Yonsei Med J.
2015 Nov;56(6):1538-1544. 10.3349/ymj.2015.56.6.1538.
Impact of Coronary Plaque Characteristics on Late Stent Malapposition after Drug-Eluting Stent Implantation
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea.
- 2Division of Cardiology, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea. mkhong61@yuhs.ac
- 3Cardiovascular Institute, Yonsei University College of Medicine, Seoul, Korea.
- 4Severance Biomedical Science Institute, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2345880
- DOI: http://doi.org/10.3349/ymj.2015.56.6.1538
Abstract
- PURPOSE
To evaluate the impact of pre-procedural coronary plaque composition assessed by virtual histology intravascular ultrasound (VH-IVUS) on late stent malapposition assessed by optical coherence tomography (OCT) following drug-eluting stent (DES) implantation.
MATERIALS AND METHODS
The study population consisted of 121 patients (121 lesions) who underwent both pre-procedural VH-IVUS and follow-up OCT after DES implantation. The association between pre-procedural plaque composition [necrotic core (NC), dense calcium (DC), fibrotic (FT), and fibro-fatty (FF) volumes] assessed by VH-IVUS and late stent malapposition (percent malapposed struts) or strut coverage (percent uncovered struts) assessed by follow-up OCT was evaluated.
RESULTS
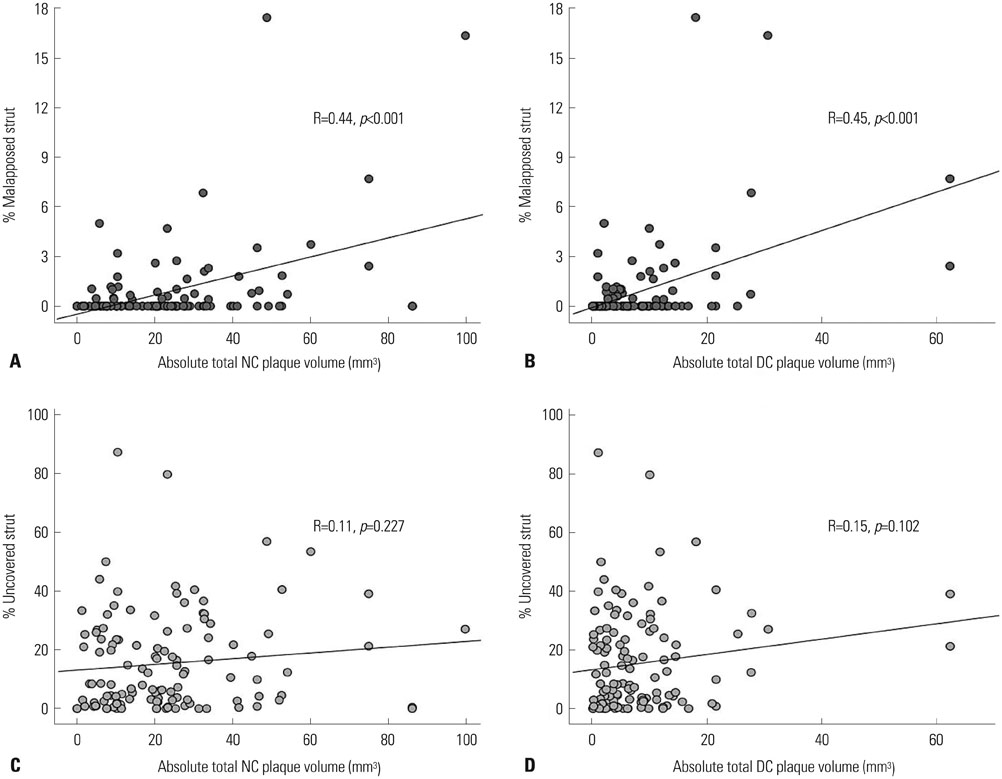
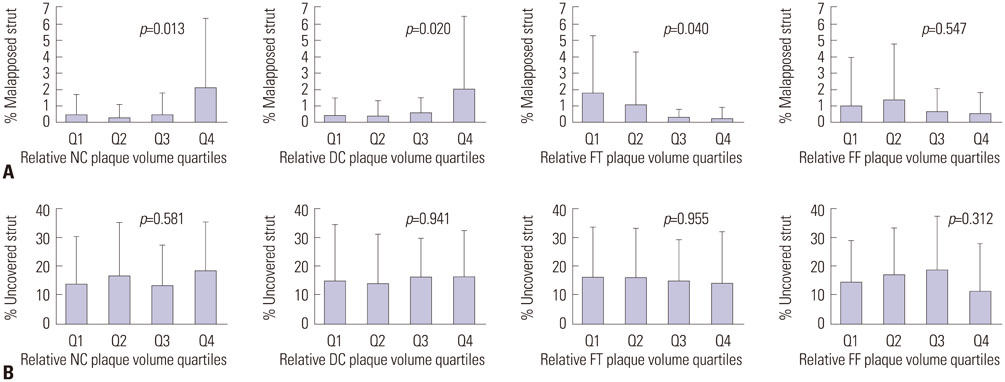
Pre-procedural absolute total NC, DC, FT, and FF plaque volumes were 22.9+/-19.0, 7.9+/-9.6, 63.8+/-33.8, and 16.5+/-12.4 mm3, respectively. At 6.3+/-3.1 months post-intervention, percent malapposed and uncovered struts were 0.8+/-2.5% and 15.3+/-16.7%, respectively. Pre-procedural absolute total NC and DC plaque volumes were positively correlated with percent malapposed struts (r=0.44, p<0.001 and r=0.45, p<0.001, respectively), while pre-procedural absolute total FT plaque volume was weakly associated with percent malapposed struts (r=0.220, p=0.015). Pre-procedural absolute total DC plaque volume was the only independent predictor of late stent malapposition on multivariate analysis (beta=1.12, p=0.002). There were no significant correlations between pre-intervention plaque composition and percent uncovered struts.
CONCLUSION
Pre-procedural plaque composition was associated with late stent malapposition but not strut coverage after DES implantation. Larger pre-procedural absolute total DC plaque volumes were associated with greater late stent malapposition.
MeSH Terms
Figure
Reference
-
1. Cook S, Wenaweser P, Togni M, Billinger M, Morger C, Seiler C, et al. Incomplete stent apposition and very late stent thrombosis after drug-eluting stent implantation. Circulation. 2007; 115:2426–2434.
Article2. Siqueira DA, Abizaid AA, Costa Jde R, Feres F, Mattos LA, Staico R, et al. Late incomplete apposition after drug-eluting stent implantation: incidence and potential for adverse clinical outcomes. Eur Heart J. 2007; 28:1304–1309.
Article3. Hassan AK, Bergheanu SC, Stijnen T, van der Hoeven BL, Snoep JD, Plevier JW, et al. Late stent malapposition risk is higher after drug-eluting stent compared with bare-metal stent implantation and associates with late stent thrombosis. Eur Heart J. 2010; 31:1172–1180.
Article4. Guagliumi G, Sirbu V, Musumeci G, Gerber R, Biondi-Zoccai G, Ikejima H, et al. Examination of the in vivo mechanisms of late drug-eluting stent thrombosis: findings from optical coherence tomography and intravascular ultrasound imaging. JACC Cardiovasc Interv. 2012; 5:12–20.
Article5. Won H, Shin DH, Kim BK, Mintz GS, Kim JS, Ko YG, et al. Optical coherence tomography derived cut-off value of uncovered stent struts to predict adverse clinical outcomes after drug-eluting stent implantation. Int J Cardiovasc Imaging. 2013; 29:1255–1263.
Article6. Im E, Kim BK, Ko YG, Shin DH, Kim JS, Choi D, et al. Incidences, predictors, and clinical outcomes of acute and late stent malap-position detected by optical coherence tomography after drug-eluting stent implantation. Circ Cardiovasc Interv. 2014; 7:88–96.
Article7. Kim BK, Kim JS, Oh C, Ko YG, Choi D, Jang Y, et al. Major determinants for the uncovered stent struts on optical coherence tomography after drug-eluting stent implantation. Int J Cardiovasc Imaging. 2012; 28:705–714.
Article8. Guo N, Maehara A, Mintz GS, He Y, Xu K, Wu X, et al. Incidence, mechanisms, predictors, and clinical impact of acute and late stent malapposition after primary intervention in patients with acute myocardial infarction: an intravascular ultrasound substudy of the Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction (HORIZONS-AMI) trial. Circulation. 2010; 122:1077–1084.
Article9. Gutiérrez-Chico JL, Wykrzykowska J, Nüesch E, van Geuns RJ, Koch KT, Koolen JJ, et al. Vascular tissue reaction to acute malap-position in human coronary arteries: sequential assessment with optical coherence tomography. Circ Cardiovasc Interv. 2012; 5:20–29.
Article10. Ozaki Y, Okumura M, Ismail TF, Naruse H, Hattori K, Kan S, et al. The fate of incomplete stent apposition with drug-eluting stents: an optical coherence tomography-based natural history study. Eur Heart J. 2010; 31:1470–1476.
Article11. Mintz GS, Nissen SE, Anderson WD, Bailey SR, Erbel R, Fitzgerald PJ, et al. American College of Cardiology Clinical Expert Consensus Document on Standards for Acquisition, Measurement and Reporting of Intravascular Ultrasound Studies (IVUS). A report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2001; 37:1478–1492.
Article12. Nair A, Kuban BD, Tuzcu EM, Schoenhagen P, Nissen SE, Vince DG. Coronary plaque classification with intravascular ultrasound radiofrequency data analysis. Circulation. 2002; 106:2200–2206.
Article13. Nasu K, Tsuchikane E, Katoh O, Vince DG, Virmani R, Surmely JF, et al. Accuracy of in vivo coronary plaque morphology assessment: a validation study of in vivo virtual histology compared with in vitro histopathology. J Am Coll Cardiol. 2006; 47:2405–2412.14. Takano M, Inami S, Jang IK, Yamamoto M, Murakami D, Seimiya K, et al. Evaluation by optical coherence tomography of neointimal coverage of sirolimus-eluting stent three months after implantation. Am J Cardiol. 2007; 99:1033–1038.
Article15. Barlis P, Dimopoulos K, Tanigawa J, Dzielicka E, Ferrante G, Del Furia F, et al. Quantitative analysis of intracoronary optical coherence tomography measurements of stent strut apposition and tissue coverage. Int J Cardiol. 2010; 141:151–156.
Article16. Kim BK, Hong MK, Shin DH, Kim JS, Ko YG, Choi D, et al. Optical coherence tomography analysis of strut coverage in biolimus- and sirolimus-eluting stents: 3-month and 12-month serial follow-up. Int J Cardiol. 2013; 168:4617–4623.
Article17. Kim BK, Ha J, Mintz GS, Kim JS, Shin DH, Ko YG, et al. Randomised comparison of strut coverage between Nobori biolimus-eluting and sirolimus-eluting stents: an optical coherence tomography analysis. EuroIntervention. 2014; 9:1389–1397.
Article18. Tanigawa J, Barlis P, Dimopoulos K, Dalby M, Moore P, Di Mario C. The influence of strut thickness and cell design on immediate apposition of drug-eluting stents assessed by optical coherence tomography. Int J Cardiol. 2009; 134:180–188.
Article19. Davlouros PA, Mavronasiou E, Xanthopoulou I, Karantalis V, Tsigkas G, Hahalis G, et al. An optical coherence tomography study of two new generation stents with biodegradable polymer carrier, eluting paclitaxel vs. biolimus-A9. Int J Cardiol. 2012; 157:341–346.
Article20. Hong MK, Mintz GS, Lee CW, Park DW, Park KM, Lee BK, et al. Late stent malapposition after drug-eluting stent implantation: an intravascular ultrasound analysis with long-term follow-up. Circulation. 2006; 113:414–419.
Article21. Ako J, Morino Y, Honda Y, Hassan A, Sonoda S, Yock PG, et al. Late incomplete stent apposition after sirolimus-eluting stent implantation: a serial intravascular ultrasound analysis. J Am Coll Cardiol. 2005; 46:1002–1005.
Article22. Hong YJ, Jeong MH, Choi YH, Song JA, Jang SY, Yoo JH, et al. Relation between poststenting peristent plaque components and late stent malapposition after drug-eluting stent implantation: virtual histology-intravascular ultrasound analysis. Int J Cardiol. 2013; 167:1882–1887.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Late Stent Thrombosis Associated with Late Stent Malapposition after Drug-Eluting Stenting: A Case Report
- Very Late Stent Thrombosis Related to Fracture of a Sirolimus-Eluting Stent
- Long-term Clinical Outcomes of DrugEluting Stent Malapposition
- A Case of Stent Strut Fracture of a Paclitaxel-Eluting Stent at the Time of Stent Implantation in a Complex Coronary Lesion
- A Case of Extremely Very Late Stent Thrombosis 8 Years after Implantation of Drug-Eluting Stent Observed by Intravascular Ultrasound