Korean Circ J.
2016 May;46(3):417-420. 10.4070/kcj.2016.46.3.417.
Endovascular Treatment of Multilevel Chronic Total Occlusion Using a Stent Puncture Technique in Buerger's Disease
- Affiliations
-
- 1Division of Cardiology, Yonsei University College of Medicine, Severance Cardiovascular Hospital, Yonsei University Health System, Seoul, Korea. cdhlyj@yuhs.ac
- KMID: 2344456
- DOI: http://doi.org/10.4070/kcj.2016.46.3.417
Abstract
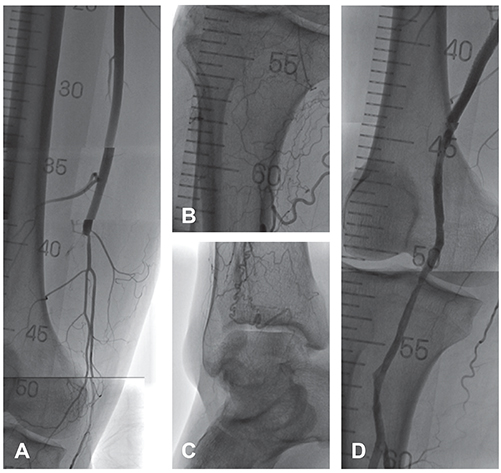
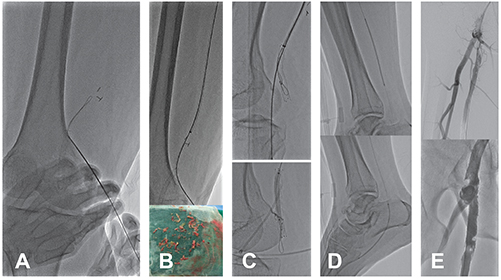
- We reported a patient with Buerger's disease who presented with critical limb ischemiawith prior recurrent occlusions after multiple surgical and endovascular treatments. Total occlusion of the whole native femoropopliteal and infrapopliteal arteries was observed. The femoropopliteal bypass graft, as well as a stent that was implanted in the mid-popliteal artery, were also occluded. Because of the lack of distal targets for bypass, surgical revascularization was not feasible; therefore, we decided to perform endovascular treatment. To overcome the limitation of vascular access, the previously implanted popliteal stent was directly punctured, and a guide wire was passed through the bypass graft. After the organized thrombus in the bypass graft was aspirated, further recanalization below the popliteal stent down to the plantar arteries was performed successfully. In conclusion, the stent puncture technique is a feasible and safe option for overcoming the limitations of vascular access in patients with multilevel occlusions.
Keyword
MeSH Terms
Figure
Reference
-
1. Olin JW. Thromboangiitis obliterans (Buerger's disease). N Engl J Med. 2000; 343:864–869.2. Sasaki S, Sakuma M, Kunihara T, Yasuda K. Distribution of arterial involvement in thromboangiitis obliterans (Buerger's disease): results of a study conducted by the Intractable Vasculitis Syndromes Research Group in Japan. Surg Today. 2000; 30:600–605.3. Graziani L, Morelli L, Parini F, et al. Clinical outcome after extended endovascular recanalization in Buerger's disease in 20 consecutive cases. Ann Vasc Surg. 2012; 26:387–395.4. Laird JR, Katzen BT, Scheinert D, et al. Nitinol stent implantation versus balloon angioplasty for lesions in the superficial femoral artery and proximal popliteal artery: twelve-month results from the RESILIENT randomized trial. Circ Cardiovasc Interv. 2010; 3:267–276.5. Schlager O, Dick P, Sabeti S, et al. Long-segment SFA stenting--the dark sides: in-stent restenosis, clinical deterioration, and stent fractures. J Endovasc Ther. 2005; 12:676–684.6. Del Conde I, Peña C. Buerger disease (thromboangiitis obliterans). Tech Vasc Interv Radiol. 2014; 17:234–240.7. Puechal X, Fiessinger JN. Thromboangiitis obliterans or Buerger's disease: challenges for the rheumatologist. Rheumatology (Oxford). 2007; 46:192–199.8. Cooper LT, Tse TS, Mikhail MA, McBane RD, Stanson AW, Ballman KV. Long-term survival and amputation risk in thromboangiitis obliterans (Buerger's disease). J Am Coll Cardiol. 2004; 44:2410–2411.9. Graziani L, Piaggesi A. Indications and clinical outcomes for below knee endovascular therapy: review article. Catheter Cardiovasc Interv. 2010; 75:433–443.10. Gandini R, Del Giudice C, Assako Ondo EP, Spano S, Stefanini M, Simonetti G. Stent puncture for recanalization of occluded superficial femoral artery stents. J Endovasc Ther. 2012; 19:30–33.11. Palena LM, Manzi M. Direct stent puncture technique for intraluminal stent recanalization in the superficial femoral and popliteal arteries in-stent occlusion: outcomes from a prospective clinical analysis of diabetics with critical limb ischemia. Cardiovasc Revasc Med. 2013; 14:203–206.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful Complex Endovascular Intervention for a Patient with Typical Buerger's Disease
- Endovascular Revascularization for the Obstruction after Patch Angioplasty in Buerger's Disease
- Complete Revascularization of Juxtarenal Aortic Occlusion by Endovascular Treatment and Adjunctive Anticoagulation
- A novel hybrid technique to treat flush mesenteric arterial occlusion in acute-on-chronic mesenteric ischemia
- Percutaneous Recanalization for Refractory Dialysis-related Subclavian Vein Obstruction: A Case with Needle Puncture