Korean J Urol.
2015 Sep;56(9):637-643. 10.4111/kju.2015.56.9.637.
Difference in the rate of rectal complications following prostate brachytherapy based on the prostate-rectum distance and the prostate longitudinal length among early prostate cancer patients
- Affiliations
-
- 1Department of Urology, CHA Bundang Medical Center, CHA University, Seongnam, Korea. dsparkmd@cha.ac.kr
- 2Department of Radiation Oncology, CHA Bundang Medical Center, CHA University, Seongnam, Korea.
- 3Department of Urology, Seoul National University Bundang Hospital, Seongnam, Korea.
- KMID: 2344102
- DOI: http://doi.org/10.4111/kju.2015.56.9.637
Abstract
- PURPOSE
To investigate the difference in rectal complications rate following prostate low dose rate (LDR) brachytherapy based on prostate-rectum distance and prostate longitudinal length among early prostate cancer patients.
MATERIALS AND METHODS
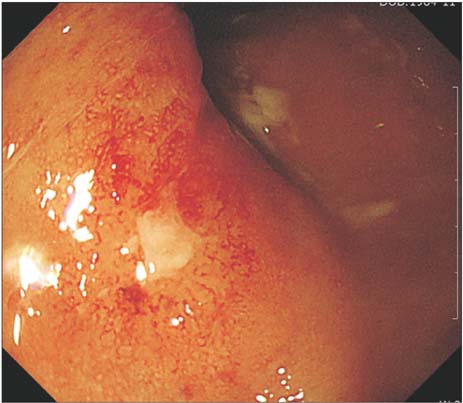
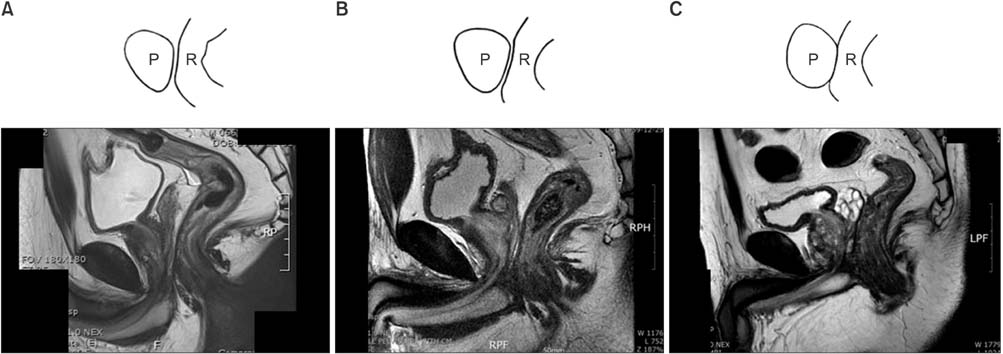
From March 2008 to February 2013, 245 prostate cancer patients with a Gleason score < or =7 were treated with 125-I LDR brachytherapy. Among them, 178 patients with prostate volume 20-35 mL and a follow-up period > or =6 months were evaluated for radiation proctitis. Magnetic resonance imaging (MRI) was performed for a prebrachytherapy evaluation, and prostate-rectum distance and prostate longitudinal length were measured. The radiation proctitis was confirmed and graded via colonoscopy based on the radiation therapy oncology group (RTOG) toxicity criteria.
RESULTS
Twenty-three patients received a colonoscopy for proctitis evaluation, and 12 were identified as grade 1 on the RTOG scale. Nine patients were diagnosed as grade 2 and 2 patients were grade 3. No patient developed grade 4 proctitis. The rectal-complication group had a mean prostate-rectum distance of 2.51+/-0.16 mm, while non-rectal-complication control group had 3.32+/-0.31 mm. The grade 1 proctitis patients had a mean prostate-rectum distance of 2.80+/-0.15 mm, which was significantly longer than 2.12+/-0.31 mm of grades 2 and 3 patient groups (p=0.045). All 11 patients of grades 2 and 3 had a prostate longitudinal length of 35.22+/-2.50 mm, which was longer than group 1, but the difference was not statistically significant (p=0.214).
CONCLUSIONS
As the prostate-rectum distance increased, fewer postimplantation rectal symptoms were observed. Patients with a shorter prostate-rectum distance in MRI should receive modified implantation techniques or radical prostatectomy.
Keyword
MeSH Terms
Figure
Reference
-
1. Ragde H, Elgamal AA, Snow PB, Brandt J, Bartolucci AA, Nadir BS, et al. Ten-year disease free survival after transperineal sonography-guided iodine-125 brachytherapy with or without 45-gray external beam irradiation in the treatment of patients with clinically localized, low to high Gleason grade prostate carcinoma. Cancer. 1998; 83:989–1001.2. Blasko JC, Grimm PD, Sylvester JE, Badiozamani KR, Hoak D, Cavanagh W. Palladium-103 brachytherapy for prostate carcinoma. Int J Radiat Oncol Biol Phys. 2000; 46:839–850.3. Frank SJ, Pisters LL, Davis J, Lee AK, Bassett R, Kuban DA. An assessment of quality of life following radical prostatectomy, high dose external beam radiation therapy and brachytherapy iodine implantation as monotherapies for localized prostate cancer. J Urol. 2007; 177:2151–2156.4. Wei JT, Dunn RL, Sandler HM, McLaughlin PW, Montie JE, Litwin MS, et al. Comprehensive comparison of health-related quality of life after contemporary therapies for localized prostate cancer. J Clin Oncol. 2002; 20:557–566.5. Kleinberg L, Wallner K, Roy J, Zelefsky M, Arterbery VE, Fuks Z, et al. Treatment-related symptoms during the first year following transperineal 125I prostate implantation. Int J Radiat Oncol Biol Phys. 1994; 28:985–990.6. Gelblum DY, Potters L. Rectal complications associated with transperineal interstitial brachytherapy for prostate cancer. Int J Radiat Oncol Biol Phys. 2000; 48:119–124.7. Wallner K, Blasko JC, Dattoli M. Prostate brachytherapy made complicated. 2nd ed. Seattle: Smart Medicine Press;2001.8. Wallner K, Roy J, Zelefsky M, Fuks Z, Harrison L. Short-term freedom from disease progression after I-125 prostate implantation. Int J Radiat Oncol Biol Phys. 1994; 30:405–409.9. Wallner K, Roy J, Harrison L. Tumor control and morbidity following transperineal iodine 125 implantation for stage T1/T2 prostatic carcinoma. J Clin Oncol. 1996; 14:449–453.10. Blasko JC, Ragde H, Cavanagh W, Sylvaster J, Grimm PD. Long term outcomes of external beam irradiation and I-125/Pd-103 brachytherapy boost for prostate cancer. Int J Radiat Oncol Biol Phys. 1996; 36:198.11. Critz FA, Levinson K, Williams WH, Holladay D, Holladay C, Griffin V. Prostate-specific antigen nadir of 0.5 ng/mL or less defines disease freedom for surgically staged men irradiated for prostate cancer. Urology. 1997; 49:668–672.12. Critz FA, Levinson AK, Williams WH, Holladay DA. Prostatespecific antigen nadir: the optimum level after irradiation for prostate cancer. J Clin Oncol. 1996; 14:2893–2900.13. Albert P, Zeitlin S, Raboy A, Lederman G. High dose combination radiotherapy in the treatment of carcinoma of the prostate - 410 consecutive patients. J Urol. 1997; 157:290.14. Beyer DC, Priestley JB Jr. Biochemical disease-free survival following 125I prostate implantation. Int J Radiat Oncol Biol Phys. 1997; 37:559–563.15. Stone NN, Stock RG. Brachytherapy for prostate cancer: realtime three-dimensional interactive seed implantation. Tech Urol. 1995; 1:72–80.16. Stock RG, Stone NN, DeWyngaert JK, Lavagnini P, Unger PD. Prostate specific antigen findings and biopsy results following interactive ultrasound guided transperineal brachytherapy for early stage prostate carcinoma. Cancer. 1996; 77:2386–2392.17. Wallner K, Roy J, Harrison L. Dosimetry guidelines to minimize urethral and rectal morbidity following transperineal I-125 prostate brachytherapy. Int J Radiat Oncol Biol Phys. 1995; 32:465–471.18. Kaye KW, Olson DJ, Payne JT. Detailed preliminary analysis of 125iodine implantation for localized prostate cancer using percutaneous approach. J Urol. 1995; 153(3 Pt 2):1020–1025.19. Phan J, Swanson DA, Levy LB, Kudchadker RJ, Bruno TL, Frank SJ. Late rectal complications after prostate brachytherapy for localized prostate cancer: incidence and management. Cancer. 2009; 115:1827–1839.20. Benoit RM, Naslund MJ, Cohen JK. Complications after prostate brachytherapy in the Medicare population. Urology. 2000; 55:91–96.21. Dattoli M, Wallner K, Sorace R, Koval J, Cash J, Acosta R, et al. 103Pd brachytherapy and external beam irradiation for clinically localized, high-risk prostatic carcinoma. Int J Radiat Oncol Biol Phys. 1996; 35:875–879.22. Lee WR, McQuellon RP, Case LD, deGuzman AF, McCullough DL. Early quality of life assessment in men treated with permanent source interstitial brachytherapy for clinically localized prostate cancer. J Urol. 1999; 162:403–406.23. Brandeis JM, Litwin MS, Burnison CM, Reiter RE. Quality of life outcomes after brachytherapy for early stage prostate cancer. J Urol. 2000; 163:851–857.24. Li S, Boyer A, Lu Y, Chen GT. Analysis of the dose-surface histogram and dose-wall histogram for the rectum and bladder. Med Phys. 1997; 24:1107–1116.25. Snyder KM, Stock RG, Hong SM, Lo YC, Stone NN. Defining the risk of developing grade 2 proctitis following 125I prostate brachytherapy using a rectal dose-volume histogram analysis. Int J Radiat Oncol Biol Phys. 2001; 50:335–341.26. Waterman FM, Dicker AP. Probability of late rectal morbidity in 125I prostate brachytherapy. Int J Radiat Oncol Biol Phys. 2003; 55:342–353.27. Merrick GS, Butler WM, Dorsey AT, Lief JH, Walbert HL, Blatt HJ. Rectal dosimetric analysis following prostate brachytherapy. Int J Radiat Oncol Biol Phys. 1999; 43:1021–1027.28. Kouloulias V, Kalogeropoulos T, Platoni K, Georgakopoulos J, Matsopoulos G, Chaldeopoulos D, et al. Feasibility and radiation induced toxicity regarding the first application of transperineal implementation of biocompatible balloon for high dose radiotherapy in patients with prostate carcinoma. Radiat Oncol. 2013; 8:82.29. Prada PJ, Fernandez J, Martinez AA, de la Rua A, Gonzalez JM, Fernandez JM, et al. Transperineal injection of hyaluronic acid in anterior perirectal fat to decrease rectal toxicity from radiation delivered with intensity modulated brachytherapy or EBRT for prostate cancer patients. Int J Radiat Oncol Biol Phys. 2007; 69:95–102.30. Davis BJ, Horwitz EM, Lee WR, Crook JM, Stock RG, Merrick GS, et al. American Brachytherapy Society consensus guidelines for transrectal ultrasound-guided permanent prostate brachytherapy. Brachytherapy. 2012; 11:6–19.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The prostate specific antigen in detection of the prostate cancer
- The Diagnostic Value of Prostate-specific Antigen and the of Routine Laboratory Examination for Early Detection
- Radical Prostatectomy
- Radiation Dose Calculation in the Surrounding Organs during Brachytherapy of Prostate Cancer
- Prostate Cancer in Young Man