Restor Dent Endod.
2016 Aug;41(3):210-217. 10.5395/rde.2016.41.3.210.
Esthetic enhancement of a traumatized anterior tooth with a combination of forced eruption and tooth alignment: a case report
- Affiliations
-
- 1Department of Conservative Dentistry, Kyungpook National University School of Dentistry, Daegu, Korea. wisekim@knu.ac.kr
- KMID: 2346770
- DOI: http://doi.org/10.5395/rde.2016.41.3.210
Abstract
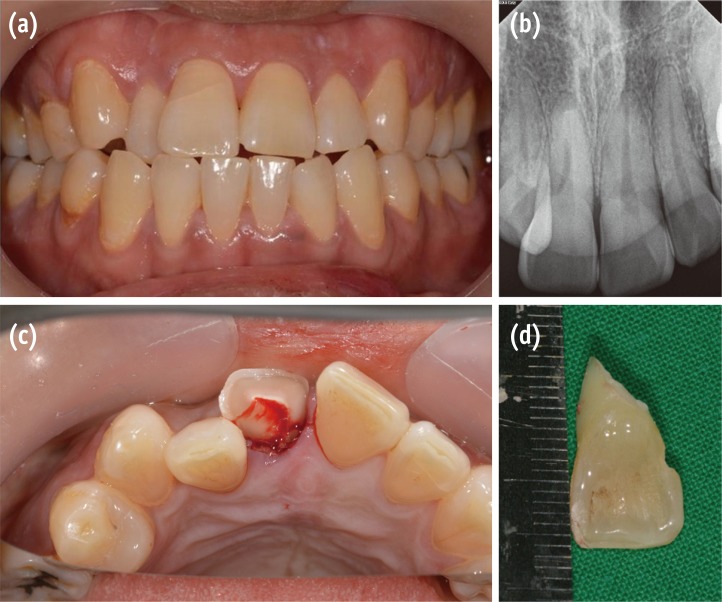
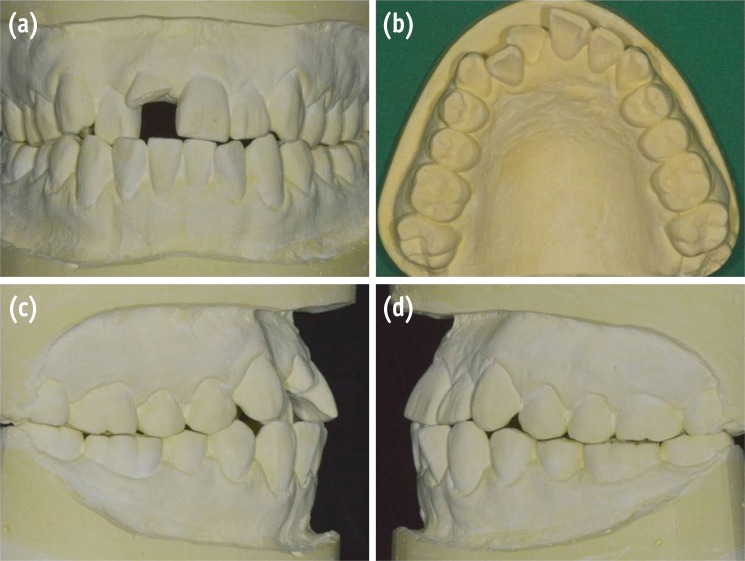
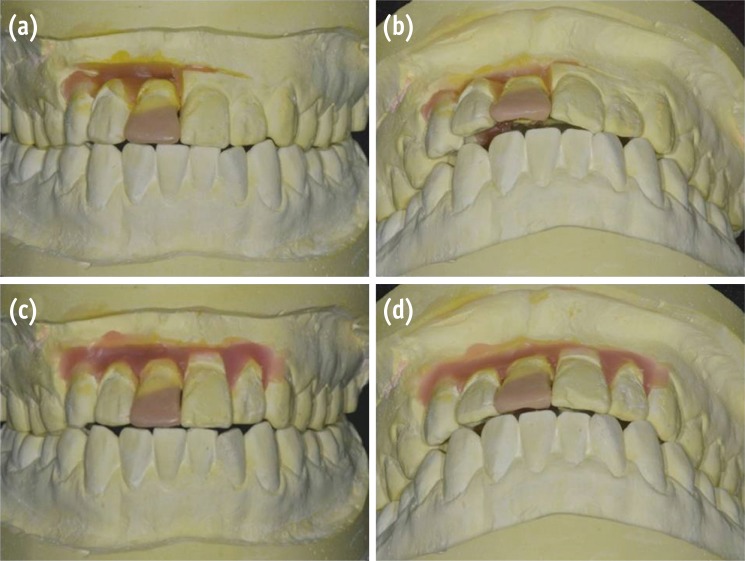
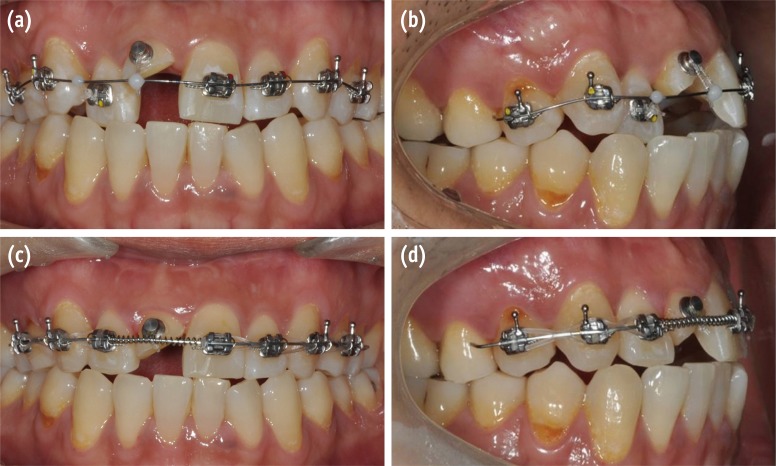
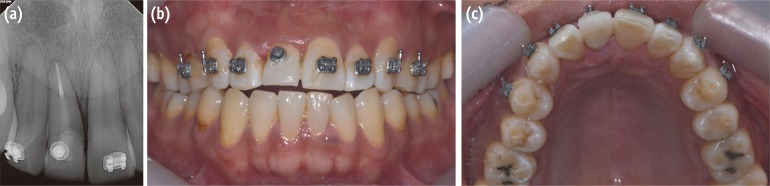
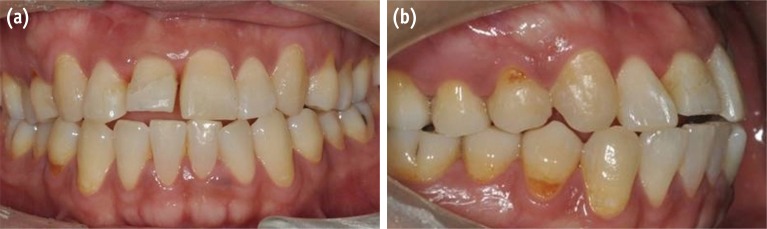
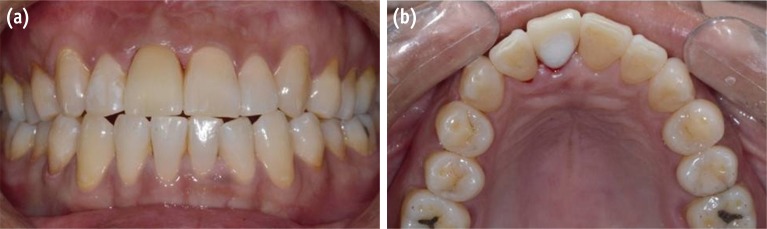
- Exposing sound structure of a subgingivally fractured tooth using orthodontic extrusion is considered to be a conservative way to re-establish biologic width without sacrificing esthetics or jeopardizing periodontal support of neighboring teeth. When a misaligned tooth is traumatically involved, a more comprehensive approach combining tooth extrusion and re-alignment may be necessary for a successful restorative outcome. This case report describes a successful esthetic management of a patient with complicated crown-root fracture on the maxillary right central incisor and pre-existing malocclusion in the maxillary anterior region. Forced eruption along with re-alignment of teeth by orthodontic movement seems to allow re-positioning of the fracture line to a favorable position and correction of crowding, providing a better esthetic result.
Keyword
Figure
Reference
-
1. Olsburgh S, Jacoby T, Krejci I. Crown fractures in the permanent dentition: pulpal and restorative considerations. Dent Traumatol. 2002; 18:103–115. PMID: 12110103.
Article2. Jeon SM, Lee KH, Jung BY. An esthetic appliance for the management of crown-root fracture: a case report. Restor Dent Endod. 2014; 39:226–229. PMID: 25110648.
Article3. Durham TM, Goddard T, Morrison S. Rapid forced eruption: a case report and review of forced eruption techniques. Gen Dent. 2004; 52:167–175. PMID: 15101313.4. Proffit WR, Fields HW Jr, Sarver DM. Contemporary orthodontics. 5th ed. St. Louis: Mosby Elsevier;2012. p. 368.5. van der Linden FPGM, Duterloo HS. Development of the human dentition: an atlas. Hagerstown: Harper & Row;2013. p. 217.6. Andreasen JO, Andreasen FM, Andersson L. Textbook and Color Atlas of Traumatic Injuries to the Teeth. 4th ed. Oxford: Wiley-Blackwell;2007. p. 671.7. Rossouw PE, Tortorella A. Enamel reduction procedures in orthodontic treatment. J Can Dent Assoc. 2003; 69:378–383. PMID: 12787475.8. ellini-Ferreira F, Cotrim-Ferreira FA, Ribeiro JA, Ferreira-Santos RI. Mapping of proximal enamel thickness in permanent teeth. Braz J Oral Sci. 2012; 11:481–485.9. Twesme DA, Firestone AR, Heaven TJ, Feagin FF, Jacobson A. Air-rotor stripping and enamel demineralization in vitro. Am J Orthod Dentofacial Orthop. 1994; 105:142–152. PMID: 8311036.10. Danesh G, Hellak A, Lippold C, Ziebura T, Schafer E. Enamel surfaces following interproximal reduction with different methods. Angle Orthod. 2007; 77:1004–1010. PMID: 18004908.
Article11. Rogers GA, Wagner MJ. Protection of stripped enamel surface with topical fluoride applications. Am J Orthod. 1969; 56:551–559. PMID: 4900287.12. Johnson GK, Sivers JE. Forced eruption in crown-lengthening procedures. J Prosthet Dent. 1986; 56:424–427. PMID: 3531482.
Article13. Guimarães GS, de Morais LS, de Souza MM, Elias CN. Superficial morphology and mechanical properties of in vivo aged orthodontic ligatures. Dental Press J Orthod. 2013; 18:107–112. PMID: 24094019.14. Son MK, Jang HS. Gingival recontouring by provisional implant restoration for optimal emergence profile: report of two cases. J Periodontal Implant Sci. 2011; 41:302–308. PMID: 22324008.
Article15. Nam J, Aranyarachkul P. Achieving the optimal peri-implant soft tissue profile by the selective pressure method via provisional restorations in the esthetic zone. J Esthet Restor Dent. 2015; 27:136–144. PMID: 25968909.
Article16. Seixas MR, Costa-Pinto RA, de Araújo TM. Gingival esthetics: an orthodontic and periodontal approach. Dent Press J Orthod. 2012; 17:190–201.
Article17. Bach N, Baylard JF, Voyer R. Orthodontic extrusion: periodontal considerations and applications. J Can Dent Assoc. 2004; 70:775–780. PMID: 15588553.18. Palomo F, Kopczyk RA. Rationale and methods for crown lengthening. J Am Dent Assoc. 1978; 96:257–260. PMID: 272411.
Article19. Lythgoe JR, Torabinejad M, Simon JH. Extrusion techniques for the general dentist. Gen Dent. 1980; 28:42–43. 46–49. PMID: 6935146.20. Berglundh T, Marinello CP, Lindhe J, Thilander B, Liljenberg B. Periodontal tissue reactions to orthodontic extrusion. An experimental study in the dog. J Clin Periodontol. 1991; 18:330–336. PMID: 2066448.
Article21. al Yami EA, Kuijpers-Jagtman AM, van't Hof MA. Occlusal outcome of orthodontic treatment. Angle Orthod. 1998; 68:439–444. PMID: 9770102.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prosthetic restoration of the maxillary anterior teeth using implantation and forced eruption: Case report
- Conservative approach for anterior crown-root fractured teeth: forced eruption
- Anterior esthetic improvement through orthodontic extrusive remodeling and single-unit implantation in a fractured upper lateral incisor with alveolar bone loss: A case report
- The treatment of an ankylosed canine: Luxation and forced eruption
- Effect of slow forced eruption on the vertical levels of the interproximal bone and papilla and the width of the alveolar ridge