Korean Circ J.
2016 Mar;46(2):246-255. 10.4070/kcj.2016.46.2.246.
Complications of Cardiac Catheterization in Structural Heart Disease
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Children's Hospital, Seoul, Korea. ped9526@snu.ac.kr
- 2Department of Pediatrics, Seoul National University Boramae Hospital, Seoul, Korea.
- 3Department of Pediatrics, Bundang Seoul National University Hospital, Seongnam, Korea.
- KMID: 2344477
- DOI: http://doi.org/10.4070/kcj.2016.46.2.246
Abstract
- BACKGROUND AND OBJECTIVES
Cardiac catheterization is used to diagnose structural heart disease (SHD) and perform transcatheter treatment. This study aimed to evaluate complications of cardiac catheterization and the associated risk factors in a tertiary center over 10 years.
SUBJECTS AND METHODS
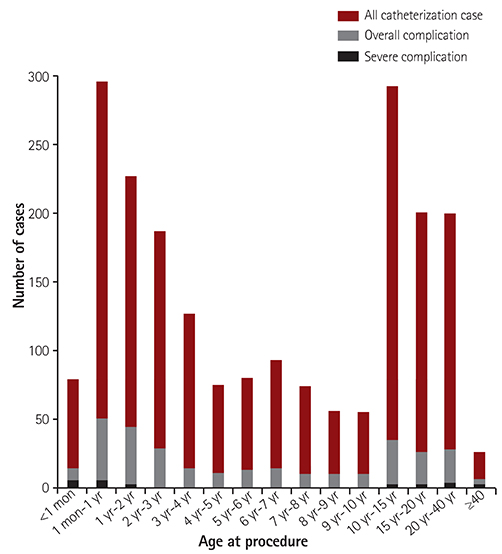
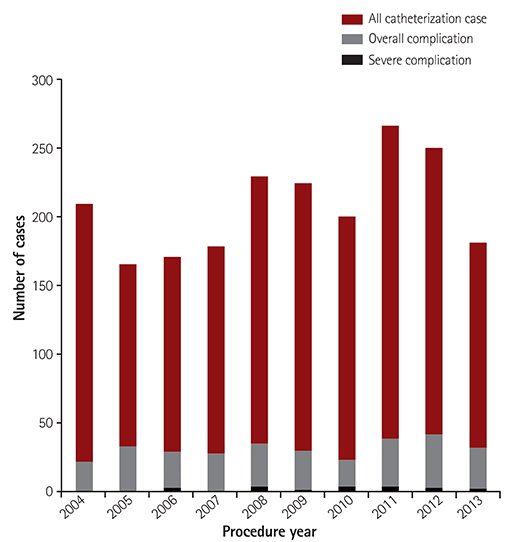
Total 2071 cardiac catheterizations performed at the Seoul National University Children's Hospital from January 2004 to December 2013 were included in this retrospective study.
RESULTS
The overall complication, severe complication, and mortality rates were 16.2%, 1.15%, and 0.19%, respectively. The factors that significantly increased the risk of overall and severe complications were anticoagulant use before procedure (odds ratio [OR] 1.83, p=0.012 and OR 6.45, p<0.001, respectively), prothrombin time (OR 2.30, p<0.001 and OR 5.99, p<0.001, respectively), general anesthesia use during procedure (OR 1.84, p=0.014 and OR 5.31, p=0.015, respectively), and total procedure time (OR 1.01, p<0.001 and OR 1.02, p<0.001, respectively). Low body weight (OR 0.99, p=0.003), severe SHD (OR 1.37, p=0.012), repetitive procedures (OR 1.7, p=0.009), and total fluoroscopy time (OR 1.01, p=0.005) significantly increased the overall complication risk. High activated partial thromboplastin time (OR 1.04, p=0.001), intensive care unit admission state (OR 14.03, p<0.001), and concomitant electrophysiological study during procedure (OR 3.41, p=0.016) significantly increased severe complication risk.
CONCLUSION
Currently, the use of cardiac catheterization in SHD is increasing and becoming more complex; this could cause complications despite the preventive efforts. Careful patient selection for therapeutic catheterization and improved technique and management during the peri-procedural period are required to reduce complications.
Keyword
MeSH Terms
Figure
Reference
-
1. Kim GB. Psychosocial adjustment and quality of life of adolescents and adults with congenital heart disease. Korean J Pediatr. 2014; 57:257–263.2. Mehta R, Lee KJ, Chaturvedi R, Benson L. Complications of pediatric cardiac catheterization: a review in the current era. Catheter Cardiovasc Interv. 2008; 72:278–285.3. Porter CJ, Gillette PC, Mullins CE, McNamara DG. Cardiac catheterization in the neonate. A comparison of three techniques. J Pediatr. 1978; 93:97–101.4. Booth P, Redington AN, Shinebourne EA, Rigby ML. Early complications of interventional balloon catheterisation in infants and children. Br Heart J. 1991; 65:109–112.5. Cassidy SC, Schmidt KG, Van Hare GF, Stanger P, Teitel DF. Complications of pediatric cardiac catheterization: a 3-year study. J Am Coll Cardiol. 1992; 19:1285–1293.6. Yetman AT, Nykanen D, McCrindle BW, et al. Balloon angioplasty of recurrent coarctation: a 12-year review. J Am Coll Cardiol. 1997; 30:811–816.7. Zeevi B, Berant M, Fogelman R, Galit BM, Blieden LC. Acute complications in the current era of therapeutic cardiac catheterization for congenital heart disease. Cardiol Young. 1999; 9:266–272.8. Rhodes JF, Asnes JD, Blaufox AD, Sommer RJ. Impact of low body weight on frequency of pediatric cardiac catheterization complications. Am J Cardiol. 2000; 86:1275–1278.9. Mori Y, Nakazawa M, Yagihara T. Complications of pediatric cardiac catheterization and system of catheterization laboratories minimizing complications--a Japanese multicenter survey. J Cardiol. 2010; 56:183–188.10. West R, Ellis G, Brooks N. Joint Audit Committee of the British Cardiac Society and Royal College of Physicians of London. Complications of diagnostic cardiac catheterisation: results from a confidential inquiry into cardiac catheter complications. Heart. 2006; 92:810–814.11. Warnes CA, Liberthson R, Danielson GK, et al. Task force 1: the changing profile of congenital heart disease in adult life. J Am Coll Cardiol. 2001; 37:1170–1175.12. Vitiello R, McCrindle BW, Nykanen D, Freedom RM, Benson LN. Complications associated with pediatric cardiac catheterization. J Am Coll Cardiol. 1998; 32:1433–1440.13. Brotschi B, Hug MI, Kretschmar O, Rizzi M, Albisetti M. Incidence and predictors of cardiac catheterisation-related arterial thrombosis in children. Heart. 2015; 101:948–953.14. Krasemann T. Complications of cardiac catheterisation in children. Heart. 2015; 101:915.15. Luceri MJ, Tala JA, Weismann CG, Silva CT, Faustino EV. Prevalence of post-thrombotic syndrome after cardiac catheterization. Pediatr Blood Cancer. 2015; 62:1222–1227.16. Lin CH, Desai S, Nicolas R, et al. Sedation and anesthesia in pediatric and congenital cardiac catheterization: a prospective multicenter experience. Pediatr Cardiol. 2015; 36:1363–1375.17. Bobhate P, Guo L, Jain S, et al. Cardiac catheterization in children with pulmonary hypertensive vascular disease. Pediatr Cardiol. 2015; 36:873–879.18. Büsing KA, Schulte-Sasse C, Flüchter S, et al. Cerebral infarction: incidence and risk factors after diagnostic and interventional cardiac catheterization--prospective evaluation at diffusion-weighted MR imaging. Radiology. 2005; 235:177–183.19. De Bono D. The Joint Audit Committee of the British Cardiac Society and Royal College of Physicians of London. Complications of diagnostic cardiac catheterisation: results from 34,041 patients in the United Kingdom confidential enquiry into cardiac catheter complications. Br Heart J. 1993; 70:297–300.20. Glatz AC, Shah SS, McCarthy AL, et al. Prevalence of and risk factors for acute occlusive arterial injury following pediatric cardiac catheterization: a large single-center cohort study. Catheter Cardiovasc Interv. 2013; 82:454–462.21. Stone PA, Campbell JE, AbuRahma AF. Femoral pseudoaneurysms after percutaneous access. J Vasc Surg. 2014; 60:1359–1366.22. Zuckerman WA, Turner ME, Kerstein J, et al. Safety of cardiac catheterization at a center specializing in the care of patients with pulmonary arterial hypertension. Pulm Circ. 2013; 3:831–839.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A clinical study on cardiovascular disease of children taken cardiac catheterization and cineangiography
- Study of Neonatal Cardiac Catheterization for Over the Last 10 Years
- CT and MR Imaging Findings of Structural Heart Diseases Associated with Sudden Cardiac Death
- Digital subtraction angiography in cardiac disease
- Recent Trend of Increasing Proportion of Interventional Catheterization in Congenital Heart Disease