Korean J Ophthalmol.
2014 Dec;28(6):486-492. 10.3341/kjo.2014.28.6.486.
Introduction of Lens-angle Reconstruction Surgery in Rabbit Eyes
- Affiliations
-
- 1Department of Ophthalmology and Visual Science, Seoul St. Mary's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea. ckjoo@catholic.ac.kr
- 2Department of Ophthalmology, Chuncheon Sacred Heart Hospital, Hallym University College of Medicine, Chuncheon, Korea.
- 3St. Mary's Eye Center, Seoul, Korea.
- 4Department of Ophthalmology, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea.
- KMID: 2345826
- DOI: http://doi.org/10.3341/kjo.2014.28.6.486
Abstract
- PURPOSE
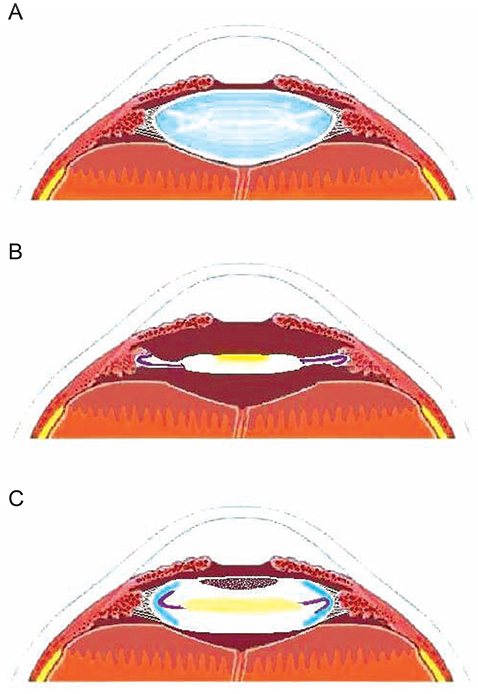
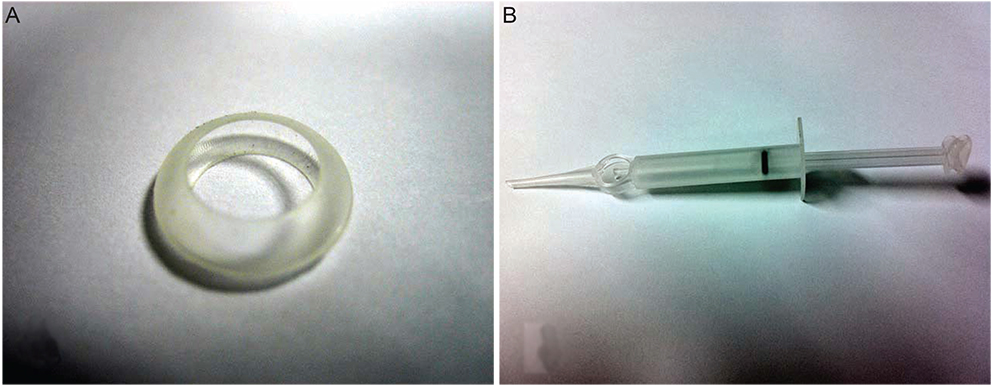
In this study, we examined the stability of the lens-angle supporter (LAS) for accommodation restoration by comparing intraocular lens (IOL) location, after-cataract and ciliary body damage after cataract surgery in rabbits.
METHODS
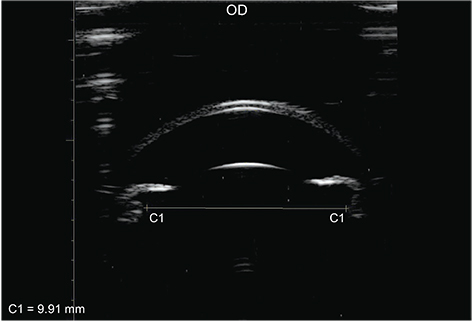
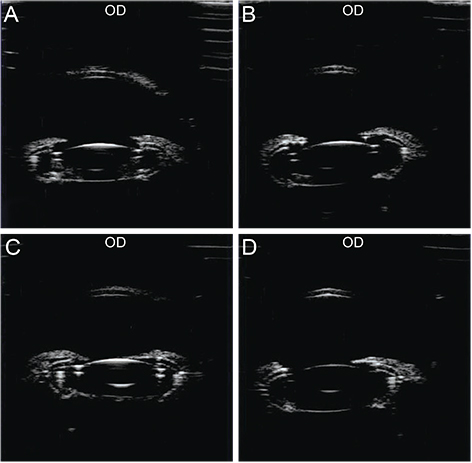
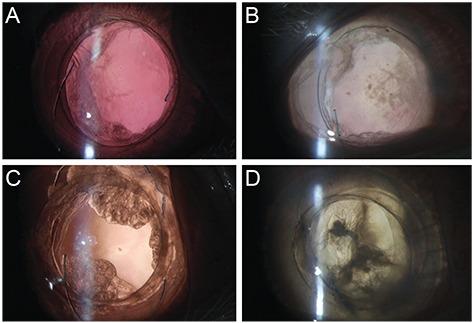
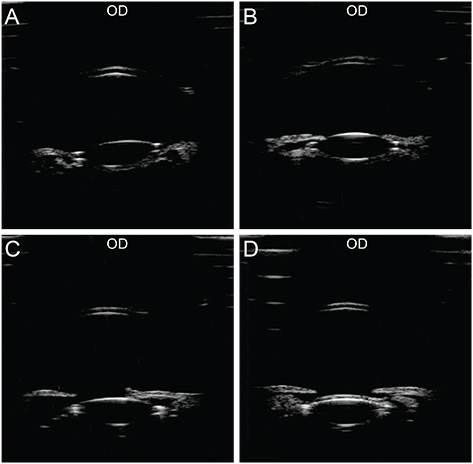
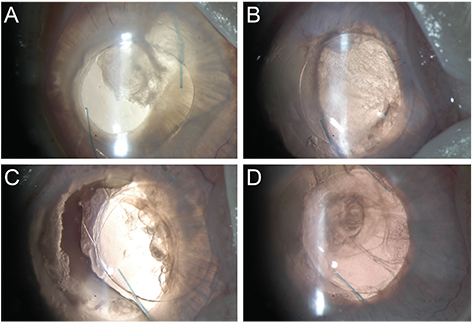
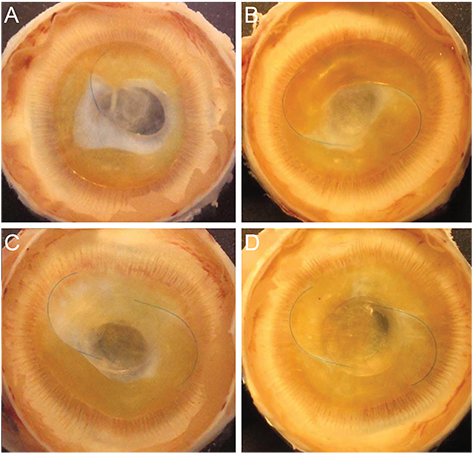
Eight rabbits were divided into experimental and control groups of four rabbits each. Phacoemulsification and irrigation and aspiration were performed in all rabbits. This was followed by an LAS and IOL insertion in the four experimental rabbits. In the four control rabbits, only an IOL insertion was performed. Six months after the surgery, the location of the IOL, the conditions of the lens capsule and ciliary body were evaluated using a slitl-amp examination and Miyake-Apple view.
RESULTS
For the experimental group, the ultrasound biomicroscope results showed normal LAS and IOL positioning in all four cases. According to the slitlamp examination and Miyake-Apple view, the IOL was positioned at the center, with less after-cataract and damage to the ciliary body. For the control group, ultrasound biomicroscope results indicated a higher IOL position than normal, as well as a single case of IOL decentering. According to the slit-lamp examination and Miyake-Apple view, the IOL was decentered with more severe after-cataract and ciliary body damage.
CONCLUSIONS
The LAS has the potential to maintain a stable IOL position while producing less after-cataract when used in lens-angle reconstruction for correction of presbyopia. Moreover, LAS implantation incurs less damage to the ciliary body.
Keyword
MeSH Terms
Figure
Reference
-
1. Schachar RA. The mechanism of accommodation and presbyopia. Int Ophthalmol Clin. 2006; 46:39–61.2. Baumeister M, Kohnen T. Accommodation and presbyopia. Part 1: physiology of accommodation and development of presbyopia. Ophthalmologe. 2008; 105:597–608.3. Croft MA, Kaufman PL. Accommodation and presbyopia: the ciliary neuromuscular view. Ophthalmol Clin North Am. 2006; 19:13–24.4. Modesti M, Pasqualitto G, Appolloni R, et al. Preoperative and postoperative size and movements of the lens capsular bag: ultrasound biomicroscopy analysis. J Cataract Refract Surg. 2011; 37:1775–1784.5. Salcan I, Aykan U, Yildirim O, Kanik A. Quantitative ultrasound biomicroscopy study of biometry of the lens and anterior chamber. Eur J Ophthalmol. 2012; 22:349–355.6. Pereira FA, Werner L, Milverton EJ, Coroneo MT. Miyake-Apple posterior video analysis/photographic technique. J Cataract Refract Surg. 2009; 35:577–587.7. Klaproth OK, Titke C, Baumeister M, Kohnen T. Accommodative intraocular lenses: principles of clinical evaluation and current results. Klin Monbl Augenheilkd. 2011; 228:666–675.8. Mesci C, Erbil H, Ozdoker L, et al. Visual acuity and contrast sensitivity function after accommodative and multifocal intraocular lens implantation. Eur J Ophthalmol. 2010; 20:90–100.9. Alio JL, Ben-nun J, Rodriguez-Prats JL, Plaza AB. Visual and accommodative outcomes 1 year after implantation of an accommodating intraocular lens based on a new concept. J Cataract Refract Surg. 2009; 35:1671–1678.10. Marchini G, Mora P, Pedrotti E, et al. Functional assessment of two different accommodative intraocular lenses compared with a monofocal intraocular lens. Ophthalmology. 2007; 114:2038–2043.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Experimental Studies on the Artificial Anterior Chamber Lens
- Phacoemulsification using Iris Hook in Patients with Secondary Angle-Closure Glaucoma Associated with Lens Subluxation
- Influence of Lens Factor and Effect of Selected Cataract Extraction on Acute Angle-Closure Glaucoma
- Biometric Measurements in Acute Angle Closure Glaucoma
- Long-Term Endothelial Cell Changes after Angle-Supported Anterior Chamber Lens Implantation in Phakic Eyes