Clin Endosc.
2016 Jul;49(4):332-335. 10.5946/ce.2016.069.
Treatment Strategy after Incomplete Endoscopic Resection of Early Gastric Cancer
- Affiliations
-
- 1Department of Internal Medicine and Liver Research Institute, Seoul National University College of Medicine, Seoul, Korea. harley1333@hanmail.net
- KMID: 2348250
- DOI: http://doi.org/10.5946/ce.2016.069
Abstract
- Endoscopic resection of early gastric cancer is defined as incomplete when tumor cells are found at the resection margin upon histopathological examination. However, a tumor-positive resection margin does not always indicate residual tumor; it can also be caused by tissue contraction during fixation, by the cautery effect during endoscopic resection, or by incorrect histopathological mapping. Cases of highly suspicious residual tumor require additional endoscopic or surgical resection. For inoperable patients, argon plasma coagulation can be used as an alternative endoscopic treatment. Immediately after the incomplete resection or residual tumor has been confirmed by the pathologist, clinicians should also decide upon any additional treatment to be carried out during the follow-up period.
MeSH Terms
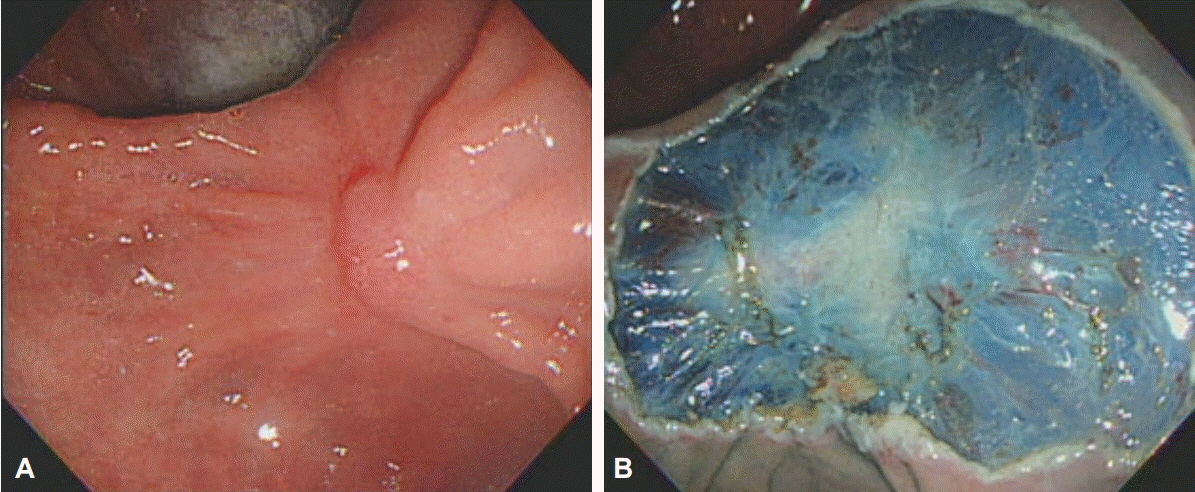
Figure
Cited by 1 articles
-
Risk Factors and Clinical Outcomes of Non-Curative Resection in Patients with Early Gastric Cancer Treated with Endoscopic Submucosal Dissection: A Retrospective Multicenter Study in Korea
Si Hyung Lee, Min Cheol Kim, Seong Woo Jeon, Kang Nyeong Lee, Jong Jae Park, Su Jin Hong
Clin Endosc. 2020;53(2):196-205. doi: 10.5946/ce.2019.123.
Reference
-
1. Kitamura K, Yamaguchi T, Okamoto K, et al. Clinicopathologic features of synchronous multifocal early gastric cancers. Anticancer Res. 1997; 17(1B):643–646.2. Gotoda T, Yanagisawa A, Sasako M, et al. Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer. 2000; 3:219–225.
Article3. Oda I, Gotoda T, Sasako M, et al. Treatment strategy after non-curative endoscopic resection of early gastric cancer. Br J Surg. 2008; 95:1495–1500.
Article4. Lee JH, Kim JH, Kim DH, et al. Is surgical treatment necessary after non-curative endoscopic resection for early gastric cancer? J Gastric Cancer. 2010; 10:182–187.
Article5. Nagano H, Ohyama S, Fukunaga T, et al. Indications for gastrectomy after incomplete EMR for early gastric cancer. Gastric Cancer. 2005; 8:149–154.
Article6. Song KY, Hyung WJ, Kim HH, et al. Is gastrectomy mandatory for all residual or recurrent gastric cancer following endoscopic resection? A large-scale Korean multi-center study. J Surg Oncol. 2008; 98:6–10.
Article7. Kim TK, Kim GH, Park do Y, et al. Risk factors for local recurrence in patients with positive lateral resection margins after endoscopic submucosal dissection for early gastric cancer. Surg Endosc. 2015; 29:2891–2898.
Article8. Hwang JJ, Park KJ, Park YS, et al. A scoring system for patients with a tumor-positive lateral resection margin after endoscopic resection of early gastric cancer. Surg Endosc. 2016; 30:2751–2758.
Article9. Lee JH, Lee JH, Kim KM, Kang KJ, Min BH, Kim JJ. Clinicopathological factors of multiple lateral margin involvement after endoscopic submucosal dissection for early gastric cancer. Surg Endosc. 2015; 29:3460–3468.
Article10. Sekiguchi M, Suzuki H, Oda I, et al. Risk of recurrent gastric cancer after endoscopic resection with a positive lateral margin. Endoscopy. 2014; 46:273–278.
Article11. Yoon H, Kim SG, Choi J, et al. Risk factors of residual or recurrent tumor in patients with a tumor-positive resection margin after endoscopic resection of early gastric cancer. Surg Endosc. 2013; 27:1561–1568.
Article12. Soetikno R, Kaltenbach T, Yeh R, Gotoda T. Endoscopic mucosal resection for early cancers of the upper gastrointestinal tract. J Clin Oncol. 2005; 23:4490–4498.
Article13. Miyata M, Yokoyama Y, Okoyama N, et al. What are the appropriate indications for endoscopic mucosal resection for early gastric cancer? Analysis of 256 endoscopically resected lesions. Endoscopy. 2000; 32:773–778.
Article14. Abe N, Sugiyama M, Masaki T, et al. Predictive factors for lymph node metastasis of differentiated submucosally invasive gastric cancer. Gastrointest Endosc. 2004; 60:242–245.
Article15. Yokota T, Ishiyama S, Saito T, et al. Lymph node metastasis as a significant prognostic factor in gastric cancer: a multiple logistic regression analysis. Scand J Gastroenterol. 2004; 39:380–384.
Article16. Kang HY, Kim SG, Kim JS, Jung HC, Song IS. Clinical outcomes of endoscopic submucosal dissection for undifferentiated early gastric cancer. Surg Endosc. 2010; 24:509–516.
Article17. Ryu KW, Choi IJ, Doh YW, et al. Surgical indication for non-curative endoscopic resection in early gastric cancer. Ann Surg Oncol. 2007; 14:3428–3434.
Article18. Noh H, Park JJ, Yun JW, et al. Clinicopathologic characteristics of patients who underwent curative additional gastrectomy after endoscopic submucosal dissection for early gastric cancer or adenoma. Korean J Gastroenterol. 2012; 59:289–295.
Article19. Choi JY, Jeon SW, Cho KB, et al. Non-curative endoscopic resection does not always lead to grave outcomes in submucosal invasive early gastric cancer. Surg Endosc. 2015; 29:1842–1849.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Resection of Undifferentiated Early Gastric Cancer
- Endoscopic Resection of Early Gastric Cancer in Korea: Recent Results and Future Directions
- Endoscopic Treatment for Early Gastric Cancer
- Endoscopic Resection for Early Gastric Cancer beyond Absolute Indication with Emphasis on Controversial Issues
- Endoscopic Resection of Early Gastric Cancer