Korean J Ophthalmol.
2014 Oct;28(5):393-398. 10.3341/kjo.2014.28.5.393.
Augmentation of Filtering Blebs with Viscoelastics in Trabeculectomy
- Affiliations
-
- 1Department of Ophthalmology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. sungeye@gmail.com
- KMID: 2344263
- DOI: http://doi.org/10.3341/kjo.2014.28.5.393
Abstract
- PURPOSE
To evaluate the clinical outcome of viscoelastics (VE, sodium hyaluronate)-augmented trabeculectomy (VAT, 66 eyes) and conventional trabeculectomy (CT, 57 eyes) for glaucomatous eyes.
METHODS
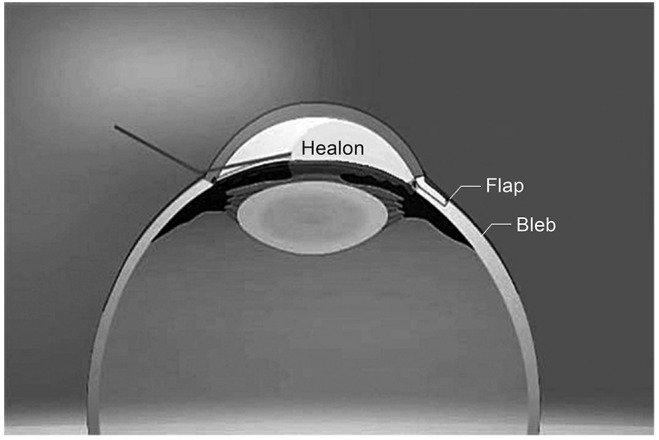
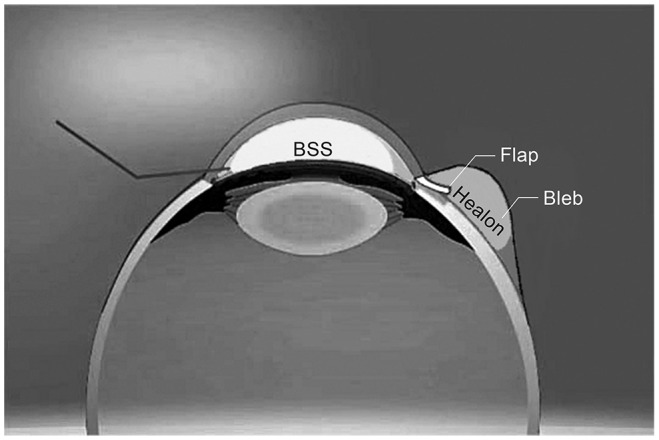
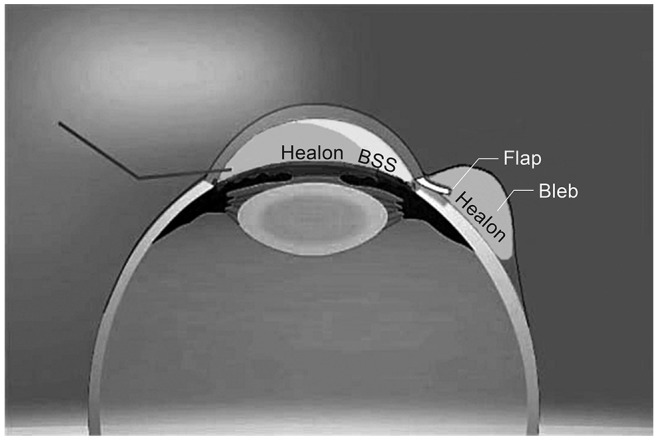
In the VAT group, half of the anterior chamber space was filled with VE via the paracentesis site at the end of CT and a balanced salt solution was injected into the anterior chamber. This procedure induced migration of VE from the anterior chamber into the bleb space; thus the bleb was elevated with underlying VE. Follow-up examinations were performed until 1 year after surgery. Success was defined as the attainment of an intraocular pressure (IOP) greater than 5 mmHg and less than 22 mmHg. If IOP was in the range of success without antiglaucoma medication, it was regarded as a complete success.
RESULTS
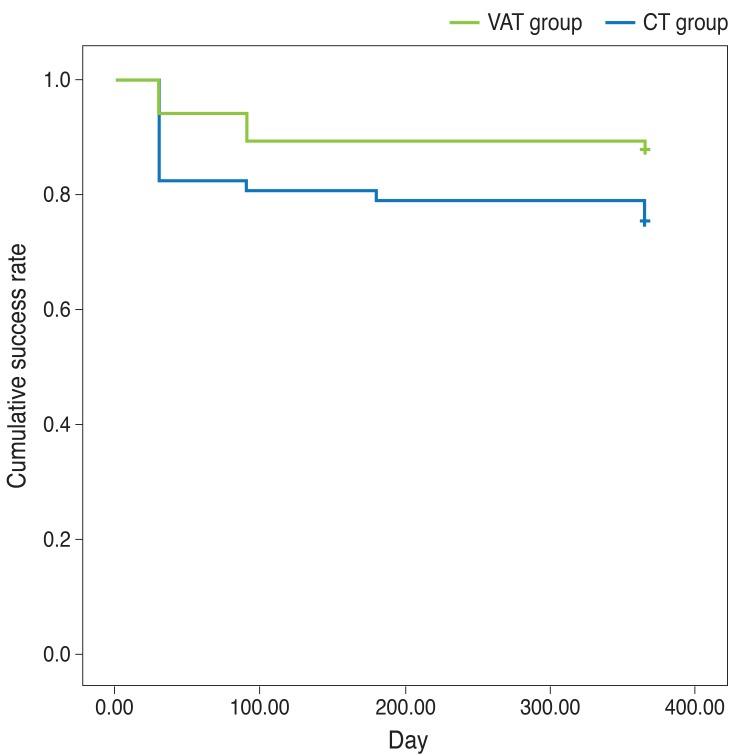
The mean postoperative IOP was significantly lower in the VAT group at postoperative 1 day, 1 week, and 1 month. The complete success rate was significantly higher in the VAT group (89%) than in the CT group (75%), though the qualified success rate was not different between the two groups. The number of IOP-lowering medications at postoperative 1 year was significantly higher in the CT group (1.30 ± 1.08 vs. 0.73 ± 0.98, p = 0.003). Among postoperative procedures, laser suture lysis was required less frequently in the VAT group (p < 0.001).
CONCLUSIONS
Placing VE within the bleb at the end of surgery may result in better IOP control and less need for IOP-lowering medication without any additional materials, cost, or time.
MeSH Terms
Figure
Reference
-
1. Azuara-Blanco A, Katz LJ. Dysfunctional filtering blebs. Surv Ophthalmol. 1998; 43:93–126. PMID: 9763136.
Article2. Stewart WC, Shields MB, Miller KN, et al. Early postoperative prognostic indicators following trabeculectomy. Ophthalmic Surg. 1991; 22:23–26. PMID: 2014106.
Article3. Allingham RR, Shields MB. Shields' textbook of glaucoma. 5th ed. Philadelphia: Lippincott Williams & Wilkins;2005. p. 565–595.4. Haynes WL, Alward WL. Control of intraocular pressure after trabeculectomy. Surv Ophthalmol. 1999; 43:345–355. PMID: 10025517.
Article5. Vijaya L, Manish P, Ronnie G, Shantha B. Management of complications in glaucoma surgery. Indian J Ophthalmol. 2011; 59(Suppl):S131–S140. PMID: 21150025.
Article6. Hau S, Barton K. Corneal complications of glaucoma surgery. Curr Opin Ophthalmol. 2009; 20:131–136. PMID: 19240546.
Article7. Fourman S. Management of cornea-lens touch after filtering surgery for glaucoma. Ophthalmology. 1990; 97:424–428. PMID: 2326021.
Article8. Shin DH. Management of flat anterior chamber with hypotonia after glaucoma surgery. Glaucoma. 1982; 4:193–197.9. Stewart RH, Kimbrough RL. A method of managing flat anterior chamber following trabeculectomy. Ophthalmic Surg. 1980; 11:382–383. PMID: 7402579.10. Kurtz S, Leibovitch I. Combined perfluoropropane gas and viscoelastic material injection for anterior chamber reformation following trabeculectomy. Br J Ophthalmol. 2002; 86:1225–1227. PMID: 12386073.
Article11. Geyer O, Segev E, Steinberg JM, Buckman G. Stabilization of post-trabeculectomy flat anterior chamber with Healon and sulfur hexafluoride. J Cataract Refract Surg. 2003; 29:2026–2028. PMID: 14604731.
Article12. Higashide T, Sugiyama K. Use of viscoelastic substance in ophthalmic surgery: focus on sodium hyaluronate. Clin Ophthalmol. 2008; 2:21–30. PMID: 19668386.13. Bowers D, Raybon RB, Wheeless CR Jr. Hyaluronic acid-carboxymethylcellulose film and perianastomotic adhesions in previously irradiated rats. Am J Obstet Gynecol. 1999; 181:1335–1337. PMID: 10601909.
Article14. Osada H, Minai M, Tsunoda I, et al. The effect of hyaluronic acid-carboxymethylcellulose in reducing adhesion reformation in rabbits. J Int Med Res. 1999; 27:292–296. PMID: 10726238.
Article15. Burns JW, Colt MJ, Burgees LS, Skinner KC. Preclinical evaluation of Seprafilm bioresorbable membrane. Eur J Surg Suppl. 1997; (577):40–48. PMID: 9076451.16. Ouaissi M, Gaujoux S, Veyrie N, et al. Post-operative adhesions after digestive surgery: their incidence and prevention: review of the literature. J Visc Surg. 2012; 149:e104–e114. PMID: 22261580.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Risk Factors for the Development of Thin-walled Blebs after Mitomycin C Trabeculectomy
- Two Cases of Bleb-Related Endophthalmitis after Trabeculectomy with Mitomycin C
- Needle Revision with and without Mitomycin C for the Teatment of Failed Filtering Blebs after Trabeculectomy
- Two Cases of Subconjunctival Bevacizumab Injection to Prevent Bleb Failure After Trabeculectomy
- Effect of Cataract Surgery through Clear Corneal Incision in Glaucomatous Eyes with Filtering Blebs