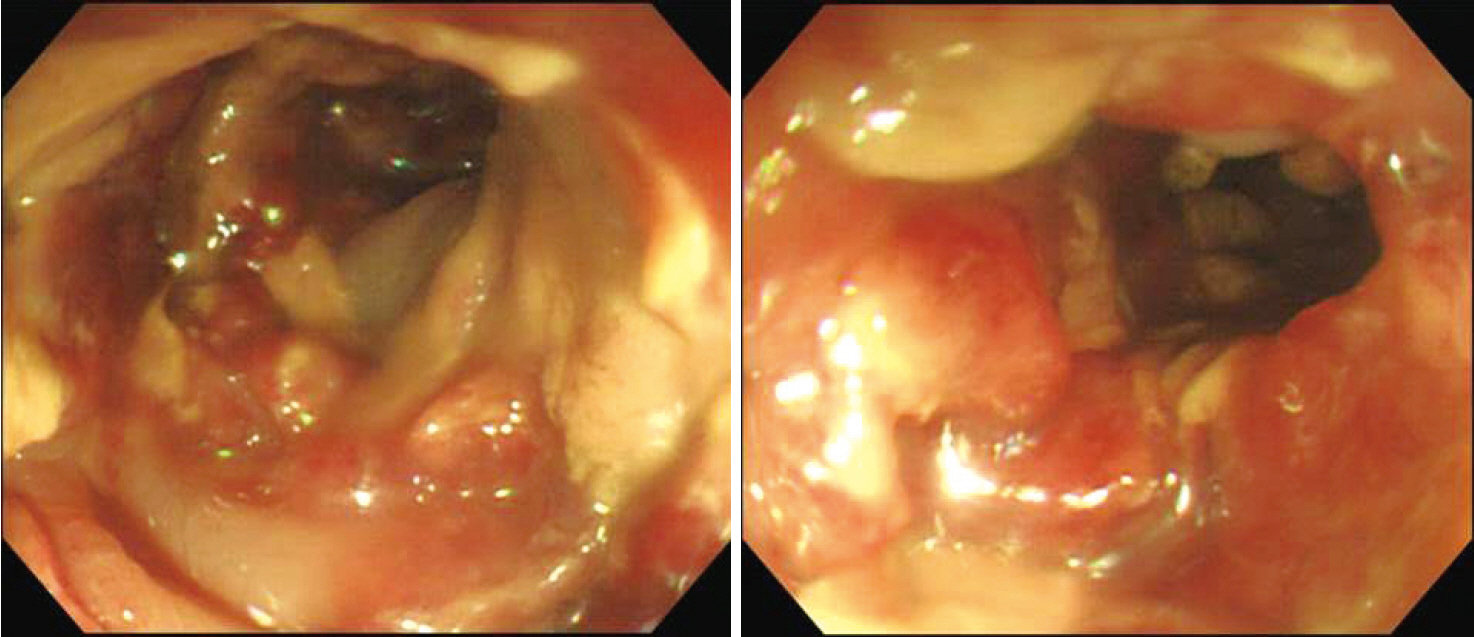
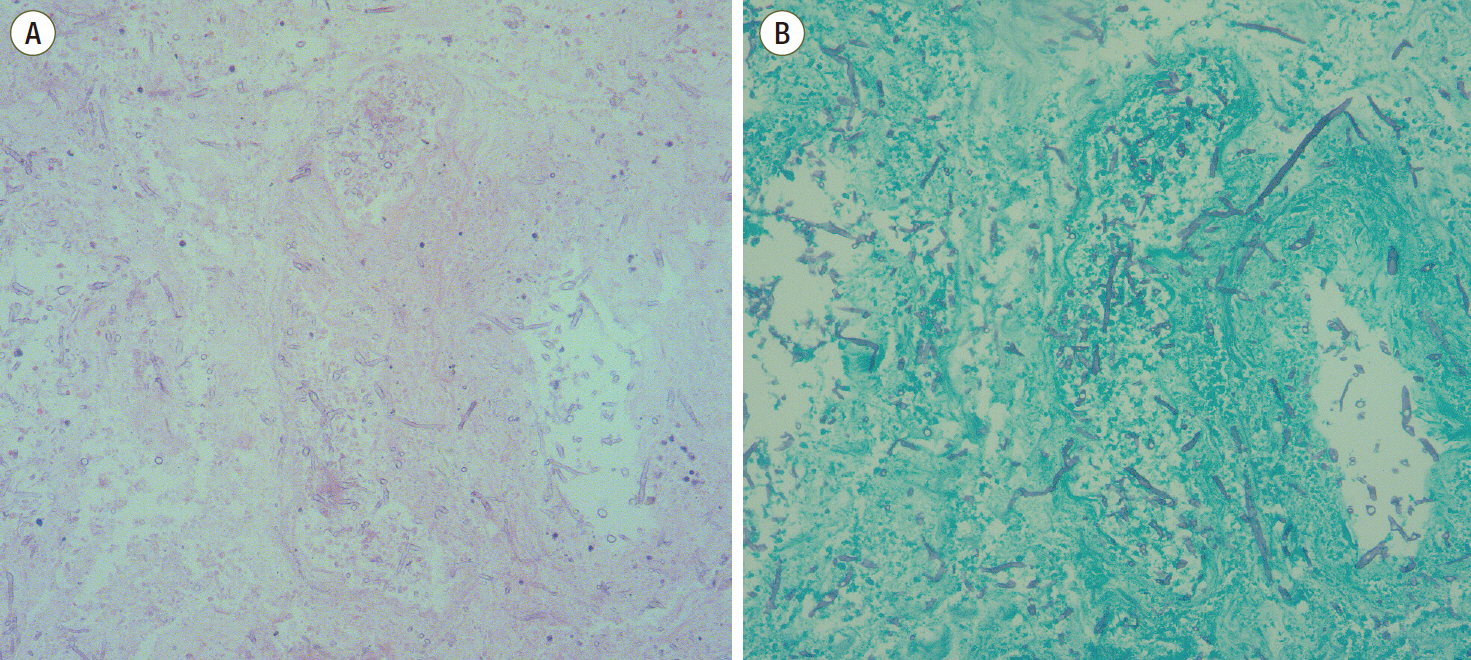
- Invasive aspergillosis (IA) is most commonly seen in patients with risk factors, such as cytotoxic chemotherapy, prolonged neutropenia, corticosteroids, transplantation and acquired immune deficiency syndrome. IA commonly occurs in the respiratory tract. Extrapulmonary aspergillosis is usually a part of a disseminated infection, and primary invasive intestinal aspergillosis is very rare. Herein, we report a case of an immunocompetent 53-year-old male who suffered recurrent septic shock in the intensive care unit (ICU) and was finally diagnosed as invasive intestinal aspergillosis without dissemination. IA is rarely considered for patients who do not have an immune disorder. Thus, when such cases do occur, the diagnosis is delayed and the clinical outcome is often poor. However, there is a growing literature reporting IA cases in patients without an immune disorder, mostly among ICU patients. Primary intestinal aspergillosis should be considered for critically ill patients, especially with severe disrupted gastrointestinal mucosal barrier.
MeSH Terms
Figure
Reference
-
References
1. Segal BH. Aspergillosis. N Engl J Med. 2009; 360:1870–84.
Article2. Meersseman W, Lagrou K, Maertens J, Van Wijngaerden E. Invasive aspergillosis in the intensive care unit. Clin Infect Dis. 2007; 45:205–16.
Article3. Clancy CJ, Nguyen MH. Acute community-acquired pneumonia due to Aspergillus in presumably immunocompetent hosts: clues for recognition of a rare but fatal disease. Chest. 1998; 114:629–34.4. Eggimann P, Chevrolet JC, Starobinski M, Majno P, Totsch M, Chapuis B, et al. Primary invasive aspergillosis of the digestive tract: report of two cases and review of the literature. Infection. 2006; 34:333–8.
Article5. Stevens DA, Melikian GL. Aspergillosis in the ‘nonimmunocompromised’ host. Immunol Invest. 2011; 40:751–66.
Article6. Cha SA, Kim MH, Lim TS, Kim HH, Chang KY, Park HS, et al. Invasive primary colonic Aspergillosis in the immunocompetent host without classical risk factors. Yonsei Med J. 2015; 56:1453–6.
Article7. Choi SH, Chung JW, Cho SY, Kim BJ, Kwon GY. A case of isolated invasive Aspergillus colitis presenting with hematochezia in a nonneutropenic patient with colon cancer. Gut Liver. 2010; 4:274–7.
Article8. Nivoix Y, Velten M, Letscher-Bru V, Moghaddam A, Natarajan-Amé S, Fohrer C, et al. Factors associated with overall and attributable mortality in invasive aspergillosis. Clin Infect Dis. 2008; 47:1176–84.
Article9. Hsu JL, Ruoss SJ, Bower ND, Lin M, Holodniy M, Stevens DA. Diagnosing invasive fungal disease in critically ill patients. Crit Rev Microbiol. 2011; 37:277–312.
Article10. Pfeiffer CD, Fine JP, Safdar N. Diagnosis of invasive aspergillosis using a galactomannan assay: a meta-analysis. Clin Infect Dis. 2006; 42:1417–27.
Article11. Sulahian A, Touratier S, Ribaud P. False positive test for Aspergillus antigenemia related to concomitant administration of piperacillin and tazobactam. N Engl J Med. 2003; 349:2366–7.
Article12. Kazan E, Maertens J, Herbrecht R, Weisser M, Gachot B, Vekhoff A, et al. A retrospective series of gut aspergillosis in haematology patients. Clin Microbiol Infect. 2011; 17:588–94.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Invasive Aspergillosis with Skin and Thyroid Gland Involvement
- A Case of Invasive Aspergillosis with Skin Involvement in a Renal Transplant Recipient
- A Case of Esophageal Aspergillosis Developed in Patient with Rheumatoid Arthritis
- Diagnosis and Treatment of Cutaneous Aspergillosis
- A Case of a 16-Year-Old Patient With Chronic Invasive Aspergillosis in the Trachea Treated With Segmental Tracheal Resection and Cricotracheal Anastomosis